| Chest radiography findings concerning for blunt aortic injury |
| Widened mediastinum (>8 cm on supine or >6 cm on upright film) |
| Obscured aortic knob |
| Left apical cap (blood above apex of lung) |
| Large left hemothorax |
| Rightward deviation of nasogastric tube |
| Rightward deviation of trachea or downward deviation of right mainstem bronchus |
| Wide left paravertebral stripe |
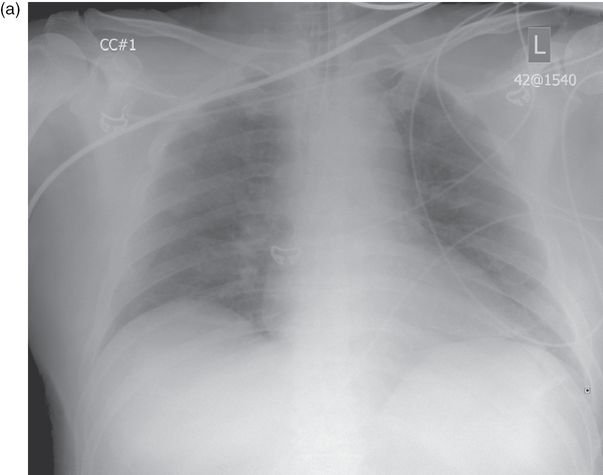
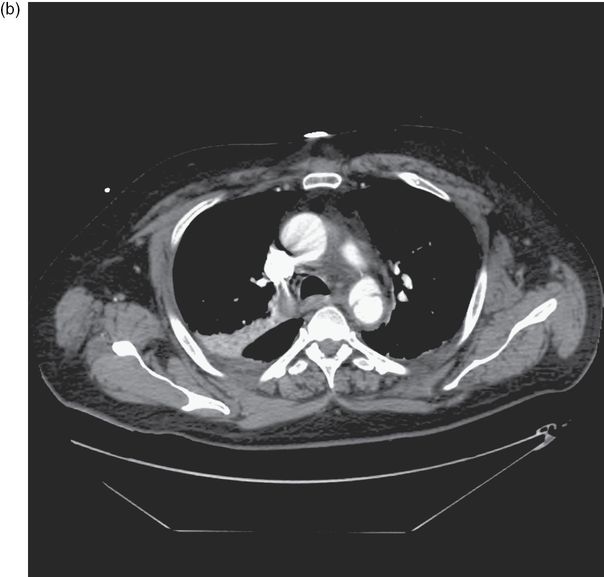
Figure 10.1. (a) demonstrates a wide mediastinum suspicious for blunt aortic injury on portable chest radiograph. The diagnosis is confirmed on CT (b). (Image courtesy of Michael A. Gibbs, MD.)
Critical management
- Immediate surgical repair is necessary in patients who are unstable due to traumatic aortic injury.
- Medical management of the stable traumatic aortic injury patient or those in whom surgical repair must be delayed centers on the reduction of wall tension and shearing forces. Use a short-acting beta-blocker, such as esmolol, to reduce heart rate to a goal of 60 bpm, followed by an arterial vasodilator such as nicardipine or sodium nitroprusside to reduce blood pressure to 100–120 mmHg. These measures minimize risk of rupture prior to repair and can allow delay of repair while other more critical injuries are treated. Patients with significant traumatic head injury are an exception to this recommendation.
Sudden deterioration
- The patient with traumatic aortic injury is at extremely high risk for deterioration.
- Rapid surgical consultation at the first suspicion of traumatic aortic injury must be obtained to expedite repair.
Tracheobronchial injury
- Injury to the tracheobronchial tree is relatively uncommon.
Presentation
Classic presentation
- May present with dyspnea, subcutaneous emphysema, sternal tenderness, and Hamman’s sign (a “crunching” sound heard on auscultation of the precordium due to mediastinal emphysema).
- Tracheobronchial injury should be suspected in the presence of a large air leak from a chest tube, or a rapidly reaccumulating pneumothorax or pneumomediastinum.
- Diagnosis of tracheobronchial injury is frequently delayed and may present as retained lung secretions, poor lung expansion, persistent air leak or recurrent pneumothorax, or bronchial obstruction in the days to weeks following the injury.
Critical presentation
- Tracheal transection is usually associated with multiple other severe injuries and is generally fatal.
- Missed tracheobronchial injury can result in mediastinitis, bronchial stenosis, and recurrent pulmonary infections.
Diagnosis and evaluation
- Definitive diagnosis may be established by bronchoscopy or operative evaluation.
- High-quality CT scan may also diagnose tracheobronchial injury.
Critical management
- Most tracheobronchial injuries should be surgically repaired; however, observation may be considered in hemodynamically stable patients in whom ventilation is not difficult, there is no accumulating subcutaneous or mediastinal emphysema, and there is no involvement of the esophagus.
Flail chest
- Flail chest occurs when three or more ribs are each fractured in two or more places resulting in a “floating” segment of the rib cage. The floating segment paradoxically moves inward with inhalation and outward with exhalation and can greatly increase work of breathing.
Presentation
Classic presentation
- The patient with flail chest may present with pain, dyspnea, tachypnea, chest wall tenderness and crepitus, and visible flail segment on observation of breathing.
Critical presentation
- Patients with a significant flail chest, especially older patients or those with underlying lung disease or multiple other injuries, may present with respiratory distress or arrest.
Diagnosis and evaluation
- Chest radiograph shows multiple rib fractures.
- Patients who present with flail chest should receive CT of the chest to evaluate for other injuries including blunt aortic injuries, pulmonary contusions and pneumothorax.
Critical management
- External stabilization of the flail segment restricts chest expansion and is not recommended.
- Positive-pressure ventilation, either invasive or noninvasive, may be used in patients with hypoxia, hypercapnea, or respiratory distress. However, obligatory mechanical ventilation in flail chest should be avoided as it may increase complications and many patients will do well with pain control and pulmonary toilet alone.
- As with all chest wall injuries, pain management is critical to prevent splinting and the development of atelectasis or pneumonia. An epidural catheter is preferred for pain control in severe chest injury.
- Elderly trauma patients who sustain blunt chest trauma with rib fractures have twice the mortality and morbidity of younger patients with similar injuries. For each additional rib fracture in the elderly, mortality increases by 19% and the risk of pneumonia by 27%. Aggressive pain control with epidural catheter placement is recommended in these patients.
- Surgical fixation of rib or sternal fractures is controversial but may be considered.
Sudden deterioration
- Patients with flail chest can deteriorate rapidly to the point of respiratory arrest due to increased work of breathing combined with hypoxia caused by underlying lung contusion.
- Endotracheal intubation and mechanical ventilation is indicated for the decompensating patient with flail chest.
References
Ball CG, Kirkpatrick AW, Laupland KB, et al. Factors related to the failure of radiographic recognition of occult posttraumatic pneumothoraces. Am J Surg. 2005; 189: 541–6; discussion 546.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







