Chapter 9 The two primary patterns of torso dysfunction
Altered function in the posturomovement system is observable in the manner in which we relate to gravity. The pelvis, in housing the centre of gravity of the body plays a central role in posturomovement control and its position when standing is the key to good or faulty postural alignment.1 Small shifts can exert significant changes throughout the body.
While each person with back pain has an individual presentation; in general, the altered neuromuscular responses fall into certain predictable, common patterns of response which can be distilled into the two primary pictures of torso dysfunction. These are characterized by a changed sagittal plane spatial position of the pelvis in standing and corresponding alterations in the postural alignment of the body in relation to the line of gravity (see Ch. 8). They afford a simple clinical classification system and underlie a working model or paradigm to help understand the development and perpetuation of posturomovement disorders responsible for many musculoskeletal pain syndromes. Before examining these two proposed primary patterns more closely, it is useful to consider clinical classification systems suggested by other authors.
The case for a clinical classification based upon underlying motor control impairments
The premise that impairments in the way people posture and move are the underlying factor driving the patient’s presenting musculoskeletal pain and dysfunction is central to the approach of this model and is one shared by Sahrmann,2,3 O’Sullivan,4,5 and Dankaerts et al.6 Based upon this premise, those authors have argued for a clinical classification system to assist in the diagnosis and management of chronic non specific low back pain disorders (CNSLBPD). They advocate classification into clinical subgroups which are determined by ‘the alignment, stress, or movement direction that most consistently reproduces pain.3 When the mechanism or cause of a disorder is known treatment of the cause is usually considered more effective.6
Sahrmann3 arrived at five diagnostic categories for CNSLBP based upon the direction of movement causing the pain, which in order of her observed frequency are:
Sahrmann says: ‘The diagnosis is designed to direct the intervention. The primary strategy for an intervention program is eliminating the alignment stress or movement in the symptom producing direction. The program does not emphasize movement in the opposite direction, except where the alignment impairment is excessive’.3
Similarly, O’Sullivan7,8 and Dankaerts et al.,6 no doubt influenced by Sahrmann, suggest a mechanism based classification in the diagnosis and treatment of CNSLBPD. They also proposed five distinct yet different clinical patterns based upon a specific direction of motor control impairment which aggravated the pain, and the hypothesized mechanism underlying the pain disorder6. These patterns were originally described by O’Sullivan in relation to ‘instability’ of the lumbar spine:7,8
O’Sullivan4,5 further elaborated his classification based upon the mechanism underlying the disorder, proposing that three broad subgroups of NSCLBP disorders exist. The directional patterns appear to be a subgroup of Group 3.
This author concurs with O’Sullivan’s three broad subgroups and that maladaptive movement patterns are responsible for chronic abnormal tissue loading and ongoing pain. However, this author considers that movement and control impairments are not necessarily exclusive, but generally co-exist in some measure, albeit with one dominating, depending upon the subgroup classification to be presented in this chapter (see also Ch. 8). The patterns of altered neuromuscular response (movement impairments) may well be the heightened responses of chronically dysfunctional movement pattern behavior and indicative of the severity of pain, tissue irritability as well as the stage of the disorder. It is suggested that clinically, symptom reproduction with movement is not necessarily always achieved nor a reliable guide to the underlying reason why that person’s movement problems have developed and are further feeding his pain picture. Nor is it necessarily always desirable to reproduce the pain as the testing in doing so can be potentially very provocative.
The two primary pictures of torso dysfunction
Observing the habitual standing posture provides a convenient ‘road map’ of the way in which the patient has adaptively organized herself against gravity.
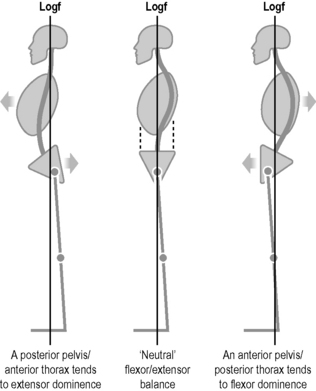
In the sagittal view optimal posturomotor control has the pelvis balanced within the line of gravity, but when disturbed, the pelvis is postured either more anteriorly or posteriorly from the line of gravity (Fig. 9.1 & also Fig. 8.4).
This constitutes the basis of the two primary pictures of dysfunction – the pelvic crossed syndromes. When pelvic alignment changes so do the spinal curves in a predictable fashion. The thoracolumbar junction is considered the inflexion point between the thoracic kyphosis and the lumbar lordosis and through which the line of gravity passes.9 Its position has a marked effect on the distribution of the intersegmental rotations of the lumbar vertebrae and upon the magnitude of the sagittal moments carried by the passive spine.10 When more anterior, a constant extension torque ensues; when more posterior, a flexion torque results.11
Roussouly et al.12 comment ‘the majority of degenerative disease occurs in spines that are well aligned in the coronal plane but exhibit highly variable morphology in the sagittal plane’. They performed a significant radiographic study examining the sagittal alignment of the lumbar spine in a cohort of 160 asymptomatic subjects. They found that ‘normal’ varied, and classified these variations into four groups. These subgroups resonate well with clinical impressions and so the features of each are described:
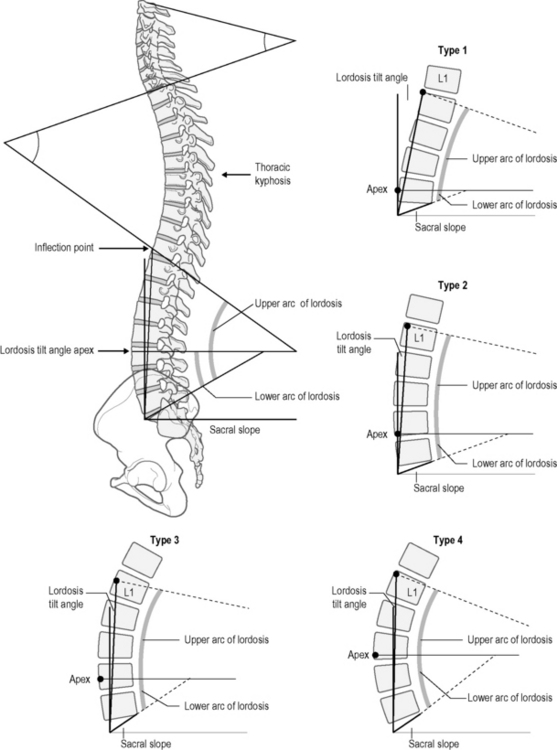
Fig 9.2 • The four lordosis types according to Roussouly et al. 2005. Change in the sacral slope effects reciprocal change in the lordosis.
While demonstrating that sagittal alignment ‘normally’ varies significantly, the authors found the least common was Type 2 and the most common was Type 3 (construed as normal); where the apex of the lordosis was located on average in the centre of the L4 body. They also confirmed that the characteristics of the lumbar lordosis are most dependent on the orientation of the sacral slope and the pelvis. They comment that there appears to be an association between loss of lordosis and an anterior shift of the vertical axis and the development of symptomatic back pain. Further, they comment that they have noticed that patients with symptomatic disc herniations are most commonly classified as Type 1or 2; patients with spinal stenosis are most commonly classified as type 4 and that they rarely see patients with significant complaints who are classified as Type 3! A further study13 compared the native sagittal alignment of patients with spondylolysis and low grade spondylolisthesis against a control group. They found increased lumbar lordosis, but less segmental extension between L5 and S1 than in the normal population. Reporting a later related study14 in patients with lumbar degenerative diseases, they commented that previous data suggested that patients demonstrated less distal lordosis, more proximal lordosis and a more vertical sacrum; while that particular study found the loss of lordosis and a decreased sacral slope were significant. Their findings are important in corroborating the clinical impressions which underpin the pelvic crossed syndromes. Of particular significance are Type 1 with a reduced lordosis and Type 4 with an increased, albeit more cephalad or high lordosis.
In addition, Smith et al.15 reported a photographic study examining sagittal alignment in 235 adolescents and also identified four subgroups – neutral, hyperlordotic, flat and sway. A higher proportion of the adolescent group that had never had back pain was in the ‘neutral’ subgroup.
The Pelvic Crossed Syndromes
These paradigms have elaborated upon the model of the Pelvic Crossed Syndrome described by Professor Vladimir Janda.16–18 Attempts to validate the relationship between The Pelvic Crossed Syndrome as described by Janda and back pain have not been successful.19 While the Pelvic Crossed syndrome as he described it certainly applied to some of this author’s patients, it did not completely fit the picture for many, or at all for others. It took some time for this author to recognize the other patterns.
These two syndromes form the basis of a proposed clinical classification system.
It is important to appreciate that not all patients will demonstrate the pure pelvic and related picture. Some will show some tendency, and others will exhibit a variable mixture of the two with a dominant tendency. Understanding the features of each helps understand the patient in front of you – possibly a Mixed Syndrome (see Ch. 10).
Posterior Pelvic Crossed Syndrome (PPXS)
The pelvis is back
Here the neuromuscular system is generally more switched on but in an abnormal manner of relative systemic global muscle system (SGMS) ‘overdrive’, with a tendency for axial extensor muscle system dominance. However, this extensor hyperactivity is regionally patchy and associated and related under activity of the deep system (SLMS). In its purest form it may be more common in males. The patient ‘looks up’– the ‘pseudo warrior’ although he is tense, unyielding, generally tight and stiff, with poor selective control of movement within the torso (Figs 9.3–9.6).
Sagittal alignment characterized by:
Table 9.1 Altered myofascial length/tension contributing to PPXS
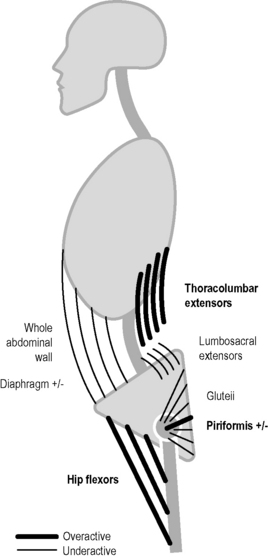
As Janda17 described the ‘cross‘, there is an oblique relationship between the iliopsoas/hip flexors and erector spinae which are overactive/tight with poor control of eccentric lengthening. The spatially oblique gluteals and abdominals are weakened resulting in an anterior pelvic tilt, increased lordosis and a slightly flexed position of the hip (Fig. 9.3; Fig. 9.6). If the lordosis is deep and short the imbalance is principally located in the pelvic musculature. If it is shallower but longer extending into the thoracic area the imbalance is more marked in the trunk musculature.17,23 Clinically, the latter appears more common and many also have quite bulky buttocks. Janda noted that those who stand with an opened lower thoracic aperture have a shortened diaphragm in association with underactive abdominals with decreased excursion in breathing.23 Janda also noted that hamstrings could be tight in this syndrome either as a compensatory mechanism to lessen pelvic tilt or possibly as a functional compensation for the inhibited glutei.17 He also noted that an imbalance can exist in the lateral pelvic muscles where a weak gluteus medius can be compensated for by overactivity and tightness in the ipsilateral quadratus lumborum and tensor fascia latae. An increased thoracic kyphosis and further compensatory increase in the cervical lordosis develop in efforts to balance the body and keep the head and eyes in the upright position.17
Toppenberg and Bullock24 examined lumbopelvic muscle lengths and their interrelationships in healthy adolescent females and found significant positive correlations between shorter (by implication overactive) erector spinae and iliopsoas and rectus femoris with a tendency for longer abdominals (by implication weaker) in association with longer gluteals and shorter iliopsoas muscles. They concluded that the pattern of length relationships which constitute the pelvic crossed syndrome as described by Janda can be seen in normal pain free adolescent females. This study lends weight to the premise that movement dysfunction is present and observable before pain appears. A prospective study would be nice in determining which subjects went on to develop pain syndromes.