Chapter 10 Clinical posturomovement impairment syndromes
Changed muscle activation patterns produce altered alignment of the body segments against gravity. Observing the patient provides information about the more common patterns of posturomovement dysfunction. Chapter 9 dealt with the two primary pictures of torso dysfunction which underlie all the clinical syndromes. These provide a clinically useful classification system guiding assessment, diagnosis and therapeutic care. The presence of these syndromes result in altered stresses on the joints and soft tissues and the predictable development of various pain syndromes in time. Diagnosing the ‘underlying mechanism driving the disorder’1 rather than the often spurious diagnosis based upon pathology helps inform more rational treatment interventions.
Sagittal view
The three pelvic syndromes and the common upper body posturomovement dysfunction:
Coronal view
Layer or Stratification Syndrome. Described by Janda3–5 this describes the commonly altered muscle activation patterns in the flexor and extensor systems.
Mixed Syndrome (MS)
Clinically, this is perhaps the more common presentation. Appreciating each primary syndrome separately helps see the composite presentation and the relative underlying influence of one. The two basic pictures of dysfunction in the pelvic crossed syndromes are reflective of the developmental prowess or otherwise of the individual which not only includes the early developmental history but also subsequent influences. Psychological occupational and recreational factors all impact upon the primary picture of dysfunction and variously contribute to the development of the MS pictures in some patients. Unfortunately, poorly conceived therapeutic interventions and fitness industry programs appear to be responsible for the increasing prevalence and most flamboyant examples. The important role that the systemic local muscle system (SLMS) plays in the proper control of movement is generally not well understood. Instead, many myths abound and in particular with regard to ‘core control’ (see Ch. 6, Part B). In pursuit of this, many are entrenching central torso ‘cinch patterns’ and dysfunctional breathing patterns – a ‘gym junkie syndrome’ is becoming apparent (see Ch. 11, Sport and Recreation; Training and the fitness industry).
In general terms, the shared common dysfunction in the primary pictures consists of:
However, within the common patterns above, variations occur in accordance with each primary syndrome and are summarized in Table 10.1.
Table 10.1 The cardinal features of altered function in the two primary pictures of dysfunction
| PPXS | APXS | |
|---|---|---|
| Pelvis position re line of gravity | Posterior | Anterior |
| Thoracolumbar position re line of gravity | Anterior | Posterior |
| Flexor/extensor system tendency | Extensor | Flexor |
| Central cinch pattern | CPC | CAC → CCC |
| Suspected principal regional dysfunction | Thoracolumbar > pelvic? | Pelvic > thoracolumbar? |
| Pattern of hip/thigh muscle restrictions | Anterior > posterior | Posterior > anterior |
‘Central conical cinch’ (CCC) behavior and ‘butt-gripping’6 are probably the most consistent distinguishing traits which unite the two primary pelvic syndromes in the MS. This results in a hyperstabilized central torso yet poorly stabilized lumbopelvic region with variable patterns of inferior pelvis/hip restriction.
Central cinch patterns (CCPs)
CCPs refer to the seemingly reflexive and somewhat obligatory bilateral neuromuscular responses which are observed to occur in posture and movement around the central torso. In most instances, their early activation means they become the postural set which initiate and support the ensuing movements. They hyperstabilize the central torso in one or more planes. They appear to be a response to reduced SLMS control and a compensation for inadequate proximal girdle control particularly in the pelvis. They are further magnified in the presence of a ‘dome’ (Ch. 8, Thoracic dysfunction). For whatever reason, the response is more dominant above the belt line than below. The patient finds it difficult to inhibit these responses and in essence only learns how to when better SLMS control is established, including control of the proximal limb girdles along with proper diaphragmatic breathing and better co-activation between the axial muscles.
Central posterior cinch (CPC)
CPC refers to the observed pattern of bilateral reflex overactivation of the superficial muscle groups which form a dense ‘fan’ which spans posteriorly from approximately the level of the mid/upper lumbar spine extending upwards to cover the lower pole of the thorax (Fig. 10.1). These work in synergy as a reflex ‘mass response’ with associated underactivity in the abdominals. Janda7 considered that a clinically found muscle imbalance between different muscle groups is probably the result of a combination of both reflex and mechanical mechanisms. Regional extensor system hyperactivity may serve to inhibit the abdominals mediated by Sherrington’s Law of reciprocal inhibition2 or conversely, SLMS system dysfunction, abdominal underactivity and changed axial alignment creates the loading torque such that the CPC activity is necessarily facilitated. The presence of a ‘dome’ and generally reduced extension can mean that the CPC represents the region of ‘active’ extension. This can be readily observed when the patient simply lifts his head up in prone (see Fig. 8.18). The response is also a common compensation in forward bending when lumbopelvi-femoral control is decreased.
