Trauma and Burns
Approximately 75% of the hospital mortality from high-energy trauma (motor vehicle accidents falls, gunshot and stab wounds) occurs within 48 hours after admission, most commonly from central nervous system (CNS), thoracic, abdominal, retroperitoneal, or vascular injuries (Capan LM, Miller SM, Gingrich K. Trauma and burns. In: Barash PG, Cullen BF, Stoelting RK, Cahalan MK, Ortega R, Stock MC, eds. Clinical Anesthesia. Philadelphia: Lippincott Williams & Wilkins; 2013:1490–1534). CNS injury and hemorrhage are the most common causes of early trauma mortality. Nearly one third of these patients die within the first 4 hours after admission, representing the majority of operating room (OR) trauma deaths. Of the hospital deaths, 5% to 10% occur between the third and seventh days of admission, usually from CNS injuries, and the rest occur in subsequent weeks, most commonly as a result of multiorgan failure.
I. Initial Evaluation and Resuscitation
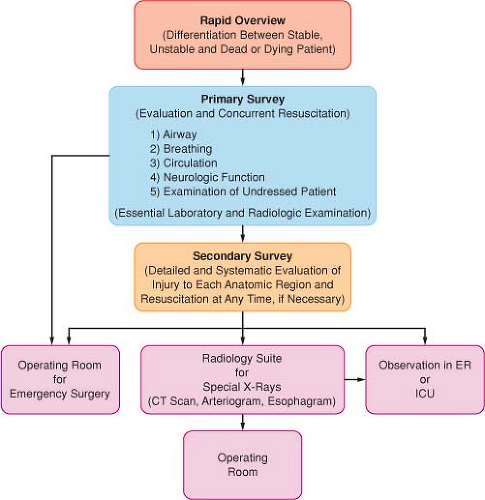
The general approach to evaluation of an acute trauma victim has three sequential components: rapid overview, primary survey, and secondary survey (Fig. 52-1).
Airway Evaluation and Intervention. Airway evaluation involves the diagnosis of any trauma to the airway or surrounding tissues, recognition and anticipation of the respiratory consequences of these injuries, and prediction of the potential for exacerbation of these or other injuries by any contemplated airway management maneuvers.
Airway Obstruction. Airway obstruction is a frequent cause of asphyxia and may result from posteriorly displaced or lacerated pharyngeal soft tissues; cervical or mediastinal hematoma; bleeding, secretions, or foreign bodies within the airway; and/or displaced bone or cartilage fragments.
Full Stomach. A full stomach is a background condition in acute trauma. (Urgency of securing the airway often does not permit adequate time for pharmacologic measures to reduce gastric volume and acidity.) After locating the cricothyroid membrane and denitrogenating the lungs, a rapid sequence induction may be used to permit securing the airway with direct laryngoscopy or, if necessary, with immediate cricothyroidotomy.
Head, Open-Eye, and Contained Major Vessel Injuries
These patients require deep anesthesia and profound muscle relaxation before airway manipulation (helps prevent hypertension, coughing, and bucking and thereby minimizes intracranial, intraocular, or intravascular pressure elevation, which can result in herniation
of the brain, extrusion of eye contents, or dislodgment of a hemostatic clot from an injured vessel).
The preferred anesthetic sequence in patients who are not hemodynamically compromised includes preoxygenation and opioid loading followed by relatively large doses of an intravenous (IV) anesthetic and muscle relaxant (prevent fasciculations produced by succinylcholine).
II. Cervical Spine Injury
Overall, 2% to 4% of blunt trauma patients have cervical spine (C-spine) injuries (most often motor vehicle accidents), of which 7% to 15% are unstable.
Initial Evaluation. Accurate and timely evaluation is important because 2% to 10% of patients with blunt trauma–induced C-spine injury develop new or worsening neurologic deficits after admission.
Clearance of the neck at the earliest possible time after airway management should be performed to minimize the complications associated with the collar such as pressure ulceration, intracranial pressure (ICP) elevation in head-injured patients, compromised central venous access, and airway management challenges if reintubation is needed.
Routine computed tomography (CT) in addition to clinical evaluation is recommended to rule out C-spine injury in major trauma victims.
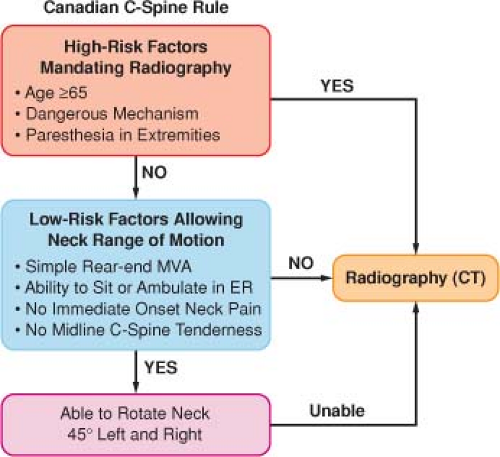
The Canadian C-spine rule for radiography after trauma is a tool designed to identify low-risk patients (Fig. 52-2).
Airway Management. Almost all airway maneuvers, including jaw thrust, chin lift, head tilt, and oral airway placement, result in some degree of C-spine movement. To secure the airway with direct laryngoscopy, manual in-line stabilization (MILS) of the neck is the standard care of these patients in the acute stage. A hard cervical collar alone, which is routinely placed, does not provide absolute protection, especially for rotational movements of the neck.
MILS is best accomplished by having two operators in addition to the physician who is actually managing the airway. The first operator stabilizes and aligns the head in neutral position without applying cephalad traction, and the second stabilizes both shoulders by holding them against the table or stretcher.
In the presence of MILS, the glottic view may be suboptimal in 10% to 15% of patients during direct laryngoscopy because of limitation of neck extension.
The more the restriction of the glottic view during direct laryngoscopy, the greater the pressure on the tongue, the spine, and the unstable segment with potential displacement of the unstable fragment.
During various phases of direct laryngoscopy and intubation, the pressures exerted on the tongue and indirectly to the spine are greater with MILS than without MILS. Nevertheless, it cannot be concluded airway management without MILS is associated with a favorable spinal cord outcome. However, it is reasonable to allow some relaxation of the MILS to improve the glottic view when visualization of the larynx is restricted.
III. Direct Airway Injuries
Direct airway damage can occur anywhere between the nasopharynx and the bronchi.
Maxillofacial Injuries. In addition to soft tissue edema of the pharynx and peripharyngeal hematoma, blood or debris in the oropharynx may be responsible for partial or complete airway obstruction in the acute stage of these injuries.
Serious airway compromise may develop within a few hours in up to 50% of patients with major penetrating facial injuries or multiple trauma as a result of progressive inflammation or edema resulting from liberal administration of fluids.
Fracture-induced encroachment on the airway or limitation of mandibular movement, pain, and trismus may limit mouth opening. (Fentanyl in titrated doses of up to 2–4 μg/kg over a period of 10–20 minutes may produce an improvement in the patient’s ability to open the mouth if mechanical limitation is not present.)
Most patients with isolated facial injuries do not require emergency tracheal intubation. Surgery may be delayed for as long as 1 week with no adverse effect on the repair. Alternatively, tracheostomy may be indicated as an emergency procedure.
Cervical Airway Injuries. Clinical signs such as air escape, hemoptysis, and coughing are present in almost all patients with penetrating injuries, facilitating the diagnosis. In contrast, the patient with major blunt laryngotracheal damage may asymptomatic or not recognized because suggestive signs and symptoms are missed in the initial evaluation (hoarseness, muffled voice, dyspnea, stridor, dysphagia)
A CT scan of the neck provides valuable information and should be performed before any airway intervention in all stable patients.
Laryngeal damage precludes cricothyroidotomy. Tracheostomy should be performed with extreme caution because up to 70% of patients with blunt laryngeal injuries may have an associated C-spine injury.
Thoracic Airway Injuries. Blunt injury usually involves the posterior membranous portion of the trachea and the mainstem bronchi, usually within approximately 3 cm of the carina.
In patients intubated without the suspicion of a tracheal injury, difficulty in obtaining a seal around the endotracheal tube or the presence on a chest radiograph of a large radiolucent area in the trachea corresponding to the cuff suggests a perforated airway.
Anesthetics, and especially muscle relaxants, may produce irreversible obstruction, presumably because of relaxation of structures that maintain the airway patent in the awake patient. Airway loss may also occur during attempts at awake intubation.
IV. Management of Breathing Abnormalities
Of the several causes that may alter respiration after trauma, tension pneumothorax, flail chest, and open pneumothorax are life threatening.
Although cyanosis, tachypnea, hypotension, neck vein distention, tracheal deviation, and diminished breath sounds on the affected side are the classic signs of tension pneumothorax, neck vein distention may be absent in hypovolemic patients, and tracheal deviation may be difficult to appreciate.
The definitive diagnosis is made by CT scanning.
In hypoxemic and hypotensive patients, immediate insertion of a 14-gauge angiocatheter through the fourth intercostal space in the midaxillary line or, at times, through the second intercostal space at the midclavicular line is essential. (There is no time for radiologic confirmation in this setting.)
A flail chest results from fractures of more than two sites of at least three adjacent ribs or rib fractures with associated costochondral separation or sternal fracture.
It often develops over a 3- to 6-hour period, causing gradual deterioration of the chest radiograph and arterial blood gases (ABGs).
Effective pain relief by itself can improve respiratory function and often avoid the need for mechanical ventilation (continuous epidural analgesia).
Ventilation with low tidal volumes (6–8 mL/kg) and moderate positive end-expiratory pressure (PEEP) producing low inspiratory alveolar or plateau pressures appears to be the best pattern to prevent deterioration of hemodynamics and decrease the likelihood of acute respiratory distress syndrome (ARDS).
Systemic air embolism occurs mainly after penetrating lung trauma and blast injuries or less frequently after blunt thoracic trauma that produces lacerations of both distal air passages and pulmonary veins. (Positive-pressure ventilation after tracheal intubation may then result in entrainment of air into the systemic circulation.)
Respiratory maneuvers that minimize or prevent air entry into the systemic circulation include isolating and collapsing the lacerated lung by means of a double-lumen tube or ventilation with the lowest possible tidal volumes via a single-lumen tube.
Transesophageal echocardiography (TEE) of the left side of the heart may permit visualization of air bubbles and their disappearance with therapeutic maneuvers.
V. Management of Shock
Hemorrhage is the most common cause of traumatic hypotension and shock and is, after head injury, the second most common cause of death after trauma (Table 52-1).
Patients with significant intra-abdominal fluid recognized with these tests and hemodynamic instability require immediate surgical intervention.
Those who are suspected to have occult abdominal bleeding based on a high-risk mechanism of injury but who are hemodynamically stable must undergo further evaluation with CT.
Clinical assessment using hemodynamic data is based on a few relatively insensitive and nonspecific clinical signs. (Tachycardia as an index of hypovolemia may be absent in up to 30% of hypotensive trauma patients because of increased vagal tone.)
Although traditional vital signs are relatively unreliable for recognizing life-threatening shock, heart rate, systemic blood pressure, pulse pressure, respiratory rate, urine output, and mental status are still used as early clinical indicators of the severity of hemorrhagic shock (Table 52-2).
The response to initial fluid resuscitation in the form of lactated Ringer’s solution (LRS) or normal saline solution of about 2 L or 20 mL/kg in children over a period of 15 to 30 minutes may permit estimation of the severity of hemorrhage (Table 52-3).
Crystalloids are used in the vast majority of trauma centers for initial resuscitation. (There is no difference in the mortality rate between patients receiving crystalloids and those receiving colloids.) Hydroxyethyl starch solutions (maximum, 20 mL/kg) should probably be given priority over albumin solutions. (Possible deleterious effects of colloids have mostly been associated with albumin.)
Table 52-2 Advanced Trauma Life Support Classification of Hemorrhagic Shock*
Class I
Class II
Class III
Class IV
Blood loss (mL)
≤750
750–1,500
1,500–2,000
≥2,000
Blood loss (% blood volume)
≤15
15–30
30–40
≥40
Pulse rate (beats/min)
<100
>100
>120
≥140
Blood pressure
Normal
Normal
Decreased
Decreased
Pulse pressure
Normal or increased
Decreased
Decreased
Decreased
Respiratory rate (breaths/min)
14–20
20–30
30–40
>35
Urine output (mL/hr)
≥30
20–30
5–15
Negligible
Mental status
Slightly anxious
Mildly anxious
Anxious and confused
Confused, lethargic
Fluid replacement (3:1 rule)
Crystalloid†
Crystalloid
Crystalloid + blood
Crystalloid + blood
*For a 70-kg male patient based on initial presentation.
†The 3:1 rule is based on empiric observation that most patients require 300 mL of balanced electrolyte solution for each 100 mL of blood loss. Without other clinical and monitoring parameters, this guideline may result in excessive or inadequate fluid resuscitation.
Adapted with permission from American College of Surgeons, Committee on Trauma: Shock, Advanced Trauma Life Support Student Course Manual. Edited by the American College of Surgeons, 8th ed. Chicago: American College of Surgeons; 2008:55–71.
Some of the proven markers of organ perfusion can be used during early management to set the goals of resuscitation. Of these, the base deficit and blood lactate level are the most useful and practical tools during all phases of shock, including the earliest.
Base deficit is considered a better prognostic marker than the arterial pH. (Normalization of the base deficit is one of the end points of resuscitation.)
Elevation of the blood lactate level is less specific than base deficit as a marker of tissue hypoxia. Nevertheless, in most trauma victims, an elevated lactate level correlates with other signs of hypoperfusion, rendering it an
important marker of dysoxia and an end point of resuscitation.
Table 52-3 Response to Initial Fluid Administration*
Rapid Response
Transient Response
Minimal or No Response
Vital signs
Return to normal
Transient improvement, recurrence of decreased blood pressure, and increased heart rate
Remain abnormal
Estimated blood loss
Minimal (10%–20%)
Moderate and ongoing (20%–40%)
Severe (>40%)
Need for more crystalloid
Low
High
High
Need for blood
Low
Moderate to high
Immediate
Blood preparation
Type and crossmatch
Type specific
Emergency blood release
Need for operative intervention
Possible
Likely
Highly likely
Early presence of surgeon
Yes
Yes
Yes
*2,000 mL of isotonic solution in adults; 20 mL/kg bolus of lactated Ringer’s solution in children.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree