CHAPTER 32 TRACHEAL, LARYNGEAL, AND OROPHARYNGEAL INJURIES
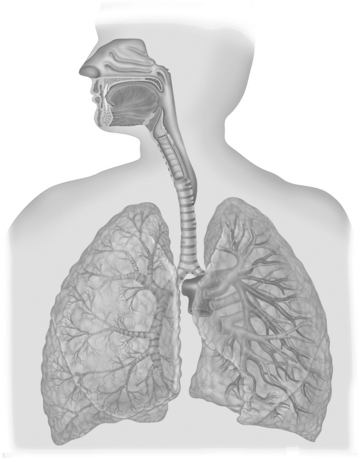
Structural mobility and elasticity are characteristics of the upper airway that make injury to these structures infrequent. Skeletal protection is also provided anteriorly by the mandible and sternum and posteriorly by the bony spinal column1 (Figure 1). Upper airway injuries are identified in only 0.03% of patients admitted to major trauma centers. These injuries are frequently lethal, which explains their higher reported occurrence in autopsy series.2,3 Penetrating mechanisms of injury are more common than blunt mechanisms of injury,1,2,4 the true incidence of which is unknown.1,5 Twenty-one percent of patients with upper airway injuries die within the first 2 hours after hospitalization.6 The diagnosis is often delayed in patients without immediate life-threatening upper airway trauma.6,7 Such delays often result in serious late complications.8,9 Limited experience in nonoperative and operative management of airway injuries has led to a wide variety of recommendations that may be considered under various clinical scenarios. For unstable, immediate life-threatening upper airway injuries, rapid airway control by any available means is essential for patient survival. Most authors agree that tracheal intubation through an open wound that communicates with the tracheobronchial tree is appropriate.1 Stable patients may benefit from bronchoscopic-guided tracheal intubation distal to the injury site, and blind endotracheal tube placement is almost always a poor choice for airway control.10 Airway injuries are always challenging to even the most experienced surgeon since traditional approaches to airway control are often contraindicated.
ANATOMY OF UPPER AIRWAY
Pharynx
Surgical Anatomy
The pharynx consists of the following elements:
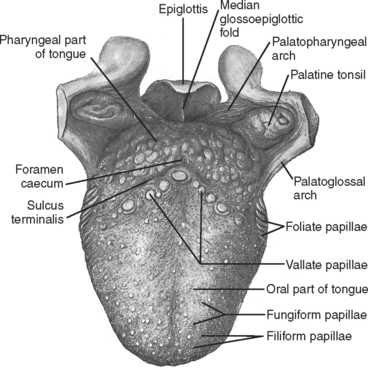
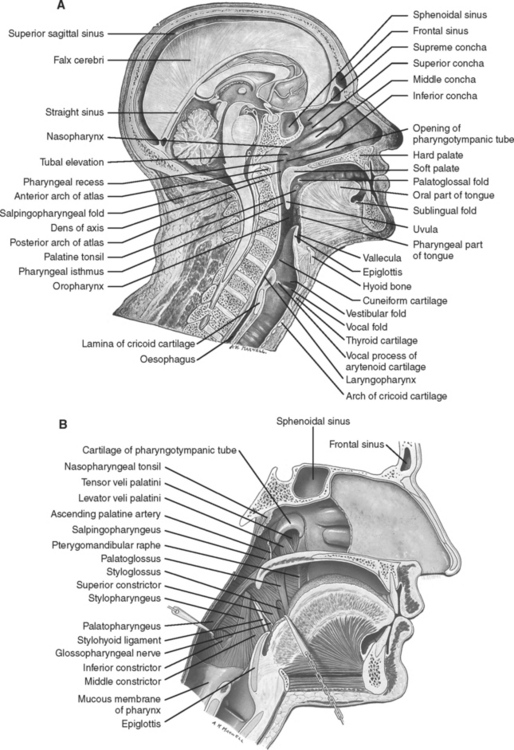
Figure 2 Contents of the oropharynx.
(From Gray’s Anatomy, 39th ed. St. Louis, Churchill Livingstone/Mosby, 2004, figure 33.4, with permission.)