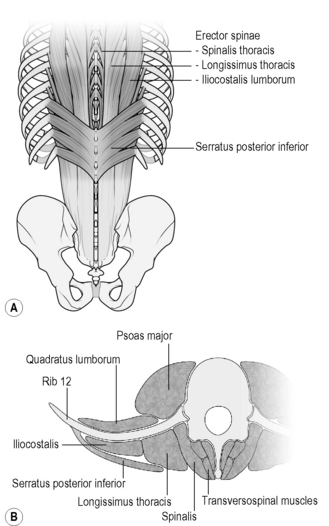
Clinically, the superficial posterior thoracolumbar muscle groups are usually but not always bulky, tender and tense with trigger points commonly found. Clinical impressions suggest they include (Fig. 10.2):
To a greater or lesser extent, practically all patients with spinal pain and related disorders can be observed to activate extensor dominant CPC patterns in posturomovement control. They are obligatory and particularly evident in the PPXS group, less so in the MS and intermittent in the APXS group. This is a reasonably constant response which the patient finds hard to inhibit. Eccentric lengthening is poor hence little adaptability/variability for postural control. The bilateral activation serves to ‘fix’ the lower pole of the thorax and the thoracolumbar spine in a ‘central’ position holding the region in a sagittal orientation and importantly, limits flexion, lateral and rotary movements and weight shifts through this region of the torso (Fig. 10.3). Neural irritability through segmental hypomobility further increases the tonus of the thoracolumbar extensors feeding into a vicious pattern generating cycle as the mid/low lumbar levels are further required to compensate.

Fig 10.3 • A central posterior cinch fixes the spine centrally limiting lateral weight shift. The subject is attempting to ‘grow one elbow to the ceiling (see Ch. 13). Note the lack of adaptive eccentric lengthening in the (L) erector spinae and probably psoas and the poor weight shift through the pelvis.
Central anterior cinch (CAC)
CAC refers to the observed pattern of bilateral reflex overactivation of the anterolateral abdominal group above the level of the umbilicus. Given their superior attachments extend over the entire anterolateral surface of the inferior pole of the thorax; their overactivity has a significant influence. The bilateral activation creates a flexor torque, holding the central torso in a more flexed sagittal orientation thereby limiting extension, lateral and rotary weight shift and movements. Most significant is the narrowing of the inferior thoracic opening and limitation of the diaphragm’s important functional role (Fig. 10.4). This ‘reflex withdrawal’ action is also initiated with anxiety, stressful states and fear (see Ch. 6, Part A). Janda11 found that in healthy children and spastics with good postural development, unresisted and resisted knee extension in supine and sitting produced only slight or no activity of the abdominal muscles. However, in those spastic children with a hypotonic trunk and bad posture, the activity of the abdominal muscles increased considerably in sitting during this test. Questioning whether this was the result of an altered reflex mechanism or due to possible mechanical stabilization dysfunction in these children, he examined healthy children with evident hypotonia of the trunk and also found a remarkable increase in their abdominal activity in sitting. The entire pattern of knee extension in this group was accompanied by a ‘simultaneous backward tilt of the pelvis and a pronounced lumbar kyphosis and a curling movement of the whole trunk’. He surmised that altered reflex mechanisms were operant. It is interesting to note that low tone, postural collapse, CAC strategies and a tendency for ‘total flexion patterns’ (Ch. 8, p. 181) are all features observed in those classified as APXS. O’Sullivan et al.12 found that patients with CLBP had difficulty preferentially activating the deep abdominals with a tendency to higher levels of upper rectus abdominis activity. The CAC postural response is the obverse of that found in the normal state where the EMG onset of the upper region of transversus abdominus has been shown to occur later than that of the lower and middle regions in response to perturbation.13
CAC strategies are obligatory in ‘pure’ presentations in the APXS group and also predominant in those in the MS group but do not occur in the ‘pure’ PPXS group. SeeFigures 4.9, 8.28, 8.38, 9.12, 9.15.
Central conical cinch (CCC)
CCC refers to the combined activation of the CPC and CAC strategies and can subsequently develop in both primary pictures of dysfunction to create a MS. This simultaneous increased reflex activation serves to ‘squeeze’ the inferior region of the lower pole of the thorax and conceptually convert it into a conical shape. The lower pole of the thorax extending into the upper lumbar spine is hyperstabilized in all three planes. This is akin to a self inflicted functional ‘straight jacket’. Rather than the ‘body cylinder’ (Ch. 6, p. 93) being open in the centre, it becomes constricted in posturomovement like squeezing a tube of toothpaste in the centre – the body cylinder now resembles an ‘hourglass’ (Figs. 10.5 & 8.38). This regional hyperstabilization coupled with inadequate and imbalanced lumbopelvic control renders the mid/low lumbar spine levels more vulnerable.
CCC strategies are seen intermittently in those classified as APXS and consistently in those in the MS based on either a primary underlying APXS (Fig. 10.6) or PPXS (Fig. 10.7).
