CHAPTER 34 THORACIC WALL INJURIES: RIBS, STERNAL SCAPULAR FRACTURES, HEMOTHORACES, AND PNEUMOTHORACES
Although many chest injuries are potentially lethal, early man sustained and survived blunt and penetrating chest trauma. Examinations of Neanderthal skeletons have shown evidence of healed penetrating and blunt rib fractures. The Edwin Smith Papyrus, written circa 3000 BC, gave explicit instructions for the management of chest injuries including soft tissue and bony injuries.1 In fact, 8 of the 43 cases discussed concerned chest injuries, suggesting that even at that time, chest injuries accounted for 20%–25% of all trauma.
Trauma to the chest wall and the underlying lung parenchyma either in isolation or as part of multisystem trauma remains exceedingly common and are a frequent source of trauma mortality and morbidity. Hemothoraces and pneumothoraces, while technically not injuries to the thoracic wall, occur commonly in conjunction with such injuries will be considered here as well. Flail chest and its accompanying pulmonary contusion are mentioned only briefly here and are more completely discussed on pages 269–277.
INCIDENCE
Thoracic injuries remain common and are directly attributable for 20%–25% of all trauma deaths; chest injuries are further associated with another 25% of trauma deaths. Chest injuries commonly accompany other injuries and contribute to organ failure in the multiply-injured patient. Rib fractures are among the most commonly encountered injuries. In a review of over 7000 patients seen in a Level I trauma center, 10% had rib fractures; of these, 94% had associated injuries, and 12% died. Half of patients with rib fractures required operation or intensive care unit (ICU) admission, one-third developed complications, and one-third ultimately required extended care in an outpatient facility.2
Pneumothorax is found in over 20% in patients arriving to a trauma center.3 Hemothoraces are encountered with similar frequency. The incidence of both hemothoraces and pneumothoraces is underestimated by plain films, as these injuries are much better visualized by computed tomography (CT) of the chest than the traditional supine anteroposterior chest radiograph (AP CXR).
MECHANISM
Rib fractures are normally the hallmark of significant blunt chest trauma, and increasing numbers of rib fractures are related to increasing morbidity and mortality. The presence of more than three rib fractures in adults is a marker for associated solid visceral trauma and mortality, and thus has been used as a marker for trauma center transfer.4 In hemodynamically stable patients, the presence of blunt chest trauma has also been shown to double the rate of intraabdominal injuries detected by abdominal CT.5 Rib fractures are less common in children due to the resilience of their bony chest wall. Thus, children may suffer major intrathoracic injury without rib fractures and the presence of any rib fracture in a child should be considered a marker for severe injury.6 The presence of acute rib fractures in a young child whose mechanism of injury is unclear or the finding of rib fractures of varying ages should also serve as an indicator for potential child abuse.7,8 Conversely, elderly patients with brittle bones will occasionally have little in the way of intrathoracic injury despite extensive rib fractures.9
DIAGNOSIS
Physical Examination
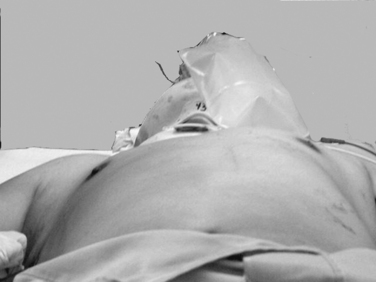
Expeditious inspection and palpation of the chest will provide much information regarding the patient’s injuries (Figure 1). Auscultation and percussion tend to be less reliable due to the high ambient noise of the trauma ED. Hypotension, tachycardia, pallor, or cyanosis suggests shock. In the presence of a known or suspected thoracic injury, shock must be assumed to be from an intrathoracic source. Inspection of the chest itself should include assessment of use of the accessory muscles suggestive of airway obstruction, the symmetry of the chest wall, number and location of wounds, presence of open chest wounds, subcutaneous emphysema, and the presence of “flail” segments. While tracheal deviation in the neck is also frequently cited as a sign of tension pneumothorax, in reality it is rarely if ever seen, even in patients with gross mediastinal deviation on chest x-ray. Palpation can reveal mobile segments of chest wall and further allows appreciation of the symmetry of chest wall motion and of crepitance. Auscultation in trauma has a high specificity but very poor sensitivity, so focus should be placed only on the presence and symmetry of air entry. Heart sounds, such as the muffled heartbeat in Beck’s triad or the “mediastinal crunch” of Hamman’s sign, are also difficult to obtain clearly in the trauma bay. The absence or asymmetry of breath sounds, however, is very suggestive of significant pathology; in the unstable patient, this is an indication for intervention on clinical grounds and a contraindication for imaging studies. Thoracic percussion, even more than auscultation, is difficult to interpret in the trauma setting and is rarely useful.
Radiographic Studies
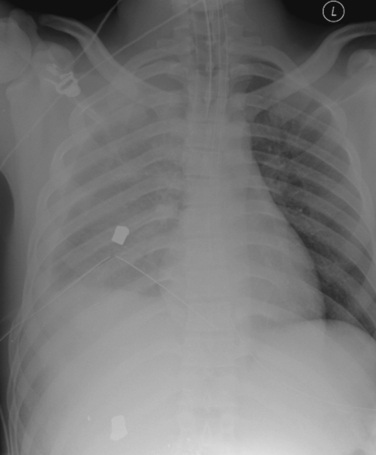
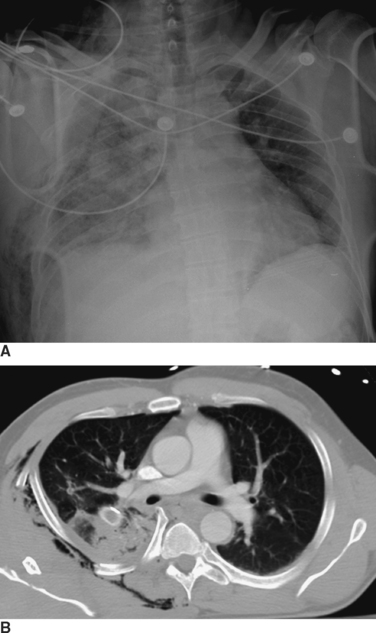
Radiographic imaging is extremely useful in the diagnosis of a hemothorax or pneumothorax. Indeed, in a hemodynamically stable patient, the diagnosis is often made on the portable AP CXR obtained for the secondary survey. In the supine position the AP CXR will reveal hemothorax only when at least 200–300 ml of blood is present in the pleural space, and is suggested by an overall opacification or haziness compared to the contralateral hemithorax as the fluid will layer posteriorly (Figure 2). False “negative”–appearing CXR may occur in the setting of bilateral hemothoraces (no difference between the two sides) or when there is a simultaneous anterior pneumothorax (decreasing the relative density more similar to the other side). In the patient with penetrating chest trauma, the CXR is best taken with the patient upright which increases the sensitivity for both hemothoraces and pneumothoraces. Chest ultrasound may help to identify the presence of pleural fluid, but its sensitivity and specificity for this purpose have not been well-defined.
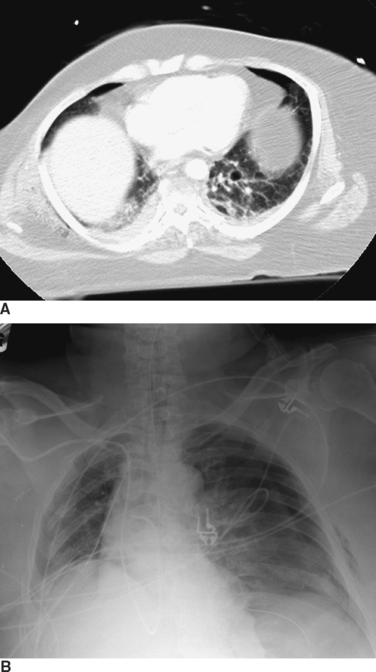
The appropriate management of the patient with “CT-only” pneumothorax is a matter of some controversy (Figure 3). The reported incidence of these pneumothoraces in blunt trauma patients is 2%–8%.10,11 The available literature suggests that 20% of these patients will require tube thoracostomy. The decision to place a chest tube, however, should be dictated by the patient’s overall status. Patients who are multiply injured, are in hemorrhagic shock, or have sustained a traumatic brain injury will not tolerate progression of even a small pneumothorax (see Figure 3). These patients would benefit from tube thoracostomy. In patients where the clinical picture appears stable, observation can be undertaken, with serial radiographs taken at 6 and 24 hours after diagnosis.
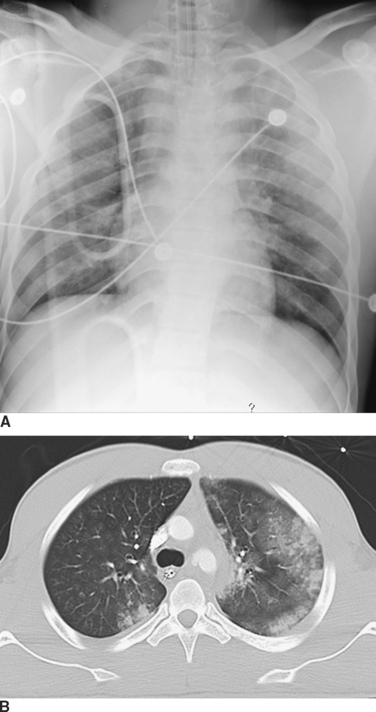
Computed tomography (CT) of the chest has become increasingly accepted in the early management of trauma. CT can reveal injuries not seen on initial CXR in about two-thirds of major trauma patients12 and can lead to therapeutic changes in 5%–30% of cases13,14 (Figure 4). In addition, CT scanning may reveal additional findings that are only suggested by an abnormal CXR (Figure 5). There are a number of specific situations in which chest CT contributes significantly to trauma management. CT of the thoracic spine is the “gold-standard” imaging modality for assessing vertebral body as well as posterior element fractures, and is also helpful in imaging the spine at the cervicothoracic junction.12,14,15 In patients with the nonspecific finding of a widened mediastinum on CXR, use of CT can help to limit the use of aortography to assess aortic injuries.16–18 As CT technology improves and as further studies become available, the role of CT in chest trauma will become better-defined.
Ultrasonography has become important in the assessment of intra-abdominal hemorrhage and pericardial fluid collections in the trauma patient. Recent reports also suggest that it might be useful to assess the pleural spaces for pneumothoraces and hemothoraces.19–21 The pleural space is interrogated by placing the ultrasound probe between the ribs and looking for the characteristic signs of pneumothorax.19,22
AAST-OIS GRADING
The American Association for the Surgery of Trauma-Organ Injury Scale (AAST-OIS) grading scales for chest wall and lung injury developed by Moore et al.23 are listed in Tables 1 and 2.
Table 1 Chest Wall Injury Scale
| Grade | Injury Type | Description of Injury |
|---|---|---|
| I | Contusion | Any size |
| Laceration | Skin and subcutaneous | |
| Fracture | <3 ribs, closed; nondisplaced clavicle, closed | |
| II | Laceration | Skin, subcutaneous, and muscle |
| Fracture | >3 adjacent ribs, closed | |
| Open or displaced clavicle | ||
| Nondisplaced sternum, closed | ||
| Scapular body, open or closed | ||
| III | Laceration | Full thickness, including pleural penetration |
| Fracture | Open or displaced sternum | |
| Flail sternum | ||
| Unilateral flail sternum (<3 ribs) | ||
| IV | Laceration | Avulsion of chest wall tissues with underlying rib fractures |
| Fracture | Unilateral flail chest (<3 ribs) | |
| V | Fracture | Bilateral flail chest (>3 ribs on both sides) |
Adapted from Moore EE, Cogbill TH, Malangoni MA, et al: Organ injury scaling. Surg Clin North Am 75(2):293–303, 1995.
| Grade | Injury Type | Description of Injury |
|---|---|---|
| I | Contusion | Unilateral, <1 lobe |
| II | Contusion | Unlateral, 1 lobe |
| Laceration | Simple pneumothorax | |
| Contusion | Unilateral, L1 lobe | |
| III | Laceration | Persistent (>72 hours) air leak from distal airway |
| Hematoma | Nonexpanding intraparenchymal | |
| Laceration | Major (segmental or lobar) air leak | |
| IV | Hematoma | Expanding intraparenchymal |
| Vascular | Primary branch intrapulmonary vessel disruption | |
| V | Vascular | Hilar vessel disruption |
| VI | Vascular | Total uncontained transaction of pulmonary hilum |
Adapted from Moore EE, Cogbill TH, Malangoni MA, et al: Organ injury scaling. Surg Clin North Am 75(2):293–303, 1995.
MANAGEMENT OF SPECIFIC INJURIES TO CHEST WALL
Chest Wall Defects
In large chest wall defects, the occlusive dressing is of no value. These patients must be endotracheally intubated with positive pressure ventilation. Operative management then focuses on control of hemorrhage from the chest wall and from any associated injuries. Chest wall hemorrhage in these cases may be life-threatening and may mandate emergent thoracotomy. “Damage control” with packing may be the optimal initial management of these patients. The chest defect can be temporarily closed with skin or prosthetic material. The definitive closure of these defects, which may require tissue-transfer procedures, is best deferred until the patient is fully resuscitated, physiologically sound, and able to tolerate a lengthy operation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree