CHAPTER 41 THORACIC VASCULAR INJURY
One of the earliest reports of thoracic vascular injury was described by Vesalius in 1557 of a fatal, blunt traumatic rupture of the aorta in a man who was thrown from a horse.1 In 1946, DeBakey and Simeone collectively described the morbidity and the complexity of the few battlefield thoracic vascular injuries that occurred during World War II.2 It was not until 1959 that Passaro and Pace3 reported the first successful primary repair of traumatic aortic rupture performed by Klassen in 1958.
Before the development of modern trauma centers, most individuals with thoracic vascular trauma died before reaching the hospital. With the advent of rapid-response trauma systems, the incidence of thoracic vascular injury that survives to the hospital is increasing and the complexity of the injuries is becoming more challenging. Mattox et al.4 reported 1467 cardiovascular injuries in 1117 patients over a 5-year period from 1979 to 1983 in Houston, Texas.
INCIDENCE
Thoracic trauma is responsible for 50% of all trauma deaths nationally.5 The incidence of chest trauma is reported to be 12 per million per day in the United States by Beeson and Saegesser.6 In a large series of thoracic trauma patients, the aorta and great vessels were injured in 4% of cases.7 Furthermore, thoracic vascular injuries are often associated with other nonvascular injuries because of their anatomic location and mechanism of injury.
MECHANISM OF INJURY
A large number of thoracic great-vessel injuries are caused by penetrating or iatrogenic trauma.4 The mechanism of injury for penetrating thoracic vascular trauma is usually direct laceration or penetration of blood vessels. This type of injury can often present with external or internal hemorrhage, vascular thrombosis from intimal flap, or pseudoaneurysms. Because of the various types of missiles involved in penetrating vascular trauma, all thoracic vascular structures are at risk. External bleeding from skin tracts usually occurs with injuries to vessels at the thoracic inlet, whereas internal hemorrhage commonly occurs with aortic and caval injuries. Intrathoracic great-vessel injuries can present with internal bleeding into the mediastinum, pleural space, or pericardial sac. It is important to note that the presence of a normal palpable distal pulse does not rule out a proximal vascular injury. Penetrating vascular injuries can be completely contained by perivascular adventitia with blood flow preserved distally.
Because of the large diameter of thoracic vessels, bullets can directly enter vessels and migrate distally (Figure 1). The diagnosis of bullet embolism is often delayed because the course of the bullet may not be obvious. Bullet embolism for thoracic missiles usually lodges in the iliac and femoral vessels. The site of entry should be controlled for hemorrhage first, followed with attempts at removing the bullet emboli with endovascular intervention or separate arteriotomy.
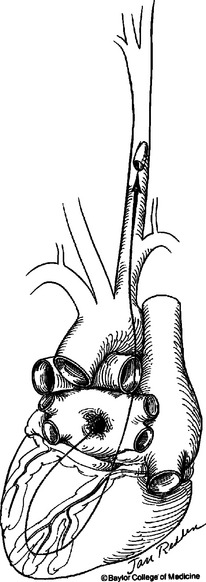
Figure 1 Bullet embolism from the left atrium to the left carotid artery.
(Courtesy Jan Redden, Baylor College of Medicine, 1980.)
DIAGNOSIS
Indicators of possible thoracic vascular injury are outlined in Table 1. The single most important screening tool for thoracic vascular trauma is the anteroposterior chest radiograph. There are numerous radiographic findings suggesting thoracic vascular injury as outlined in Table 2. One of the most reliable radiographic findings suggestive of blunt thoracic vascular injury is alteration of the aortic knob contour on chest radiograph.
Table 1 Indicators of Possible Thoracic Vascular Injury
| Mechanism of Injury |
| Suggestive Physical Signs |
| Findings on Chest Radiographs |
Table 2 Radiological Findings Suggesting Great Vessel Injury
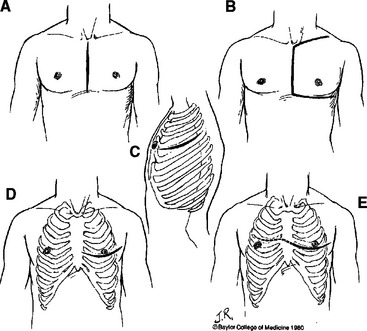
Arteriography remains the “gold standard” imaging study for evaluation of suspected thoracic vascular injury. It is important to note that preoperative angiography is never indicated in hemodynamically unstable patients with suspected thoracic vascular injury. In hemodynamically stable patients with suspected penetrating injury to the innominate, carotid, or subclavian arteries, preoperative arteriography is indicated to provide information on the type of incisions to make for proximal control of these branched aortic vessels (Figure 2). Furthermore, the proximity of missile trajectory to brachiocephalic vessels is an indication for arteriography in order to definitively rule out an injury. In blunt thoracic trauma, the need for arteriography is determined by mechanism of injury, physical examination, and screening chest radiograph. Fifty percent of patients with blunt thoracic vascular injury present without any external signs of injury.8 Seven percent of patients with blunt injury to the aorta and its branched vessels have a normal-appearing mediastinum on screening chest radiograph.9 Therefore, additional imaging studies are indicated in patients with either physical examination or chest radiograph suggesting thoracic vascular injury.
In patients with a significant mechanism of injury, but a benign physical examination and normal admission chest radiograph, it is reasonable to repeat a delayed chest radiograph to screen for radiographic evidence of thoracic vascular injury with a follow-up arteriography for a definitive diagnosis. Contrast-enhanced spiral computed tomography (CT) of the chest is being used more frequently for evaluating thoracic trauma. The sensitivity of chest CT scan for thoracic vascular injury ranges from 54% to 80%.10–16 The negative predictive value of a chest CT scan is close to 100% in evaluating thoracic vascular injury.10–16 Therefore, it is also reasonable to use chest CT scan as a screening tool in stable patients with significant mechanism of injury, normal-appearing admission chest radiograph, and benign physical examination to rule out an underlying thoracic vascular injury. However, any positive findings on CT scan should be followed by the “gold standard” arteriography for definitive diagnosis of thoracic vascular injury before operative intervention.
Transesophageal echocardiography (TEE) offers several potential advantages to arteriography in evaluating thoracic vascular injury. Avoidance of intravenous contrast, the concomitant information gained on cardiac function, and its portability are potential advantages compared with arteriography. However, published literature reports sensitivity and specificity of 85.7% and 92.0% for TEE compared with 89.0% and 100% for arteriography, respectively, in diagnosing aortic injury.17 TEE is also heavily technician and operator dependent. Furthermore, the ascending aorta, proximal aortic arch, and branch aortic vessel are extremely difficult to visualize with TEE. Therefore, its use in evaluating thoracic vascular injury is not routinely recommended.