Co-contraction of the superficial muscles was described by Radebold et al.14 in 2000 and is being increasingly reported in the literature.15,16 In an editorial on muscle function and dysfunction in the spine, Cholewicki et al.17 note that while there is consensus that the muscle activation patterns exhibited by patients with low back pain are different to healthy subjects, the interpretations of such findings are divergent. Van Dieën et al.18 analyzed the literature with respect to the changed activation of the lumbar extensor muscles derived from studies adopting the pain–spasm–pain model and the pain adaptation model. They found neither of the two models was unequivocally supported in the literature and proposed an alternate model which suggested that the altered trunk muscle recruitment is a functional adaptation to limit noxious tissues stress by limiting range and providing stabilization to the spine (Ch. 7 ‘Is the altered motor behavior observed in people…’ p. 160) An appreciation of the central cinch patterns may help provide explanations for the diverse findings in the literature. They represent evolving maladaptive responses which contribute to the development of pain syndromes and which become further enhanced and entrenched in the presence of pain. Pain tends to facilitate activity in SGMS muscles and inhibit activity in SLMS muscles.
Overall effect of CCPs
The CCPs create significant impediments to healthy torso control as follows:
‘Butt-gripping’ further affects function in ischial swing and pelvic floor myomechanics
The two primary pictures of dysfunction result in imbalanced control of pelvic tilt (Ch. 6, Part B) and the ability of the ‘ischial swing’ to adjust for weight shift in both the sagittal and frontal planes.
Clinically, in the APXS picture the pelvis predominantly shifts anteriorly and swings into posterior tilt reducing demand for postural activity of the gluteal group hence they are not well developed and show the signature ‘saggy bum’ or ‘no bum’ (Fig. 10.8).
In the primary PPXS picture the pelvis is more posterior and swings more into anterior tilt from more dominant erector spinae and psoas activity and poor abdominal activity. Although Janda described the glutei as ‘weak’ in his pelvic crossed syndrome,3–5 clinically this is probably more the lateral glutei as most are observed to have well developed buttocks as could be expected in the necessity for an antigravity role in countering the anterior pelvic tilt. Increased hamstring activity is also likely.5
Symptomatic of the MS is the adoption of more pronounced ‘butt gripping’ strategies in the PPXS group to help bring the pelvis forward and counter the activity of psoas. Described by Lee,6 ‘butt gripping’ posteriorly tilts the pelvic girdle and flexes the L4/5 and L5/S1 joints and is associated with intrapelvic postural change and narrowing of the inferior pelvis. Clenching the buttocks involves a synergy of gluteus maximus with the deep obturator group and the pelvic floor muscles (PFM) and hamstrings. The buttocks are more developed and the hips are externally rotated. Lewit20 notes the synergistic relationship between the PFM and gluteus maximus in helping to control the anal sphincter.
Clenching the buttocks helps explain why those who appear to be extensor dominant and classified as PPXS show a proclivity for posterior tilt and flexion over the lower lumbar levels while still demonstrating dominant extensor activity in the trunk (Figs. 10.9 & 10.10). While bringing the pelvis more forward and neutralizing the hip flexion action of psoas it probably shunts psoas’ effect more into the spine, locking the thoracolumbar junction more forward in extension. Reduced eccentric lengthening of psoas during lateral weight transfer reduces postural adjustment through the thoracolumbar spine.
Increased buttock development and/or gripping in a MS from a primary APXS picture is more likely to result from habit, specific exercise endeavors and training effect (Fig. 4.4).
The prevalence of MS and APXS syndromes point to an increasing incidence in the population where more and more of the pelvis assumes a position of more consistent posterior tilt, sacral counternutation and inferior bowl ‘closure’. Stress urinary incontinence (SUI) has been associated with increased PFM and external oblique activity21 (CAC) and altered recruitment, endurance and strength of the PFM.22 Posturomovement wise the ability to close and in particular to open the inferior pelvic bowl is very important. Failure to re-educate eccentric PFM control in functional pelvic movement patterns may help explain why specific PFM training is commonly associated with improvement rather than cure and the benefits are not necessarily maintained long term.23
Lateral shift or ‘list’ patterns of the trunk
These are generally an acute or subacute manifestation of a chronic problem and tend to reoccur in times of exacerbation. Left untreated, the neuromyoarticular patterns become further entrenched and more chronic (Fig. 10.11).

Fig 10.11 • Chronic lateral shift pattern. Note the associated buttock clenching and posterior cinch behavior.
As explained, the development of the adaptive CCPs leads to varying forms of hyperstabilization around the thoracolumbar junction (T/L/J). Normal studies24 have shown that lateral translations of the thorax relative to the pelvis are significant with most lateral flexion occurring at L1 but that segmental rotation angles for lateral flexion were largest at L3/4 (6.2°); L4/5 (5.7°); L2/3 (3.9°). When movement cannot occur though the T/L/J, the lower levels become more vulnerable to trivial provocations over time. In response to an acute segmental joint dysfunction, the associated muscles go into spasm and the trunk posture shifts or ‘lists’. Lee6 describes this as a multisegmental rotoscoliosis of the thoracolumbar spine coupled with a lateral shift of the thorax relative to the pelvis with associated intrapelvic torsion, internal rotation of one hip and external rotation of the other. O’sullivan25,26
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree