INJURY TO THE SPINAL CORD
Few injuries produce the devastating disability of damage to the spinal cord. In the fully conscious adult, the presence of paralysis and anaesthesia after trauma immediately points to spinal cord injury. However, in the obtunded patient the diagnosis may be difficult. Similarly, incomplete cord damage is often misdiagnosed. For cord syndromes → p. 53.
Initial Management of Spinal Cord Injury
- Keep the patient calm, warm, splinted and immobile.
- Request orthopaedic advice.
- Record respiration and SaO2 (arterial O2 saturation). The onset of respiratory failure may be insidious.
- Monitor pulse, BP and ECG. Watch carefully for peripheral vasodilatation and the onset of neurogenic shock. Copious IV fluids may be required, but there is a potential for volume overload if too much is given.
- Catheterise the patient.
Anaesthetic help will be required for both respiratory failure and neurogenic shock.
Steroid Therapy
High-dose steroid therapy in patients with spinal cord injuries remains controversial. However, as the negative effects of steroids in acute head injury are now established, it would seem inadvisable to give steroids routinely to patients with spinal cord damage on current evidence.
Special Problems That May Accompany Injury to the Spinal Cord
Respiratory Failure
Intercostal muscle paralysis occurs with most cervical cord lesions. High lesions transect the phrenic nerve nucleus (C3–5) and are usually fatal. Even when the diaphragm is spared, vital capacity is greatly reduced and a compensatory tachypnoea occurs. The tidal volume and vital capacity should be measured if possible.
Paradoxical respiration is an important sign. As the diaphragm descends during inspiration to create a negative intrathoracic pressure, intercostal muscle paralysis allows rib retraction rather than the normal expansion. Deteriorating respiratory function (rate >35 breaths/min) is an indication for senior anaesthetic advice to consider the need for ventilation.
Neurogenic Shock
Impairment of descending sympathetic pathways in the spinal cord (i.e. cord damage at T6 or above) leads to relative hypovolaemia and bradycardia. Paralytic ileus often occurs in addition with a risk of vomiting and aspiration. Other injuries may have been sustained and can cause true hypovolaemia and either a bradycardia or a tachycardia. Any reduction of blood supply to the damaged cord will further impair its function. Hypotension from loss of sympathetic tone is one of the very few indications for therapy with vasopressor agents (e.g. ephedrine). Bradycardia usually responds to atropine. Symptoms last from several hours to several weeks depending on the level and the severity of the cord damage.
Retention of Urine
Bladder tone is lost immediately after spinal transection. Distension leads to ureteric reflux and renal damage. Intermittent catheterisation may be the treatment of choice in the spinal unit, but it is preferable to insert and retain a fairly thin catheter during the initial period of resuscitation and interhospital transfer. Catheterisation must be performed by an experienced member of staff using an aseptic technique.
Impaired Thermoregulation
The patient is unable to sweat and thereby lose heat at high ambient temperatures. More commonly, too much heat is lost at low temperatures because of a failure of cutaneous vasoconstriction. The environmental temperature should be near to normal body temperature if the patient has to be exposed for long periods (e.g. for the diagnosis and treatment of other injuries). At other times, insulation is used to prevent heat loss to a cooler environment. Core temperature must be measured regularly.
Associated Injuries
The signs of abdominal, pelvic and major limb injury may be masked by the motor and sensory loss. CT scan or ultrasound examination should be performed if there are external signs of abdominal trauma or if the patient is haemodynamically unstable. Abdominal swelling may occur with a full bladder or from a paralytic ileus. Severe swelling from any cause may splint the diaphragm. Multiple fractures are present in around 5% of patients with spinal injuries.
Localisation of Spinal Cord Damage
Twisting forces are most likely to cause fractures at the junction of mobile and fixed parts of the column, i.e. at C7–T1 and T12–L1. Upper thoracic spine injury may be associated with sternal fractures – massive forces attempting to buckle the thoracic cage. Direct blows are commonly associated with injuries elsewhere.
Partial transection of the cord may be inflicted by a knife or a bullet but complete separation is unusual. A twisting or bending movement resulting from indirect blunt violence is more common. This causes a combination of crushing and tearing which produces a mixed picture of neuronal damage. There is often total loss of neural continuity with complete distal motor and sensory loss.
Distal reflex activity may not be clearly related to the extent of cord section in the immediate post-injury phase. Complete section usually causes immediate flaccid paralysis with later return of reflex activity. Rarely, some reflexes are preserved throughout.
The level of cord injury may be difficult to determine because of the following:
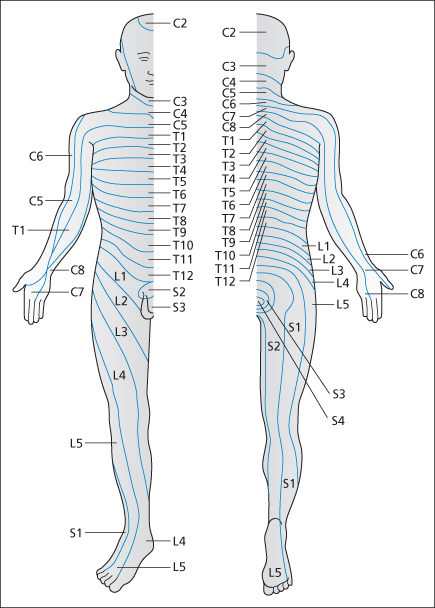
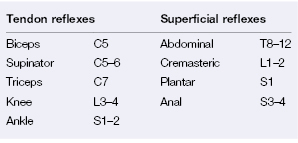
It is important to detect change in neurological status over time. Identify and document the lowest functional muscle groups and the extent of skin anaesthesia (→ Table 4.1 and Figure 4.1).
Table 4.1 Nerve roots supplying tendon and superficial reflexes
Delayed Improvement or Deterioration After Spinal Cord Injury
Spinal Shock
This is rare. After a cord injury, spinal concussion causes a generalised flaccidity below the level of the lesion. Reflex activity may initially be present but later disappears. Neurological signs begin to improve spontaneously within 8 h and the effects of the concussion are variably reversed within 48 h.
This diagnosis can be made only in retrospect. An initial finding of proximal paralysis with sparing of distal neurological function (e.g. sphincter tone) is likely to be associated with cord concussion and carries a more favourable prognosis. Concussion and permanent cord damage may coexist.
Late-onset Paralysis
Secondary deterioration can occur after spinal injuries in a similar way to the much more common complications of brain injury. Paralysis that develops hours after the incident is rare and is usually a result of cord ischaemia or oedema (causing infarction or vascular occlusion, respectively). An extradural haemorrhage may cause cord compression. Delayed signs are very unlikely to result from direct injury. Gentle handling, as described above, will not further damage a spine that has been subjected to forces sufficient to render it unstable. The doctor would be expected to be less violent than the injuring agent.
Cord Syndromes
Incomplete cord damage produces a number of discrete syndromes. Some degree of recovery is more likely than in complete lesions where there is no sign of any spinal cord function below the level of the injury. The mixed nature of the signs leads to misdiagnosis.
Lesser degrees of damage produce spinal cord contusions. There may be non-specific weakness, poor mobility and myoclonus. The diagnosis is usually only made on an MR scan. Recovery is usually slow but complete.
Central Cord Syndrome
This usually occurs in older patients with spondylitic spines following a relatively minor hyperextension injury. The spinal cord is compressed between the osteophytic vertebral body anteriorly and the stiff ligamentum flavum posteriorly. The more centrally situated parts of the corticospinal and spinothalamic tracts are the worst injured. These fibres supply the arms where the damage results in a flaccid (lower motor neuron) paresis. The legs are less affected with a spastic (upper motor neuron) type of weakness. The sacral fibres are often spared, so perineal sensation and bladder and bowel function may be normal.
Anterior Cord Syndrome
The anterior part of the spinal cord is usually injured by a mixture of bony encroachment and ischaemia. Typically, a flexion–rotation force causes a dislocation or a compression fracture of the vertebral body with accompanying anterior spinal artery compression. There is loss of power as well as reduced pain and temperature sensation below the lesion.
Traumatic Herniation of a Cervical Vertebral Disc
This may occur during an acute flexion injury and cause extensive injury to the anterior part of the spinal cord. There is impaired motor function with reduced pain and temperature sensation. The posterior horns and posterior columns are usually undamaged so that touch and proprioception remain intact. Also → p. 58.
Posterior Cord Syndrome
Hyperextension injuries with fractures of the posterior elements of the vertebrae may injure the posterior columns. Loss of proprioception may cause profound ataxia in the presence of normal power and pain and temperature sensation.
Brown–Séquard Syndrome
This lateral cord syndrome can be precisely produced only by a knife or gun, although closed injuries (lateral mass fractures) may also give rise to some of its classic features. These are the signs of a hemisection of the cord. On the injured side there is reduced power, but relatively normal pain and temperature sensation because the spinothalamic tract crosses over to the opposite side. The uninjured side has normal power, but reduced sensation for pain and temperature.
IMAGING AND CLEARANCE OF THE SPINE IN TRAUMA
Radiographs taken to confirm a clinically proven injury to the spine are less important initially than those requested for patients who are asymptomatic but at risk. Splints should be radiolucent and retained during radiography.
 Box 4.1 Indications for CT and MRI in Spinal Trauma
Box 4.1 Indications for CT and MRI in Spinal Trauma- Areas of the spine poorly visualised on plain films
- Fracture not excluded by plain films
- Significant or possibly significant fracture on plain films (requiring further visualisation)
- Unexplained neurology after trauma
- Fracture on plain films or CT scan with unknown associated soft-tissue injuries
- Suspected ligament or disc injury
- Neurological symptoms and signs referable to the spine
- Suspicion of vascular injury to the spinal cord
Radiographs of the Cervical Spine
These should be obtained for all patients with:
- multiple injuries
- injuries caused by the mobile head striking a fixed object.
There are three standard views of the cervical spine in UK practice:
Supplemental oblique views are used to visualise the apophyseal joints, looking for facet joint dislocation. Radiographs in flexion and extension are used to reveal instability. They should be taken only in the presence of a senior clinician.
Lateral View
Adequacy:
This is the view that causes the most trouble. The first film is adequate (C7–T1 disc space shown) in only about two-thirds of cases. Often, only the first five vertebrae are demonstrated.
 Box 4.2 Suggested Sequence to be Followed If the Lateral Radiograph of the Cervical Spine is Inadequate
Box 4.2 Suggested Sequence to be Followed If the Lateral Radiograph of the Cervical Spine is InadequateAlignment:
Confirm the continuity of the curve along the following four lines:
Look for steps. Normal slight lordosis is lost when there is painful muscle spasm.
C2 may appear to be subluxed forward on C3 in young children; the same appearance is less frequently seen of C3 on C4. These are normal variants that occur in up to 10% of children aged <7 years and disappear on extension of the neck.
Bones:
Compare the height and shape of each vertebral body, looking for wedging and fractures.
Examine each apophyseal joint and spinous process for malalignment and fractures.
Look at the integrity of the odontoid peg and for increased space between the peg and the anterior arch of C1. Look for fracture of the posterior arch of C1 and for ‘hangman’s fracture’ of the pedicles of C2.
Cartilages:
Examine each intervertebral joint looking for osteophytes and narrow disc spaces.
Soft Tissue:
The soft-tissue shadow, anterior to the vertebral bodies, is increased if there is a fracture, haematoma or anterior ligament injury. Air is trapped in this area if there is damage to the posterior pharyngeal wall. Above the larynx, the width of the prevertebral soft-tissue space should be less than a third of the diameter of the vertebral body. Below this level, the space is accepted as normal if it is no wider than a whole vertebral body.
Look for widening of the space between the spinous processes (torn interspinous ligaments).
Upper AP (Odontoid peg) View
Adequacy:
The upper AP view is adequate in only about two-thirds of first films. The odontoid peg may be superimposed on the base of the skull or on the upper incisors. Simple repositioning is usually sufficient.
Alignment:
Look at the lateral masses of C1, on either side of the odontoid peg. They should line up with the equivalent parts of C2. Spread suggests a burst (Jefferson’s) fracture.
Bones:
Look at the integrity of the odontoid peg.
Anteroposterior View
Adequacy:
The first attempt at this view is invariably adequate.
Alignment:
Look for symmetry of the apophyseal joints.
Bones:
Examine the transverse processes for fracture, or buttressing of C7 or a cervical rib. Thyroid cartilage wings are often misinterpreted as calcified vertebral arteries.
Cartilages:
Confirm that the disc spaces are equal. Spaces above and below the centre of the X-ray beam appear narrower but should be bilaterally symmetrical.
Soft Tissue:
Confirm the central shadow of tracheal air.