121 Third Trimester Pregnancy Emergencies
• Preeclampsia, a disease of the third trimester of pregnancy, is characterized by a sustained elevation in blood pressure and proteinuria. Edema is common in patients with preeclampsia but is no longer considered to be necessary for the diagnosis.
• HELLP syndrome is a particularly severe form of preeclampsia associated with high maternal morbidity and characterized by hemolysis, elevated liver enzymes, and low platelet counts.
• Eclampsia is defined by seizures, usually in the setting of preeclampsia.
• In patients with severe preeclampsia and eclampsia, basic management involves support of maternal vital signs, control of hypertension, prevention and treatment of seizure activity, and close consultation with obstetrics colleagues to determine the appropriate disposition.
• Placental abruption and placenta previa are the most serious causes of vaginal bleeding in late pregnancy.
• Painful bleeding in late pregnancy is probably due to placental abruption. In contrast, when the vaginal bleeding is painless, the cause is more likely to be placenta previa.
• Ultrasound evaluation of third trimester bleeding is diagnostic for placenta previa, but placental abruption is diagnosed clinically because ultrasound detects only 25% to 50% of abruptions.
• Treatment of third trimester bleeding includes stabilization of the patient, assessment of fetal status with ultrasound and fetal monitoring, and consultation with obstetrics colleagues to determine the need for delivery.
Preeclampsia and Eclampsia
Epidemiology
First pregnancies are at greatest risk. Other risk factors include extremes of reproductive age, more than 10 years between pregnancies, multiple gestations, molar pregnancies, previous or family history of preeclampsia, underlying diseases (hypertension, diabetes, autoimmune or renal diseases, obesity), and thrombophilia (e.g., antiphospholipid syndrome, factor V Leiden deficiency, activated protein C resistance).1
Pathophysiology
Preeclampsia is a multisystem disorder of gestation. Its exact cause is unclear and several mechanisms have been implicated. The disease is thought to originate within the placenta, which for reasons that remain obscure, has inappropriately decreased perfusion. Hypoperfusion and multiorgan effects ensue in some patients as a result of decreased intravascular volume and endothelial vascular leakage causing increased interstitial volume, interstitial protein leakage, and vasoconstriction.2 Preeclampsia affects nearly every organ system.
Preeclampsia has long-term implications for the health of these patients. After delivery, women with preeclampsia are at increased risk for the development of chronic hypertension, cardiovascular diseases, and psychosomatic disorders.3
Presenting Signs and Symptoms
Patients with severe preeclampsia may have additional symptoms of organ involvement (Box 121.1),4 including significant edema, especially facial edema, and documented weight gain of more than 5 pounds per week. Findings ominous for severe preeclampsia include a blood pressure of 160 mm Hg systolic and 110 mm Hg diastolic or greater, visual disturbances (blurred vision or scotomata), severe headache, altered mental status, seizures (which defines eclampsia), hyperreflexia with clonus, severe epigastric or right upper quadrant pain on examination, retinal hemorrhage with exudates and papilledema (which is rare and more commonly indicates underlying chronic hypertension), bibasilar rales and evidence of frank pulmonary edema, oliguria, and petechiae and bleeding from puncture sites.
Box 121.1 Clinical Manifestations of Severe Preeclampsia
Differential Diagnosis and Medical Decision Making
The current classification of hypertension in pregnancy is divided into four categories: preeclampsia, gestational or transient hypertension, chronic hypertension, and preeclampsia superimposed on chronic hypertension (Box 121.2).5 In addition, occult renal disease can be manifested as proteinuria and associated hypertension.
Box 121.2 Classification of Hypertension in Pregnancy
The differential diagnosis of severe preeclampsia is broad and distinction may be difficult, particularly with concomitant HELLP syndrome.6 Thrombotic thrombocytopenic purpura (TTP) and preeclampsia can have identical findings of thrombocytopenia, hemolytic anemia, renal disease, and neurologic abnormalities. In patients with preeclampsia, the hypertension, proteinuria, and edema tend to precede the hematologic findings. In patients with TTP, they generally follow and are a result of the hematologic abnormalities. However, by the time that the patient arrives in the ED, these subtle distinctions may be almost impossible to delineate.
HELLP syndrome is characterized by peripheral smears showing schistocytes and burr cells, elevated LDH levels (>600 U/L), elevated liver enzymes (bilirubin >1.2 and aspartate transaminase >70 U/L), and low platelet count (<100,000).7 In addition, the abnormal laboratory test results in patients with HELLP syndrome can be seen in the other diseases noted in Box 121.3.
Box 121.3 Differential Diagnosis of Severe Preeclampsia with HELLP Syndrome
Acute fatty liver of pregnancy
Thrombotic thrombocytopenic purpura
Immune thrombocytopenic purpura
Antiphospholipid antibody syndrome
HELLP, Hemolysis, elevated liver enzymes, and low platelets.
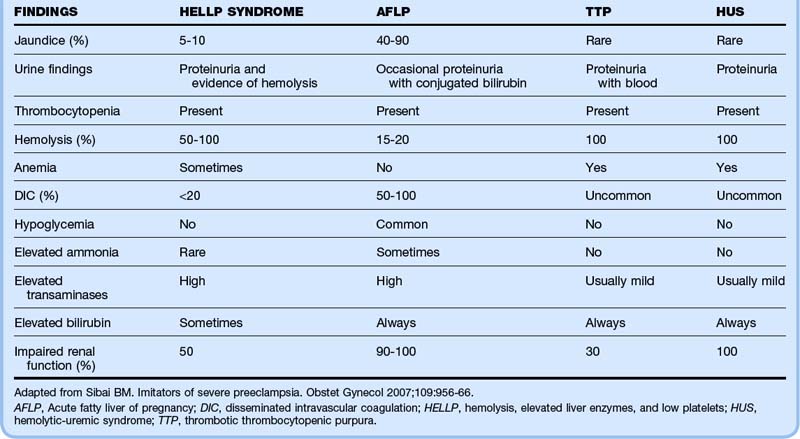
Table 121.1 shows the frequency of certain signs and laboratory values that may help distinguish between several of the key conditions that mimic severe preeclampsia with HELLP syndrome.6
![]() Red Flags
Red Flags
Preeclampsia and Eclampsia
Pain with a firm painful uterus suggests placental abruption, which is a complication in up to 10% of preeclamptic pregnancies.
Diagnosing preeclampsia may be difficult in patients with chronic hypertension complicated by chronic renal disease.
Seizures in pregnant patients do not always herald eclampsia, and other structural, toxic, and metabolic causes should be considered.
Both thrombotic thrombocytopenic purpura and preeclampsia can have the identical findings of thrombocytopenia, hemolytic anemia, renal disease, and neurologic abnormalities. In patients with preeclampsia, the hypertension, proteinuria, and edema tend to precede the hematologic findings, and in patients with thrombotic thrombocytopenic purpura, they generally follow and are a result of the hematologic abnormalities.
![]() Documentation
Documentation
Preeclampsia and Eclampsia
Pregnant women being evaluated should have their blood pressure documented; any elevation needs to be addressed. A complete history should include symptomatic clues (e.g., headache, vision changes, abdominal pain) identifying causes of the elevation.
Review of records may indicate that the elevation is chronic and that the patient is being monitored for this finding.
If the blood pressure is not dangerously high and no other evidence of preeclampsia is present, it may be addressed by making arrangements for close outpatient follow-up.
Documentation should include completion of appropriate laboratory testing.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree