
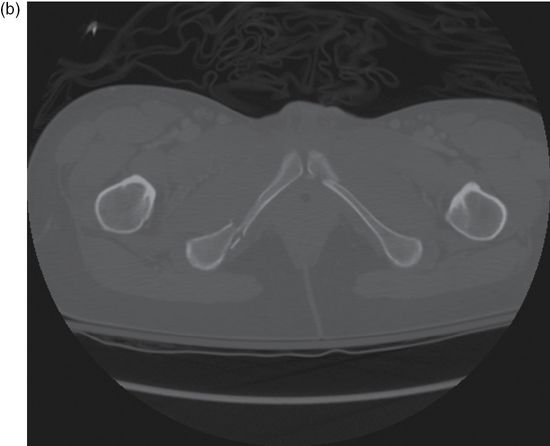
Figure 12.1. (a) Young–Burgess lateral compression (LC) pelvic fracture classifications; (b) computed tomography (CT) of LCI fracture pattern; (c) radiograph of LCI fracture pattern. (Reprinted with permission from Hammel J. Pelvic fracture. In: Legone, E, Shockley, L, Traum, W. A Comprehensive Emergency Medicine Approach. Cambridge University Press. 2011.)


Presentation
Classic presentation
- Patients (who can verbalize) with severe pelvic trauma may complain of pain at the fracture site, low back, abdominal, or hip pain, though they may be altered or have other distracting injuries.
- They are frequently hypotensive and require rapid fluid resuscitation.
- It is important to keep pelvic fractures high in the differential diagnosis when evaluating any patient with multiple injuries.
Critical presentation
- Severely injured patients are often hypotensive and require early intubation and fluid resuscitation.
Diagnosis and evaluation
- Vital signs are often an early indicator of severity of hypovolemic shock.
- Tachycardia is usually the first abnormal vital sign that may lead to the diagnosis of acute blood loss.
- Hypotension is a late finding and a sign of significant hemorrhage.
- Tachycardia is usually the first abnormal vital sign that may lead to the diagnosis of acute blood loss.
- Signs of pelvic trauma
- Ecchymosis, abrasions, or hematomas
- Pelvic and leg deformity or asymmetry
- Bony tenderness to palpation
- Instability with gentle lateral pressure on the iliac wings
- Peripheral neurovascular deficit
- Difficulty with active and passive range of motion of the hip
- Blood at urethral meatus
- Rectal bleeding and poor sphincter tone
- “High-riding prostate” is a theoretical finding for possible urethral injury.
- Ecchymosis, abrasions, or hematomas
- Diagnostic tests
- Laboratory tests:
- Type and cross
- Serum electrolytes
- CBC
- Lactic acid
- Coagulation panel
- Urinalysis
- Beta human chorionic gonadotropin for women of childbearing age.
- Type and cross
- eFAST examination
- All trauma patients should have an extended focused assessment with sonography for trauma to investigate for internal bleeding and pneumothorax.
- eFAST examinations are not sensitive or specific for retroperitoneal injuries but they are highly sensitive in detecting clinically significant hemoperitoneum.
- All trauma patients should have an extended focused assessment with sonography for trauma to investigate for internal bleeding and pneumothorax.
- Chest radiography
- Portable chest radiography is complementary to the e-FAST to determine the extent of other chest injuries.
- Pelvic radiography
- Anteroposterior (AP) pelvic radiography is the initial imaging modality of choice; it identifies up to 90% of fractures.
- Posterior sacroiliac ligament disruption may be difficult to diagnose.
- In the past, inlet and outlet pelvic views (taken with beam 45 degrees caudally or cephalad, respectively) were used to demonstrate posterior dislocation of pelvic ring and opening of pubic symphysis; these views are now replaced by CT imaging.
- Anteroposterior (AP) pelvic radiography is the initial imaging modality of choice; it identifies up to 90% of fractures.
- Abdominal/pelvic CT
- Provides optimal imaging for evaluation of bony pelvic anatomy, while also providing information on pelvic, retroperitoneal, and intra-abdominal bleeding.
- In patients with a significant mechanism of injury, CT of the abdomen/pelvis is often performed.
- Intravenous contrast is necessary to highlight active hemorrhage.
- CT scan can also confirm hip dislocation associated with an acetabular fracture.
- Provides optimal imaging for evaluation of bony pelvic anatomy, while also providing information on pelvic, retroperitoneal, and intra-abdominal bleeding.
- Laboratory tests:
Critical management
| ABCs |
| Correct hemodynamic instability |
| FAST examination and pelvic radiograph |
| Pelvic binding, if indicated |
| Pain control |
| Avoid hypothermia |
| Invasive/operative management |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




