207 Thoracic Trauma
 Initial Assessment
Initial Assessment
Primary Survey
The Advanced Trauma Life Support (ATLS) course of the American College of Surgeons Committee on Trauma1 provides basic tenets for the management of all injured patients. Initial treatment of seriously injured patients consists of a primary survey, resuscitation, secondary survey, diagnostic evaluation, and definitive care. Although the concepts are presented in a sequential fashion, in reality, they often proceed simultaneously. The process begins with the primary survey, designed to identify and treat conditions that constitute an immediate threat to life. The primary survey includes a stepwise evaluation of the “ABCs”: Airway, with cervical spine protection; Breathing; and Circulation.
Resuscitative Thoracotomy
Some trauma victims who arrive in extremis may be candidates for resuscitative thoracotomy in the ED (EDT). The primary objectives of EDT are to (1) release pericardial tamponade, (2) control intrathoracic hemorrhage, (3) control bronchovenous air embolism or bronchopleural fistula, (4) perform open cardiac massage, and (5) temporarily occlude the descending thoracic aorta to redistribute limited blood flow to the brain and myocardium and attenuate subdiaphragmatic hemorrhage. The critical determinants of survival following this procedure are the mechanism of injury and the patient’s condition at the time of thoracotomy. The best outcomes are seen in adult patients with isolated penetrating cardiac injuries who present to the ED with detectable blood pressure; survival averages 35% in large series. For penetrating noncardiac injuries, the salvage rate is 15% for patients who present with vital signs and less than 10% if only signs of life (i.e., pupillary activity, spontaneous respirations, narrow complex cardiac activity) are present. Resuscitative thoracotomy is least beneficial in the treatment of blunt injury or in the absence of signs of life, with only 1% to 2% of patients surviving.2
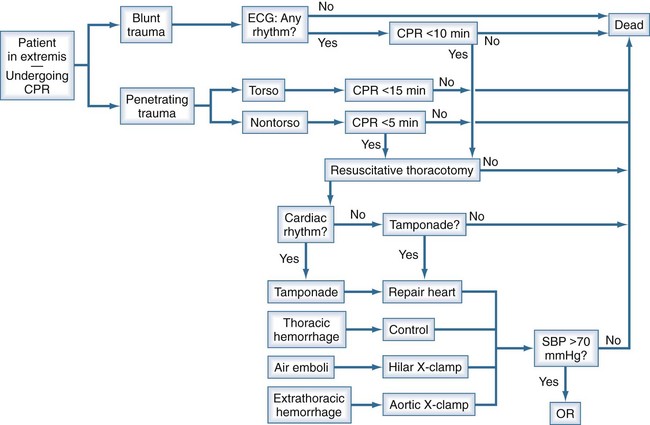
The value of thoracotomy in the resuscitation of a patient in profound shock but not yet dead is unquestioned. Its indiscriminate use, however, renders it a low-yield, high-cost procedure, including risks to the health care team. A recent Western Trauma Association (WTA) multicenter study attempted to determine the limits of EDT to enable the development of rational guidelines to withhold or terminate resuscitative efforts.3 The WTA multicenter experience suggests EDT is unlikely to yield productive survival when patients: (1) sustain blunt trauma and require more than 10 minutes of prehospital cardiopulmonary resuscitation (CPR) without response, (2) have penetrating wounds and undergo more than 15 minutes of prehospital CPR without response, or (3) manifest asystole without pericardial tamponade. There are likely to be exceptions, and the clinician must individualize care in each case. Based on our experience and that reflected in the current literature, we have formulated a decision algorithm for resuscitation of moribund trauma patients (Figure 207-1). Patients arriving in extremis following blunt injury undergo thoracotomy only if they have a rhythm on electrocardiography (ECG) and have had fewer than 10 minutes of CPR. Penetrating trauma victims in extremis undergo thoracotomy if they have had fewer than 15 minutes (for torso injuries) or 5 minutes (for non-torso injuries) of CPR. If, upon opening the chest, there is no organized cardiac activity and no blood in the pericardium, the patient is declared dead. All other patients are treated according to the injury. Pericardial tamponade is decompressed, and bleeding from cardiac wounds is controlled. Suspected air embolism is treated by application of a pulmonary hilar cross-clamp, vigorous cardiac massage, and aortic root and left ventricular aspiration for air. Intrathoracic hemorrhage is controlled. Cardiovascular collapse from suspected intraabdominal hemorrhage is temporized by occluding the descending thoracic aorta. Those patients who respond to treatment and have a systolic blood pressure above 70 mm Hg are rapidly transported to the operating room for definitive treatment of their injuries.
