CHAPTER 20 THE ROLE OF FOCUSED ASSESSMENT WITH SONOGRAPHY FOR TRAUMA: INDICATIONS, LIMITATIONS, AND CONTROVERSIES
Focused Assessment with Sonography for Trauma (FAST) has rapidly taken root in modern trauma care. FAST is an integral part of trauma algorithms, and is an important adjunct to the Advanced Trauma Life Support (ATLS) primary and secondary surveys. In 1997, the American Board of Surgery required the addition of ultrasonography into Accreditation Council for Graduate Medical Education (ACGME)–approved surgical training programs. The American College of Surgeons (ACS) has also incorporated FAST into the ATLS course and has sponsored multiple ultrasound training seminars.
FORMATION OF AN ULTRASOUND IMAGE
Proper visualization and accurate interpretation of an ultrasound image requires a basic understanding of ultrasound components, principles, physics, and terminology. The basic components of an ultrasound machine are listed in Table 1 and include the transmitter to send electrical signals to the transducer, the transducer to interconvert electrical energy and acoustic energy using the piezoelectric effect, the receiver to convert electrical signals into an image, and the monitor to display the image. An optional printer provides a hardcopy image.
Table 1 Components of Ultrasound Machine
| Component | Description |
|---|---|
| Transmitter | Sends electrical signals to transducer |
| Transducer | Interconverts electrical energy and acoustic energy by piezoelectric effect |
| Receiver | Converts electrical signals into image |
| Monitor | Displays image |
| Printer | Records hard copy of image (optional) |
There are three essential principles of ultrasonography (Table 2): the piezoelectric effect, pulse-echo principle, and acoustic impedance. Within the transducer, piezoelectric crystals expand and contract to interconvert electrical and mechanical energy, a process known as the piezoelectric effect. When an ultrasound wave contacts tissue, some of the signal is reflected and some is transmitted into tissue. The reflected waves bounce back and contact the crystals within the transducer, generating electrical impulses comparable to the strength of the returning wave. This is known as the pulse–echo principle. Acoustic impedance is the density of tissue multiplied by the speed of sound in tissue. The strength of the returning echo depends on the difference in density between the two structures imaged. Structures of different acoustic impedance (e.g., bile and gallstones) are relatively easy to distinguish from one another, whereas those of similar acoustic impedance (e.g., spleen and kidney) are more difficult to distinguish.1
Table 2 Essential Principles of Ultrasound
| Principle | Explanation |
|---|---|
| Piezoelectric effect | Piezoelectric crystals expand and contract to interconvert electrical and mechanical energy. |
| Pulse-echo principle | When an ultrasound wave contacts tissue, some of the signal is reflected and some is transmitted into tissue. These waves are then reflected to crystals within the transducer, generating electrical impulse comparable to the strength of the returning wave. |
| Acoustic impedance | Acoustic impedance is the density of tissue X speed of sound in tissue. The strength of the returning echo depends on the difference in density between the two structures imaged: structures of different acoustic impedance (e.g., bile and gallstones) are relatively easy to distinguish from one another, whereas those of similar acoustic impedance (e.g., spleen and kidney) are more difficult to distinguish. |
The basic physics of ultrasonography are important for good image formation, and terminology used for ultrasonography is listed in Table 3. Ultrasound waves are high-frequency (>20 kHz) mechanical radiant energy transmitted through a medium. The frequency (number of cycles/second) of medical diagnostic ultrasound is 2.5–10 MHz. As frequency increases, resolution improves, but penetration to deeper tissue decreases. Generally, the highest frequency transducer that produces the best resolution of the target organ is chosen (3.5 MHz for FAST). Common clinical applications of different ultrasound frequencies are listed in Table 4.
Table 3 Ultrasound Terminology
| Term | Definition |
|---|---|
| Ultrasound | High-frequency (>20 kHz) mechanical radiant energy transmitted through a medium |
| Frequency | Number of cycles per second (medical diagnostic ultrasound: 2.5–10 MHz) |
| Propagation speed | Speed at which wave travels through soft tissue (1540 m/sec) |
| Amplitude | Strength or height of wave |
| Attenuation | Decrease in amplitude and intensity of wave as it travels through medium |
| Absorption | Conversion of sound waves into heat |
| Scattering | Redirection of wave as it strikes rough or small boundary |
| Reflection | Return of wave toward transducer |
| Artifact | Error in imaging |
| Gain | Amplitude of returning waves based on tissue depth |
Table 4 Clinical Applications of Selected Transducer Frequencies
| Frequency | Application |
|---|---|
| 2.5–3.5 MHz | General abdominal |
| 5 MHz | Transvaginal, pediatric abdominal, testicular |
| 7.5 MHz | Vascular, soft tissue, thyroid |
The echogenicity of a structure is defined as the degree to which tissue echoes ultrasonic waves (generally reflected in ultrasound images as the degree of brightness). Tissues that reflect waves strongly will appear bright and are hyperechoic. Tissues that conduct ultrasound waves well are hypoechoic and are darker, while anechoic tissues conduct waves very well and appear black because essentially no waves are reflected back to the transducer. Isoechoic tissue transmits ultrasound similar to that of surrounding tissues, and is displayed with similar intensity (Table 5).1
Table 5 Terminology Used in Interpretation of Ultrasound Images
| Term | Definition |
|---|---|
| Echogenicity | Degree to which tissue echoes ultrasonic waves (generally reflected in ultrasound image as degree of brightness) |
| Anechoic | No internal echoes, appearing dark or black |
| Isoechoic | Having appearance similar to that of surrounding tissue |
| Hypoechoic | Less echoic (darker) than surrounding tissue |
| Hyperechoic | More echoic (brighter) than surrounding tissue |
TECHNIQUE
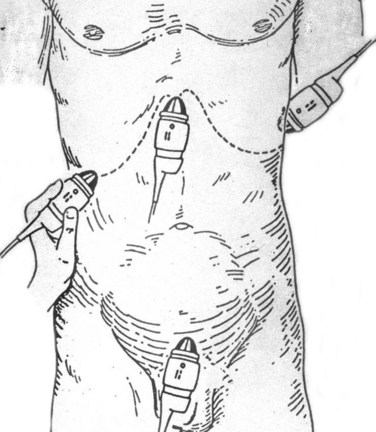
The patient’s identifying information is first entered to annotate the hardcopy ultrasound images. With the patient in the supine position, a liberal amount of ultrasound transmission gel is applied to the subxiphoid, left and right upper quadrants, and suprapubic areas. Using four transducer positions as shown in Figure 1, the pericardium and five dependent abdominal regions are examined for free fluid:
Although Morrison’s pouch was shown by Rozycki and colleagues2 to be the most sensitive for free intra-abdominal fluid, all five regions of the abdomen should be examined to maximize sensitivity of the test. Each area should be evaluated in two planes (longitudinal and transverse) with confirmation of positive regions using two views.
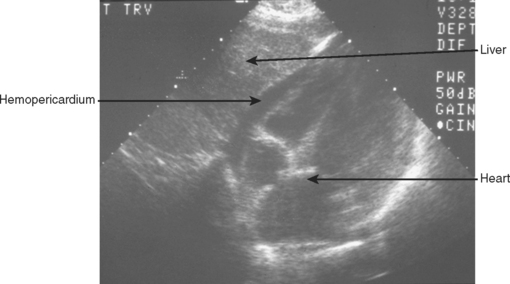
A 3.5-MHz convex transducer is oriented for sagittal sections and positioned in the subxiphoid area directing the transducer superiorly. Often, mild pressure on the transducer below the xiphoid toward the pericardial sac is required to visualize the heart. If this is unsuccessful, a left, parasternal, 4th or 5th intercostal view will be required. Obesity, rib/sternal fracture, subcutaneous emphysema, and a narrow subcostal angle may necessitate the parasternal view, and/or make this part of the examination indeterminate. Hemopericardium is detected by an anechoic band between the heart and the pericardial/diaphragmatic interface, as seen in Figure 2.
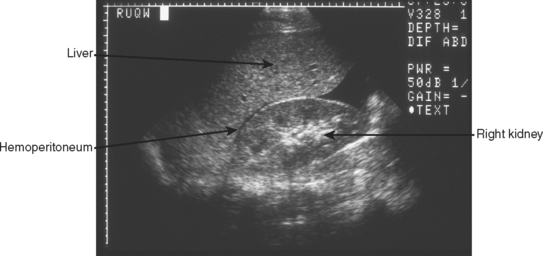
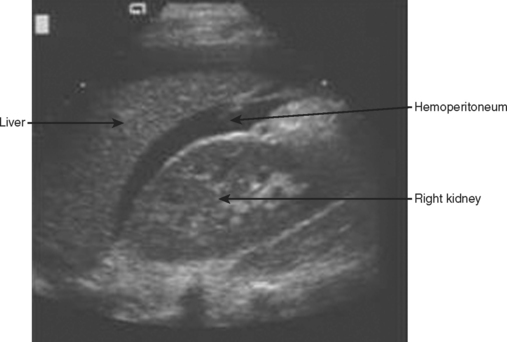
The right upper quadrant is then visualized by placing the transducer in the right mid to posterior axillary line, 11th intercostal space, in both longitudinal and transverse planes to visualize the right subdiaphragmatic and hepatorenal interface. An anechoic band between the liver and kidney as shown in Figure 3 identifies the presence of a minimal amount of blood, and a moderate hemoperitoneum is shown in Figure 4.
The left upper quadrant is examined by directing the transducer between the 10th and 11th ribs in the posterior axillary line. The right sub-diaphragmatic and splenorenal spaces are examined in two planes for free fluid, detected again by an anechoic band separating the two organs. A normal view of the hyperechoic left kidney/spleen interface is shown in Figure 5 and a positive left upper quadrant view is shown in Figure 6.
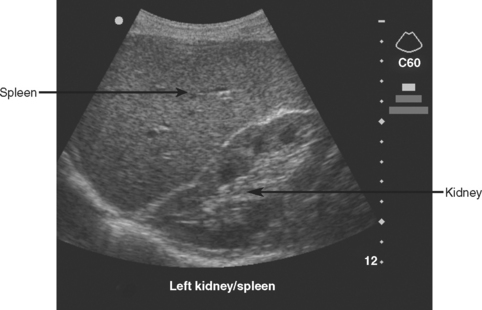
Figure 5 Normal sagittal view of left upper quadrant showing the hyperechoic left kidney/spleen interface.
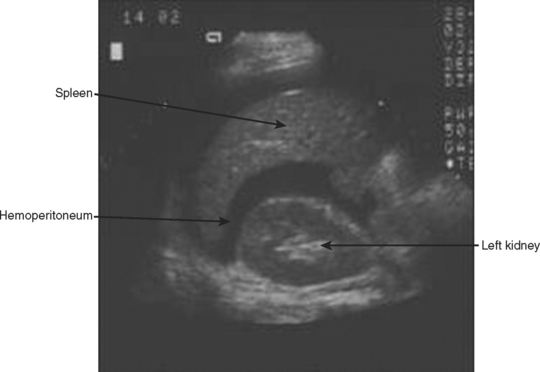
Figure 6 Sagittal view of left upper quadrant showing anechoic hemoperitoneum between left kidney and spleen.
Finally, the transducer is placed transversely just above the symphysis pubis and directed inferiorly looking for a coronal view of the bladder. This is ideally done before bladder catheterization to allow for a distended bladder, which optimizes ultrasound transmission and detection of free fluid posterior to the bladder in the rectovesical/uterine space. If a catheter has previously been placed, saline can be injected into the bladder through the catheter, or the catheter can simply be clamped and the pelvic view obtained after passive filling. Free intra-abdominal fluid is best detected on longitudinal plane in the rectovesical or rectouterine space by an anechoic band between the bladder and uterus or rectum as shown in Figure 7.
TROUBLESHOOTING
Difficulties in image formation are often solved with the simple techniques and strategy changes found in Table 6. A common solution to improve visualization is to apply a liberal amount of gel and reapply whenever the image quality is poor. An image that is too dark or too bright may require an adjustment in the gain. Poor visualization of deeper structures may also require a lower-frequency (2.5-MHz) transducer or an increase in time-gain compensation of the far field. A 2.5-MHz transducer may be necessary for the obese trauma patient. A 5-MHz transducer may increase the resolution of FAST in pediatric trauma patients, and a 7.5-MHz transducer is optimal for superficial structures (vascular, soft tissue). Subcutaneous emphysema poses a significant problem for ultrasound waves and alternate sites such as the parasternal position may be necessary for adequate visualization.
| Problem | Solution |
|---|---|
| Image too dark | Increase gain, apply more gel |
| Image too bright | Decrease gain |
| Poor penetration of waves | Use lower-frequency transducer, increase gain, subcutaneous emphysema (use alternate site), apply more gel |
| Poor image | Adjust gain, higher frequency transducer, subcutaneous emphysema (use alternate site), inadequate gel, begin with light pressure, slow movements |
| Disorientation | Confirm correct surface anatomy, orient transducer position, find known landmark (e.g., liver, kidney) |
| Obesity | Use lower frequency transducer |
| Infants | Use higher frequency transducer |
| Pericardial | Gentle pressure beneath the xiphoid directing cephalad, use alternate left parasternal window, and with slow movements look for motion of heart |
| Right upper quadrant | Move up or down a rib space, move posterior, deep inspiration |
| Left upper quadrant | Place transducer as far posteriorly as possible (on bed) and direct anteriorly, insert an oro/nasogastric tube to decompress stomach gas, deep inspiration |
| Bladder | Ensure full bladder, clamp catheter or fill bladder with saline |
INDICATIONS
FAST should be performed on all trauma patients who require evaluation of the chest and abdomen and cannot be cleared by physical exam. It should not delay a patient with penetrating abdominal trauma and hypotension or peritonitis from surgical exploration. In the case of penetrating thoracoabdominal trauma, FAST is valuable in early identification of pericardial tamponade or hemoperitoneum. This early application of FAST can direct operative intervention toward the body cavity most likely injured.
FAST is indicated in the evaluation of the unstable, multitrauma patient with an unidentified cause of hypotension. In this scenario, CT is contraindicated and FAST provides a rapid screening test without moving the patient from the resuscitation area. A positive exam is most helpful in this situation and Rozycki et al.3 reported 100% sensitivity and specificity (8 of 8 patients) for intra-abdominal injury in patients with a positive FAST and hypotension. McKenney et al.,4 in a prospective evaluation of an ultrasound scoring system, reported similar results. In this series, 10 of 10 patients with initial hypotension (systolic blood pressure <90), and 32 of 36 patients with subsequent hemodynamic deterioration and a significant hemoperitoneum on FAST had a therapeutic laparotomy. Farahmand et al.,5 in a study of 128 hypotensive patients suffering blunt abdominal trauma found FAST to be indispensable. The sensitivity of FAST for all injuries was 85%, for surgical injuries 97%, and 100% for fatal injuries. The authors found that FAST was able to virtually exclude surgical injury and detect surgical injury in 64% of positive studies. These studies strongly suggest that the combination of hemoperitoneum and hypotension mandate urgent laparotomy. A negative exam in the multi-injured, hypotensive patient should prompt further aggressive diagnostic and therapeutic evaluation.
The portable and noninvasive nature of ultrasound permits repeat FAST evaluations. A secondary ultrasound is most important in patients without obvious blood loss, a negative primary FAST, and continued hemodynamic instability despite ongoing resuscitation. Secondary FAST may also be performed on patients where CT is unavailable or delayed. Recently, Blackbourne and colleagues6 prospectively evaluated 547 patients undergoing both a primary and secondary FAST exam (within 30 minutes to 24 hours of initial exam). Excluding patients with hemoperitoneum and hypotension (who went directly to the operating room), the secondary FAST exam increased the sensitivity of detecting intra-abdominal free fluid.