Fig. 11.1
Left indirect inguinal hernia

Fig. 11.2
Left direct inguinal hernia
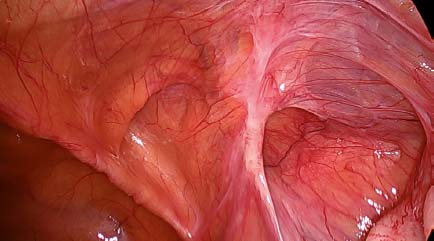
Fig. 11.3
Mixed hernia (pantaloon) on the right side
11.3.2 11.3.2 Dissection
The preperitoneal space is entered through a planned incision of the visceral peritoneum way above the visible hernia defect not tailored to hernia type and size (Figs. 11.4 and 11.5). The complex preperitoneal anatomy is best described by Sakurai [8, 9]. Peeling of the visceral leaf from the parietal leaf (the latter protecting the underlying lower epigastric vessels in the form of an “endoabdominal” fascia) starts laterally in a fairly avascular plane supported by the “pneumodissection” of CO2 gas under a pressure of 12 mmHg. We enter the space of Bogros (Fig. 11.6).

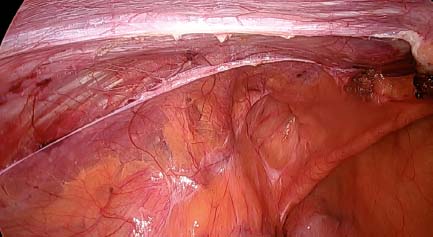
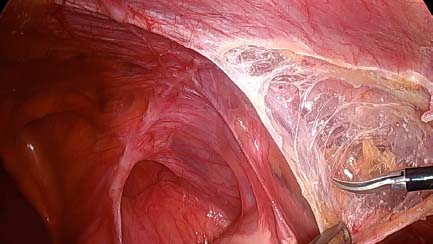

Fig. 11.4
Peritoneal incision above the defect on the right side
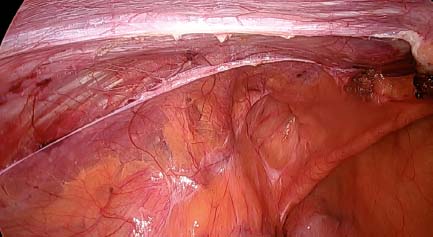
Fig. 11.5
Peritoneal incision above the direct defect on the left
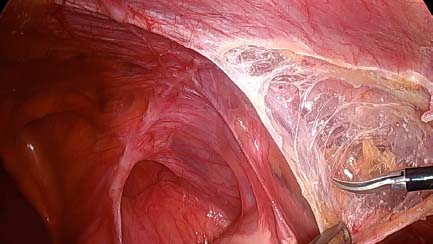
Fig. 11.6
Entering the space of Bogros on the right
Crossing the epigastric vessels in a medial direction, the endoabdominal fascia may continue to be a thin barrier which has to be entered to reach another spider-web-like compartment — the space of Retzius. These two anatomical spaces are not a continuation of each other, because they are not on the same level [9]. Further dissection deeper and medially finds Cooper’s ligament and the superior pubic arch (Fig. 11.7) up to the landmark of the symphysis pubis. The dissection 1–2 cm beyond the midline is the medial margin of the so-called “landing zone”. Caudally and laterally to the origin of the epigastric vessels and the inner inguinal ring, the figure of “A” is encountered (Figs. 11.8 and 11.9). The medial arm is the vas deferens complex and the lateral one the spermatic vessels. This region is often called the “triangle of doom” (because of the underlying external iliac vessels) (Fig. 11.10). Medial to the spermatic cord, a vascular anomaly of the arterial or venous corona mortis (or both) anastomosis between the iliac and the obturator vessels can be found in about 20% of the population. The femoral canal is encountered between the iliopubic tract, Cooper’s ligament and the external iliac vein. Lateral to the origin of the epigastric vessels the top of figure of “A” enters the inguinal canal. Laterally to the spermatic vessels a fat pad covers some nerves of the lumbar plexus (the genitofemoral nerve, the lateral cutaneous femoris and the femoral nerve) (Figs. 11.11 and 11.12). This area is called the triangle of pain. A very thin tissue layer covers both triangles and protects the fragile underlying structures in the form of the spermatic fascia. The dissection plane between the visceral and parietal peritoneal leaf facilitates the recognition and preservation of the spermatic fascia, which lowers the risk of postoperative nerve irritation or chronic pain. This gesture is easier to be accomplished in TAPP rather than in TEP, thanks to the preexisting working space and fearless dissection of the visceral leaf. In the case of dissectional insecurity, the TAPP technique allows the immediate view of the intraperitoneal structures behind the flap thereby avoiding possible sectional or thermal damage. After retraction of all hernia sacs and preperitoneal fat (Figs. 11.7 and 11.13) the presence of a cord lipoma has to be excluded. Substantial lipomas should be removed out of the inguinal canal because they are or may become symptomatic (Fig. 11.14). In large direct hernias, the remaining defect after retraction of the preperitoneal fat leaves a dead space behind. This predisposes to seroma formation and represents a risk factor for potential mesh dislocation. The attenuated transversalis fascia can be inverted and fixed with a suture or endo-loop in order to reduce this risk. The indirect sac should be retracted completely out the inguinal canal whenever possible. This sometimes difficult maneuver is safer after identification and dissection of the spermatic vessels.
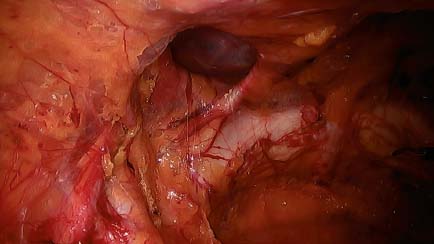
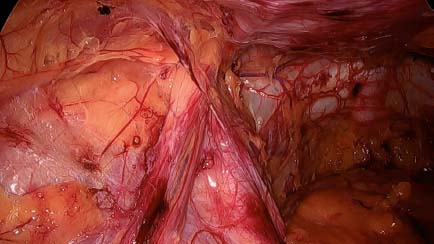
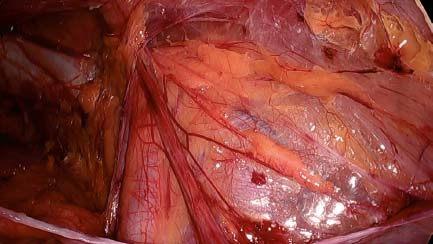
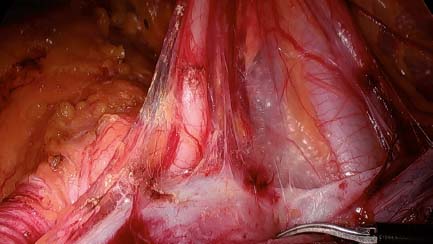
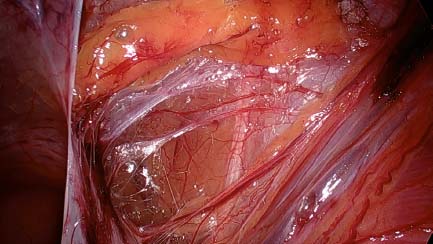
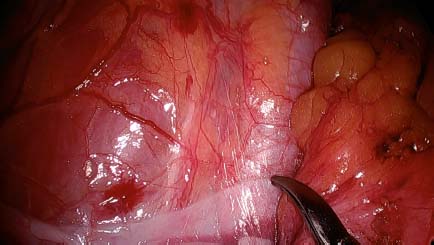
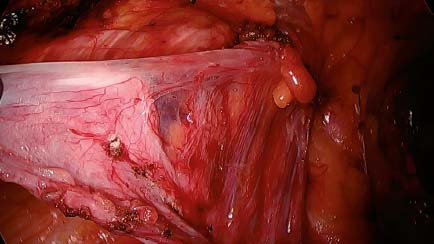
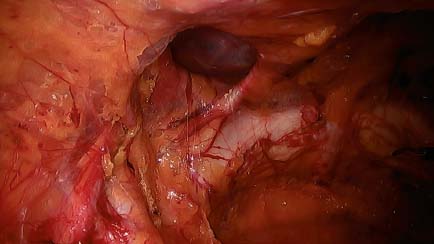
Fig. 11.7
Left direct hernia dissected
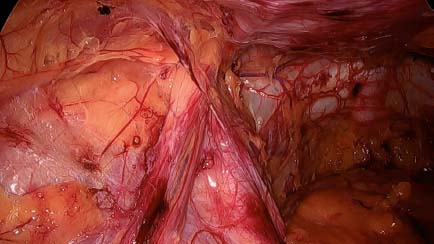
Fig. 11.8
Left figure of “A”: triangle of doom
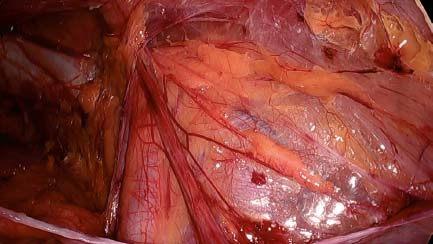
Fig. 11.9
Preserved spermatic fascia over triangle of pain on the right
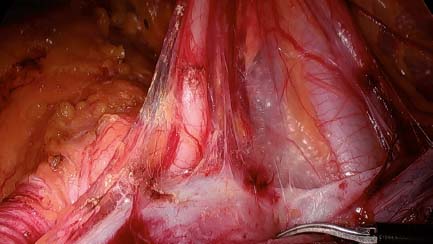
Fig. 11.10
Delicate dissection in triangle of doom on the right, vas deferens
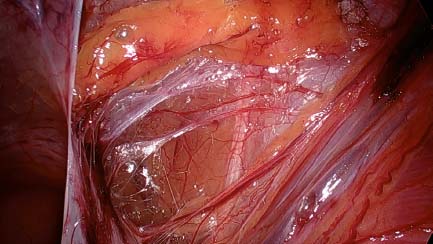
Fig. 11.11
N. cutaneus femoris lateralis on the left
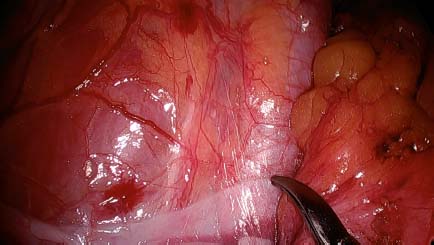
Fig. 11.12
Genitofemoral nerve on the left
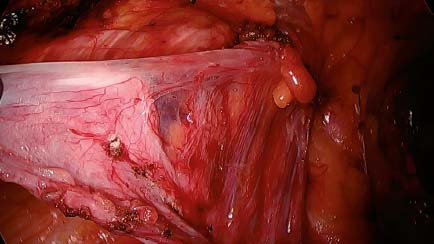
Fig. 11.13




Dissection of indirect sac on the left side
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