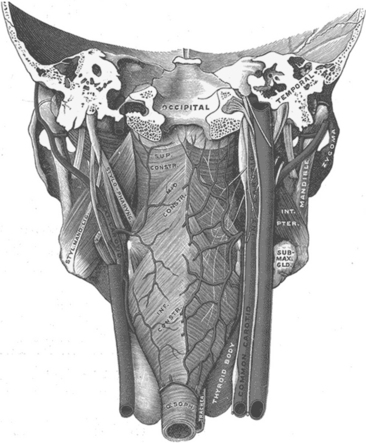
(Adapted from Gray H: Anatomy of the Human Body. Philadelphia, Lea & Febiger, 1918. Available at www.bartleby.com/107/.)
PHARYNGEAL INJURY
Incidence
Isolated blunt pharyngeal injury is exceedingly rare. It is more often associated with concomitant cervical facial trauma. Penetrating pharyngeal injury occurs more commonly in the pediatric population from lacerations caused by intraoral foreign bodies.11
Mechanism of Injury
Pharyngeal trauma may occur from foreign body ingestion, blunt or penetrating trauma, or following laryngoscopy or other endoscopic procedures.12–15
Diagnosis
The initial clinical scenario varies. Patients with nonlethal injuries commonly present with dysphagia and odynophagia. Patients with more severe injuries may present with aphonia, dyspnea, hemoptysis, and severe acute respiratory failure that may rapidly lead to asphyxia if not treated.16 Injuries to the esophagus and pharynx are difficult to diagnose and may be missed during the management of other immediate life-threatening injuries. Oral bleeding, drooling, and subcutaneous emphysema all suggest upper digestive tract or airway injury.16 When possible, careful examination of the oropharynx and hypopharynx should be performed at the bedside.
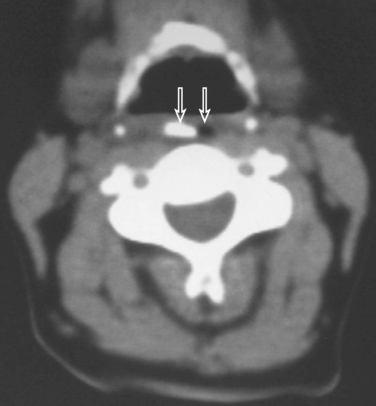
Lateral views of the neck and cervical CT scan may identify soft tissue air (Figures 5 and 6). A nonionic contrast-enhanced esophagram and/or esophagoscopy are indicated if injury is clinically suspected.17 Contrast leak may be revealed on esophagram (see Figure 5).

Figure 5 Retropharyngeal air (black arrow) as seen on a lateral cervical spine radiograph/esophagogram.
LARYNX
Surgical Anatomy
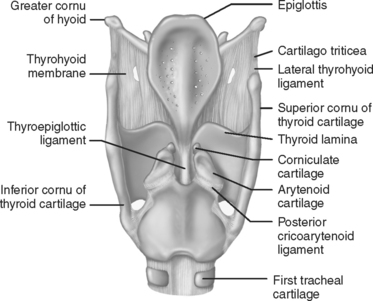
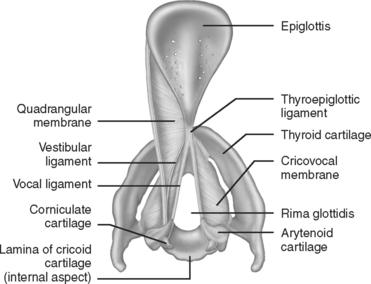
The larynx is composed of the following elements:
Laryngeal Injury
Incidence
Laryngeal and cervical tracheal injuries account for less than 1% of trauma cases seen in most major trauma centers.2,17 These injuries are rare compared to the total number of injuries that occur to the head and neck area. Experience in managing laryngeal trauma is limited because of these small numbers. External laryngeal trauma occurs in 1/30,000 emergency room visits.18,19 The rare nature of laryngeal injuries is a consequence of multiple factors, including protection by the mandible and sternum, delayed or missed diagnoses of minor laryngeal injuries in major multitrauma victims, and patient mortality at the scene from airway loss and asphyxiation.20
Although rare, initial management of laryngeal injuries affects the immediate probability of patient survival and long-term quality of life. The larynx is a well-protected structure that is both anatomically and functionally complex. Blunt and penetrating laryngeal injuries may cause chronic problems with aspiration, phonation, and respiration.20
Mechanism of Injury
The mechanisms of laryngeal injury can be divided into blunt trauma (including crushing, clothesline, and strangulation injuries) and penetrating trauma. The degree and location of blunt laryngotracheal trauma are multifactorial. Sheely et al.21 found that 88% of injuries occurred above the fourth tracheal ring. Penetrating injury can occur at any level of the cervical trachea.
Diagnosis
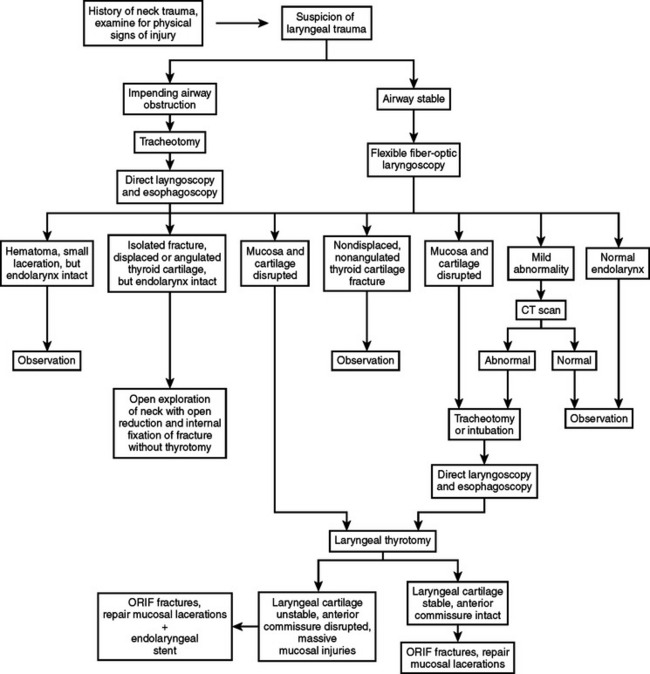
Adherence to the essential principles of initial assessment delineated in the Advanced Trauma Life Support (ATLS)® Manual is recommended. The ABCs (airway, breathing, circulation), concomitant resuscitation of the trauma victim, and a thorough secondary survey are essential for optimal management of airway injuries.22 Early recognition of these injuries requires a high index of suspicion based on mechanism of injury and findings identified during cervical and chest examination. Clinical signs and symptoms may include stridor, acute respiratory distress, cervical tenderness, subcutaneous emphysema, and cervical hematoma when associated with major vascular injury.23 Hemoptysis suggests that an intralaryngeal laceration may be present.23 This is more common with penetrating injury, but also occurs from blunt laryngeal trauma with an associated laryngeal cartilage fracture.23 Diagnostic procedures such as direct laryngoscopy, fiber-optic bronchoscopy, and cervical helical, contrast-enhanced multidetector (16 slices minimum) computed tomography (CT) with angiography are all beneficial if the patient’s clinical condition permits performing these tests.17,24 A sample algorithm for the evaluation of patients with laryngeal injuries is described (Figure 8).
TRACHEA
Surgical Anatomy
The trachea is a cartilaginous and membranous tube. It extends from the lower part of the larynx, at the level of the sixth cervical vertebra, to the upper border of the fifth thoracic vertebra. There it divides into the two main stem bronchi. The trachea is an ellipsoid cylinder that is flattened posteriorly. The average adult trachea measures about 11 cm in length with a diameter that varies from 2 to 2.5 cm. The pediatric trachea is smaller, more deeply placed, and more mobile. Half of the trachea lies within the neck and half is intrathoracic. The anterior two thirds of the trachea are composed of 18 to 22 “U”-shaped cartilages. The membranous posterior wall of the trachea is in apposition with the anterior wall of the esophagus. The bifurcation of the mainstem bronchi forms the carina at approximately the fourth to fifth thoracic vertebrae. The trachea is supplied with blood by the inferior thyroid arteries. Similarly named veins form the thyroid venous plexus. Tracheal innervation is derived from the vagus nerves, the recurrent laryngeal nerves, and from the sympathetic chain. The recurrent laryngeal nerve lies within the tracheoesophageal groove formed by the close proximity of the lateral aspects of the trachea and the esophagus (Figures 9, 10, and 11).
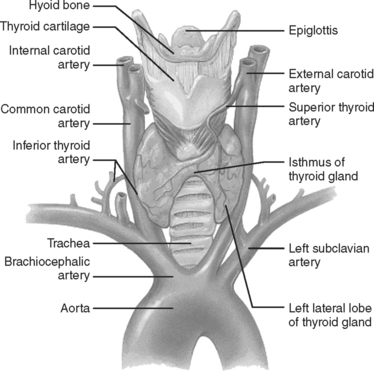
Figure 9 Anatomy of the larynx, cervical, and upper thoracic trachea.
(Copyright 2001 Benjamin Cummings, an imprint of Addison Wesley Longman, Inc.)
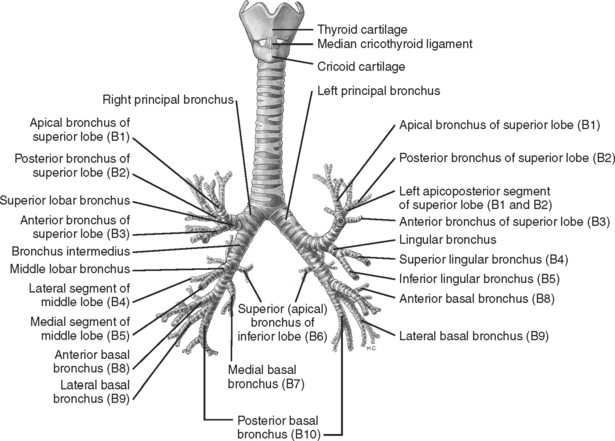
Figure 10 The cartilages of the larynx, trachea, and bronchi: anterior aspect.
(From Gray’s Anatomy, 39th ed. St. Louis, Churchill Livingstone/Mosby, 2004, figure 63.12, with permission.)
Tracheal Injury
Incidence
Disruption of the tracheobronchial tree is a rare occurrence and most surgeons’ experience is limited. On average, one such case is seen per year in large trauma centers.25 Bertelsen and Howitz4 reviewed 1178 postmortem reports of trauma deaths and found 33 (2.8%) with tracheal and/or bronchial disruptions. Of these 33 cases, 27 were dead at the scene.4
Complete cervical transection is rarer still. The true incidence (and tracheobronchial injuries in general) is unknown.26,27 There have been a number of case reports and small series described in the literature; however, the extant surgical experience remains limited.26
Knowledge of emergency airway management is essential. Loss of the airway in this clinical circumstance can rapidly lead to serious complications and/or the patient’s demise.17,28
Mortality in those patients who do not have complete airway loss at the time of injury is due to the severity of associated injuries. Those patients who arrive alive to a trauma center with isolated tracheobronchial injuries, including complete transection, have a reasonable chance for survival if the trauma surgeon has mastered the skills required for managing a difficult airway.29
Beskin30 reported the first successful repair of a complete cervical transection after blunt trauma in 1957. Hood and Sloan31 in 1959 collected 18 cases of tracheobronchial injury in the world literature. Complete tracheal transection was “rarely found.” In a more recent series, Eckert et al.3 reported a total of 105 tracheobronchial injuries, of which 75 were from penetrating trauma and 30 from blunt trauma. Of these, only 24 patients survived the transfer from the scene of the accident to the trauma center. Of the 30 blunt trauma victims reported in this series, 18 were dead on arrival at the emergency department. The majority of those who arrived alive, regardless of the mechanism of injury, had no other associated injuries (15 of 24 [63%]), and the remainder had only one other associated injury, including esophageal injuries (9 of 24 [37%]).3 In the same series, the most commonly injured segment of the tracheobronchial tree in survivors was the cervical trachea (37%). The total number of complete tracheal transections in Ecker and associates’ series is unknown.
Kelly et al.6 reviewed 106 patients with tracheobronchial injuries of which only 6 had a blunt mechanism of injury.6 They concluded that a surgeon must adopt a rapid, aggressive surgical approach to these patients in order to prevent lethal outcomes.6
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree