CHAPTER 37 TRACHEAL AND TRACHEOBRONCHIAL TREE INJURIES
For most of history, acute tracheobronchial injuries have been considered uniformly fatal. In 1871, Winslow observed a healed left mainstem bronchus in a canvasback duck that was taken while hunting. This showed that the animal had survived the rupture and demonstrated the potential of the airways for healing. In 1927, Krinitzki reported the first long-term human survivor. Autopsy findings of a 31-year-old woman, who had been injured at age 10 years when a keg of wine fell on her chest, suggested that humans with tracheobronchial disruption may have the same healing potential as the canvasback duck. The autopsy demonstrated a completely occluded right mainstem bronchus. In the modern era, understanding of anatomy, injury mechanisms, and surgical repair technique has led to improved outcomes in the face of such injuries. Although tracheobronchial injuries still may be lethal, most are treatable. A high index of suspicion is required to make a timely diagnosis and to provide appropriate intervention, both of which are essential if the patient is to have the best opportunity for recovery.
DIAGNOSIS
Presentation
Some retrospective reports show that up to two thirds of these intrathoracic tracheobronchial tears will go unrecognized longer than 24 hours and up to 10% of tracheobronchial tears will not produce any initial clinical or radiological signs and are recognized months later after stricture occurs. Immediate intubation of patients with multisystem trauma can mask laryngeal or high cervical tracheal injuries and contribute to a delay in the diagnosis. After tracheobronchial transection, the peribronchial connective tissues may remain intact and allow continued ventilation of the distal lung analogous to the way perfusion is maintained after traumatic aortic transection. If unrecognized, this injury heals with scarring and granulation tissue and may possibly create bronchial stenosis or obstruction such as in the duck reported by Winslow. After a latent period, granulation tissue and stricture of the bronchus will develop. Distal to the stricture, pneumonia, bronchiectasis, abscesses, and even empyema can result. Complete obstruction without infection leads to prolonged atelectasis and diminished pulmonary function.
Evaluation
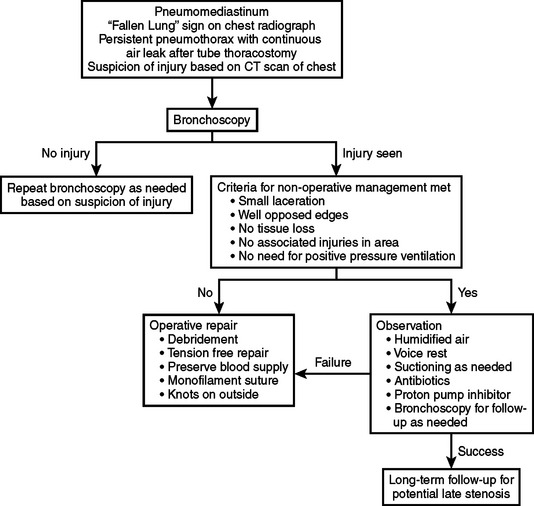
Diagnosis should be suspected based on the clinical history and the constellation of signs and symptoms previously listed. Evaluation of the patient with a suspected injury to the tracheobronchial tree is shown in the algorithm in Figure 1. The advent of spiral computed tomography (CT) has created interest in evaluation of injury with this technique. Three-dimensional reconstruction has been used to elegantly demonstrate the site and extent of injuries in case reports. While tracheobronchial injury may be well demonstrated on CT in some cases, there is no evidence that CT is adequate to exclude an injury and obviate the need for diagnostic bronchoscopy. CT scans suggesting injury should prompt bronchoscopy for definitive diagnosis. In addition to visualization of possible tracheal injury on CT, indications for bronchoscopy include large pneumomediastinum, refractory pneumothorax, large air leak, persistent atelectasis, or, occasionally, marked subcutaneous emphysema. Bronchoscopy, whether rigid or flexible, is the best-studied means of establishing the diagnosis and determining the site, nature, and extent of the tracheobronchial disruption. A potential disadvantage of rigid bronchoscopy is that it requires general anesthesia, as well as a stable ligamentous and bony cervical spine. A rigid scope has the advantage of direct visualization and the ability to provide ventilation. Flexible bronchoscopy may be performed without general anesthesia, and offers the potential for controlled insertion of a nasal or orotracheal tube while maintaining cervical stabilization. The most critical determinant seems to be the experience and comfort level of the endoscopist. It has been shown that, in the hands of an experienced bronchoscopist, either technique can be performed with a high degree of accuracy. Lesions may be missed initially or their severity may be underestimated. These lesions may evolve into more obvious or severe injuries, and for this reason bronchoscopy should be liberally repeated as needed.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree