Fig. 77.1
Chest x-ray of a 45 year old male a victim of blunt trauma demonstrating left sided tension pneumothorax with rib fractures
Question
What is the diagnosis and what should be the next step of management?
Answer
Tension pneumothorax and needle decompression with subsequent tube thoracostomy insertion.
Evacuation of pleural air is the most important first step in a tension pneumothorax and can be done via needle decompression or catheter drainage [1]. After a tube thoracostomy was placed, 100 mL of blood was evacuated from the chest. The chest tube was placed to suction through a pleur-evac system. A post procedure chest x-ray was obtained which showed the chest tube in proper posterior-apical position with the last drainage hole within the chest cavity. The patient was stabilized and a chest CT was performed which revealed multiple rib fractures, consistent with a flail chest segment, multiple areas of lung contusion, and bilateral basilar pleural effusions.
The patient’s inspiratory effort became poor and he had multiple episodes of desaturation. An arterial blood gas showed a pH 7.27, CO2 55, O2 65, HCO3 25. The patient was subsequently intubated and placed on volume control mechanical ventilation, tidal volume 400 mL, respiratory rate 18, pressure support 10, PEEP 8, FIO2 100 %. Fluid balance was carefully monitored during his intubated status and protective lung ventilation was maintained.
The patient required IV pain control with placement of an epidural catheter for pain associated with his multiple rib fractures and flail segment. Over the next few days the pain was well controlled, hypoxia associated with lung contusions improved, daily spontaneous breathing and awakening trials were performed and the patient was successfully extubated. Chest tubes were removed after complete resolution of his pneumothorax and hemothorax and the patient was subsequently discharged to a rehabilitation center.
Principles of Management
Pneumothorax
Pneumothoraces associated with trauma can be diagnosed by clinical exam and radiological studies. Patients often present with shortness of breath, chest pain, cough, and tachypnea [2]. Clinical presentations of tension pneumothorax also include chest pain, dyspnea, tachypnea, and hypoxia, but additionally present with jugular venous distention, contralateral tracheal deviation, subcutaneous emphysema, and hyper-resonance to percussion [3]. High clinical suspicion for tension pneumothorax should lead to immediate needle decompression and then tube thoracostomy insertion. Diagnosis of pneumothorax can be done with chest x-ray, ultrasound (Videos 77.1 and 77.2) or chest CT2. Small spontaneous pneumothoraces, not associated with trauma, can be observed clinically and a chest tube can be deferred unless the patient becomes symptomatic or the pneumothorax expands [4]. Traumatic pneumothorax should be treated with closed tube thoracostomy (chest tube) placement.
Hemothorax
Once there is suspicion for a hemothorax, on either radiological findings or clinical concern, a tube thoracostomy should be performed. Diagnosis can be confirmed with plain chest films, looking for a meniscus sign of fluid blunting the costo-phrenic angle or diaphragmatic surface (Fig. 77.2). Approximately 400–500 mL of fluid is required to cause blunting of the costo-phrenic angle in a traditional upright chest x-ray. Additionally, ultrasound can be useful to detect fluid; however, the precise quantitative measurement of the amount of blood in the pleural cavity is often user dependent. Finally, computed tomography with the administration of intravenous contrast of the chest allows for a global picture of thoracic anatomy and can be useful in patients who may also have to be ruled out for aortic injury and operative planning for repair.
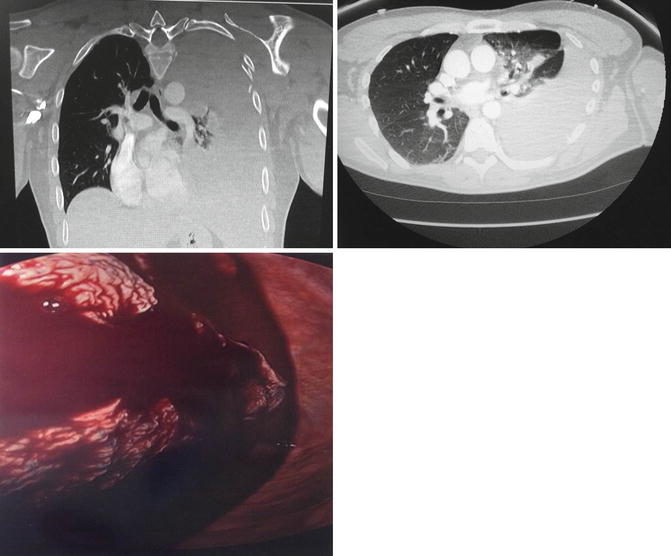
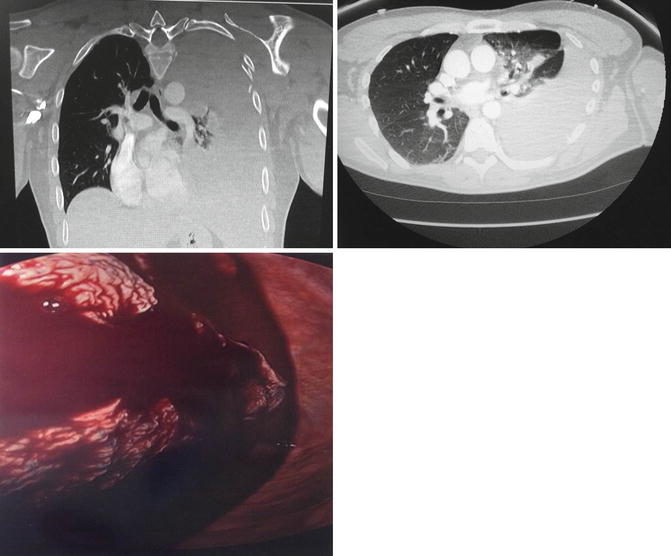
Fig. 77.2
Patient with a retained left Hemothorax- Was taken to the operating room 4 days following initial trauma. A video-assisted thoracoscopy was performed. Intra-operative pictures confirm the presence of a large hemothorax
If the initial placement of a chest tube drains more than 1500 mL within a 24-h period or demonstrates a continuing bloody output for more than 150–200 ml per hour for 4 h, massive hemothorax is diagnosed and a surgical intervention in the form of a postero-lateral thoracotomy should be considered for hemorrhage control [5]. Persistent retained hemothorax, as defined as a hemothorax that persists after chest tube insertion and attempted drainage procedures, should be treated with early video-assisted thoracoscopic surgery (VATS) rather than repeated attempted drainage with additional chest tubes to avoid long-term lung scarring, pleural thickening, and infection/empyema formation [5] (Fig. 77.2).
Rib Fractures
Rib fractures are the most common injury in blunt chest trauma and can occur in 50 % of cases [6]. Injury to the first 3 ribs usually requires high-energy trauma, fractures of fourth to eighth ribs are most common, and fractures of the ninth to twelfth ribs usually indicate the possibility of co-existing intra-abdominal injury. Clinical suspicion for rib fractures includes, splinting, localized pain, overlying skin changes including ecchymosis or subcutaneous emphysema, and/or respiratory distress. A paradoxical chest rise with inspiration and expiration is typically consistent with rib fractures involving multiple sites and ribs. Diagnosis can be made with plain films of the chest, but this method has sensitivity as low as 15 % [7]. Therefore, use of CT imaging of the thorax allows for confirmation of the diagnosis of rib fractures and 3-D reconstruction of the thoracic wall for potential operative planning [7]. The treatment of rib fractures includes adequate pain control and aggressive pulmonary toilet [8]. Typically the physiological derangement associated with rib fractures is predominantly due to the underlying lung contusion [9, 10].
Lung Contusion
Blunt chest trauma is involved in nearly one-third of acute trauma admissions to the hospital, and lung contusion (LC) (Fig. 77.3) is an independent risk factor for the development of acute lung injury (ALI), acute respiratory distress syndrome (ARDS), and ventilator-associated pneumonia (VAP) [9, 11]. The lung is also the second commonest organ involved in blast trauma-induced LC, which often has a peri-hilar distribution and carries a high risk of mortality [12]. When LC injury leads to hypoxemia severe enough to meet the definition of ARDS, the prognostic and economic impacts are significant. In a 2004 study of trauma patients, the incremental hospital cost per patient with ARDS ($36,713 or $59,633, respectively) was much higher than for patients without ARDS ($24,715) [13].
Fig. 77.3
Chest CT scan showing bilateral lung contusion-presence of involvement of the non-dependent lobes with evidence of trauma are indicative of lung contusion. Other pertinent differential diagnosis should include gastric-aspiration induced lung injury
The pathophysiology of pulmonary contusion and blunt chest trauma includes inflammation, increased alveolo-capillary permeability and pulmonary edema, ventilation/perfusion mismatching, increased intrapulmonary shunting, and a loss of compliance [14]. Treatment modalities outside of the standard treatment of other forms of lung injury such as a conservative fluid strategy, mechanical ventilation with lung protective strategy and analgesic management of associated rib fractures are currently under investigation.
Evidence Contour
Pneumothorax
Several areas of management of pneumthoraces still remain controversial. Traditionally, all sizes of post-traumatic pneumothoraces required chest tube drainage. However, a small pneumothorax in a clinically stable patient can be observed with repeat chest x-ray and a tube can be avoided unless the patient develops respiratory distress or the pneumothorax expands on chest plain film [5].
The use of smaller 14-Fr pigtail catheters has also been a new addition to the treatment algorithm in the management of pneumothorax. This procedure has been shown to reduce pain associated with chest tube placement as well as tube placement duration, and is equally effective at draining pleural air as larger, more traditional chest tubes [15].
The use of continuous negative pressure once the chest tube is placed, as well as the optimal timing for water seal prior to removal has also had some controversy. In patients without a continued air-leak, the chest tube can be placed to water seal and does not require negative pressure [16].
The routine use of chest x-rays after insertion as well as removal of chest tubes has also been investigated. Many institutions have created protocols that require a chest x-ray (CXR) after insertion of a chest tube. Newer studies are now finding that this routine study rarely changes the clinical course for the patient and clinical evaluation of the patient and tube drainage can alert the practitioner to problems that may exist [17]. Traditional protocols have centered on obtaining CXRs after chest tube removal. If a patient is not mechanically ventilated and has appropriate mental status to communicate symptoms of respiratory distress, a post-chest tube removal CXR is not required [18, 19].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