 Pleural Space
Pleural Space
Pneumothorax
Pneumothorax is a common sequela of thoracic trauma. Visceral pleural disruption due to penetrating trauma, blunt shearing, or lacerations from fractured bones allows egress of air into the pleural space as negative intrapleural pressure is created during inspiration. Physical findings include decreased breath sounds, hyperresonance to percussion, and decreased expansion of the chest wall on the affected side. If not relieved, a simple pneumothorax may progress to a tension pneumothorax, especially if the patient is receiving positive-pressure ventilation. In this setting, the mediastinal structures are shifted away from the affected side. In addition to the mechanical impediment to gas exchange, venous return to the heart is impaired secondary to vena caval distortion, and shock ensues. Immediate decompression is mandatory and can be lifesaving (see Tube Thoracostomy).
With the growing use of thoracoabdominal computed tomography (CT) in the evaluation of trauma patients, small pneumothoraces that are not seen on plain radiographs are often discovered. The treatment of these so-called occult pneumothoraces is not as well defined as the treatment of the usual pneumothorax. Generally they do not require treatment but should be monitored for progression. The notion of “prophylactic” tube thoracostomy in the setting of positive-pressure ventilation has been challenged, but vigilance is important to detect progression to tension pneumothorax in approximately 10% of patients.4
Tube Thoracostomy
In the setting of tension pneumothorax, if tube thoracostomy is not immediately available, the chest can be decompressed with a large-bore needle as a temporizing measure. Although many authors promote decompression via the second intercostal space in the midclavicular line, injuries to the great vessels and heart have been described as a result of this procedure. Further, catheters may be misdirected or kinked in the pectoralis major muscle or breast tissue, rendering them ineffective, often unbeknownst to the clinician. The author’s preference is to insert the needle through the fifth intercostal space in the midaxillary line. This site allows rapid, reliable entry into the pleural space, and the risk of great vessel injury is essentially nil.5
The major morbidity related to tube thoracostomy is infectious (pneumonia, empyema), reported in up to 20% of patients. Some investigators have proposed routine prophylactic antibiotics to prevent such morbidity, but this has been controversial. A multicenter prospective randomized clinical trial comparing prophylactic antibiotics versus placebo found that antibiotics did not reduce the incidence of empyema or pneumonia. Moreover, the use of antibiotics was associated with a definite pattern of resistance in subsequent hospital-acquired infections.6
Pneumothoraces and air leaks should be resolved before removal of the tube, and ideally, drainage should be less than 2 mL/kg/d. After 12 to 24 hours without an air leak, the tube may be removed while on suction. However, a 6- to 12-hour trial of waterseal drainage is generally warranted to observe for an occult air leak.7 It has been recommended that tubes be removed at maximal deep inspiration with a Valsalva maneuver, but recurrent pneumothorax may occur in 6% to 8% of patients regardless of respiratory phase.8 More than 20% of patients require longer than 3 days to resolve an air leak; their hospital course may be expedited by the use of thoracoscopy.9
 Chest Wall Injury
Chest Wall Injury
Rib Fracture
Rib fractures are estimated to occur in 10% of patients presenting for evaluation by trauma services. Ziegler and Agarwal reported that more than 90% of patients with rib fractures had associated injuries, and half of these patients required intensive care unit (ICU) care.10 In their series, the overall mortality of patients presenting with rib fractures was 12%. Multiple rib fractures, fractures of the first or second rib, and scapular fractures signify higher-energy injuries and should prompt a search for associated intraabdominal injury or thoracic vascular injury.
Single rib fractures in young patients are generally of little consequence; however, rib fractures in elderly patients can lead to diminished pulmonary function with potentially disastrous infectious complications. Patients over the age of 65 have two- to fivefold increases in morbidity and mortality compared with younger patients with similar injuries.11,12 Bulger et al. found that for each additional rib fracture in the elderly, the risk of pneumonia increases by 27%, and mortality increases by 19%.11 A key factor in the management of these patients is pain control to facilitate coughing and clearance of secretions. Epidural catheters have proved to be efficacious and superior to patient-controlled analgesia in this regard and may also modify the immune response.13,14 Rib blocks may provide immediate relief in the ED or ICU while awaiting epidural catheter placement. Bupivacaine or a lidocaine-bupivacaine mixture may be injected into the intercostal bundle (with care taken not to inject intravascularly) of the fractured ribs and those above and below them. An intercostal catheter provides another alternative in the event an epidural catheter is unavailable or contraindicated.15
Flail Chest
Two or more ribs fractured in two or more places produce a flail segment of the chest wall. This segment moves paradoxically—inward during inspiration, outward during expiration—because it is detached from the chest wall and thus susceptible to the forces of intrapleural pressure. The mechanical effects on respiration are related to the size of the flail segment. However, a more important cause of respiratory compromise following flail chest injury is the pulmonary contusion that invariably accompanies it. Treatment is supportive, including supplemental oxygen, analgesia, and pulmonary toilet. Endotracheal intubation with positive-pressure ventilation is sometimes necessary. Surgical stabilization of the flail segment, and rib fracture repair in general, has been performed for decades. At this time, there is a need for multicenter randomized trials with long-term follow-up to identify appropriate patients and optimal techniques.16
Sternal Fracture
Early series of sternal fractures described the “steering wheel syndrome” (rapid deceleration, with impact of the sternum on the steering wheel) as the most common cause of sternal fracture. In these series, associated blunt cardiac injury (see later) was common, so sternal fractures were thought to be harbingers of significant occult thoracic injury. More recently, however, sternal fractures have been reported more commonly with the “seatbelt syndrome” (in conjunction with three-point, or bandolier, seat belts). Because the elements of deceleration and steering wheel impact are no longer prominent, associated injuries are relatively infrequent.17 Stable patients without dyspnea, ECG abnormalities, or significantly displaced fractures can be safely discharged from the ED. Rest and analgesia are adequate treatment.
 Lung Injury
Lung Injury
Pulmonary Contusion
Pulmonary contusion is a common problem, occurring in one-quarter of patients with injury severity scores (ISS) over 15 and in a majority of patients sustaining major chest trauma. The injury may result from a direct blow, shearing or bursting at gas/liquid or high-density/low-density interfaces, or the transmission of a shock wave. The pathophysiologic changes fundamentally include hemorrhage with surrounding edema, with a broad range of severity up to “hepatization” of the lung. The clinical result is hypoxia and increased work of breathing due to ventilation/perfusion mismatching and decreased pulmonary compliance. Pulmonary contusions may not appear on initial chest radiograph, although they are usually seen by 6 hours after the injury; chest CT is more sensitive at diagnosing early pulmonary contusions. Treatment is supportive, including supplemental oxygen, pain control, pulmonary toilet, and judicious fluid management. There is no role for either routine antibiotics or steroid therapy.18 Intubation and mechanical ventilation are employed only as necessary. The degree of pulmonary dysfunction usually peaks at 72 hours and generally resolves within 7 days in the absence of associated nosocomial pneumonia. Mortality related to pulmonary contusion has improved greatly with advances in critical care.
Posttraumatic pulmonary pseudocysts are cavitary lesions that occur in approximately 3% of lung parenchymal injuries.19 They may be asymptomatic or associated with mild nonspecific symptoms and are often noted incidentally on the chest radiograph. Most resolve spontaneously within 2 to 4 months. However, surgical intervention is indicated for infection, bleeding, and rupture. The lesion can be distinguished from an abscess by CT-guided aspiration. If infected, catheter drainage may be required for definitive management.
Pulmonary Laceration
Penetrating trauma, blunt shearing, or the ends of fractured bones can cause pulmonary laceration and parenchymal disruption. The typical clinical presentation is a hemopneumothorax. Bleeding is usually self-limited, and the vast majority of these injuries are definitively managed by tube thoracostomy alone. Of the 10% of patients requiring thoracotomy, approximately 20% need lung resection. Historically, this group has experienced high morbidity and mortality, with mortality following pneumonectomy approaching 100%. In 1994, Wall and colleagues introduced the concept of pulmonary tractotomy as a nonresectional means of managing penetrating lung injuries.20 It is indicated for deep through-and-through injuries that do not involve central hilar vessels or airways. The wound tract is exposed by passing clamps (as originally described) or a stapling device (our preference) through the wound and dividing the bridge of lung tissue. Air leaks and bleeding points are sutured, and the wound tract is left open. The literature contains mixed reports of the success of this approach, but the morbidity and mortality compare favorably with those associated with anatomic resections.21
 Pneumomediastinum
Pneumomediastinum
Pneumomediastinum has classically been considered a sign of aerodigestive injury. This was particularly true of pneumomediastinum seen on plain radiography; however, with expanding use of chest CT, pneumomediastinum is being seen with increasing frequency. Recent analyses have found that pneumomediastinum is present on approximately 5% of chest CT scans following trauma, but that only 10% of these patients actually have aerodigestive injuries.22 In the absence of signs or symptoms or additional suspicious findings on CT scan, further investigation is not necessary.22,23
 Tracheobronchial Injury
Tracheobronchial Injury
Tracheobronchial injuries are uncommon but should be excluded in the presence of cervical subcutaneous emphysema, pneumomediastinum (see earlier), or pneumothorax with a persistent air leak. Although CT may reveal the injury, the preferred definitive diagnostic test is bronchoscopy. Most penetrating injuries occur in the cervical area and are approached via cervical incisions, with partial or complete sternotomy as needed. Blunt injuries more commonly occur in the distal trachea or right mainstem bronchus and are approached via sternotomy or thoracotomy. Tracheal injuries can usually be repaired primarily or by resection and reanastomosis without tracheostomy; late stenosis is uncommon. On the other hand, laryngotracheal injuries often require tracheostomy as an adjunct to repair, and tracheal stenosis is a common late complication. Absorbable monofilament sutures are preferred. Bronchial injuries may be repaired, but severe disruptions or associated vascular injuries may necessitate pneumonectomy or lobectomy. Positive end-expiratory pressure is avoided postoperatively.24
 Esophageal Injury
Esophageal Injury
Esophageal perforation from blunt-force trauma is a rare event caused by a sudden rise in intraluminal pressure or by the upper esophagus being crushed between the trachea and a vertebral body. More commonly, esophageal injury is the result of penetrating trauma. Early signs and symptoms of injury can be subtle, so a high index of suspicion is important. Pneumomediastinum should prompt consideration of this injury (see earlier). Barium esophagography is considered the diagnostic study of choice and can be readily obtained in a stable, awake patient.25 However, videoendoscopy can be done at the bedside virtually anywhere in the hospital and has excellent accuracy, particularly in the pharyngeal area. Thus, it is preferred in critically ill or unstable patients in the ICU or operating room.26
Evaluation should be expeditious because delays in definitive care are associated with increased morbidity and mortality. If the injury is identified within 24 hours, it can usually be treated with débridement, primary repair, and drainage. Injuries identified after 24 hours are better treated with débridement and drainage, cervical esophagostomy, and feeding tube placement.25
 Blunt Cardiac Injury
Blunt Cardiac Injury
Cardiac Rupture
Cardiac rupture is the most severe form of BCI; 80% to 90% of ruptures are lethal within minutes. Cardiac rupture may result from direct-impact force to the heart or pressure transmitted via venous channels; deceleration with lacerations at junctions between fixed and mobile structures (e.g., atriocaval disruptions); myocardial contusion, with subsequent necrosis and rupture; and broken ribs or sternum penetrating the heart. The most common chambers ruptured are the right atrium and ventricle, followed by the left atrium and then the left ventricle.27,28 A coexistent pericardial laceration allows free hemorrhage into the pleural or peritoneal cavity. Those who reach the hospital alive typically have a pericardial effusion and may develop pericardial tamponade. A characteristic mill-wheel murmur, the bruit de moulin, may be heard.
Pericardial Injury
Pericardial tears may result from direct thoracic impact or from an acute increase in intraabdominal pressure. The tears most commonly occur on the left (64%), paralleling the phrenic nerve; the diaphragmatic surface (18%), right pleuropericardium (9%), and mediastinum (9%) are the next most frequent sites.27 Herniation of the heart through a large tear may be associated with significant cardiac dysfunction. A pericardial rub may be detected on physical examination. The chest radiograph may demonstrate pneumopericardium, displacement of the heart, or bowel gas in the chest. Echocardiography or CT may be required to confirm the injury. In a stable patient, a subxiphoid pericardial window should be performed, followed by sternotomy in the presence of hemopericardium or a visible pericardial tear. An unstable patient may require EDT. Pericardial lacerations should be repaired, but large holes that cannot be closed primarily should be left widely open to prevent future cardiac herniation. A late complication is the postpericardiotomy syndrome, manifested by fever, chest pain, pericardial effusion, a pericardial rub, and ECG abnormalities; this is adequately treated with antiinflammatory agents.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree