CHAPTER 95 THE IMMUNOLOGY OF TRAUMA
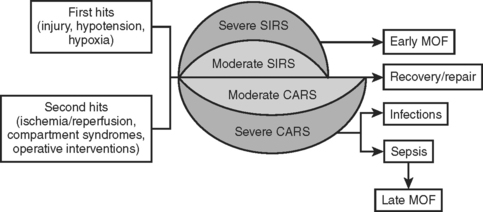
Following trauma, the immune system is called into action by signals from injured tissues. Injuries, hypoxia, and hypotension, as well as secondary insults such as ischemia/reperfusion injuries, compartment syndromes, operative interventions, and infections induce a host response that is characterized by local and systemic release of proinflammatory cytokines, arachidonic acid metabolites, and activation of complement factors, kinins, and coagulation as well as hormonal mediators. Clinically, this is the systemic inflammatory response syndrome (SIRS). Paralleling SIRS is an anti-inflammatory response referred to as the compensatory anti-inflammatory response syndrome (CARS). An imbalance between these responses appears to be responsible for increased susceptibility to infection and organ dysfunction. The aim of this chapter is to provide an overview of the immune response following trauma.
TWO-HIT MODEL
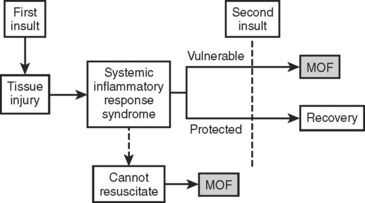
In the two-hit model, the inciting injury induces a systemic inflammatory response (Figure 1). This “first hit” primes the immune system for an exaggerated and potentially lethal inflammatory reaction to a secondary, otherwise nonlethal, stimulus (“second hit”). This secondary stimulus may be either endogenous or exogenous. Endogenous second hits include cardiovascular instability, respiratory distress, metabolic derangements, and ischemia/reperfusion injuries. In contrast, exogenous second hits include surgical interventions, blood product transfusions, and missed injuries. The two-hit model proposes that this second hit results in destructive inflammation leading to multiple organ failure (MOF) and potentially death. This model has been supported by the work of Moore and colleagues who linked postinjury opportunistic infections to SIRS and MOF.
SYSTEMIC INFLAMMATORY RESPONSE SYNDROME
In 1991, a consensus conference of the American College of Chest Physicians and the American Society of Critical Care Medicine (ACCP/SCCM) defined SIRS as a generalized inflammatory response triggered by a variety of infectious and noninfectious events. They arbitrarily established clinical parameters through a process of consensus. Table 1 summarizes the diagnostic criteria for SIRS. At least two of the four criteria must be present to fulfill the diagnosis of SIRS. Note that this definition emphasizes the inflammatory process regardless of the presence of infection. The term sepsis is reserved for SIRS when infection is suspected or proven. Subsequent studies have validated these criteria as predictive of increased intensive care unit (ICU) mortality, and that this risk increases concurrent with the number of criteria present.
Table 1 Clinical Parameters of Systemic Inflammatory Response Syndrome
PaCO2, Arterial CO2 partial pressure.
COMPENSATORY ANTI-INFLAMMATORY RESPONSE SYNDROME
Trauma not only stimulates the release of proinflammatory mediators, but also the parallel release of anti-inflammatory mediators. This compensatory anti-inflammatory response is present concurrently with SIRS (Figure 2). When these two opposing responses are appropriately balanced, the traumatized individual is able to effectively heal the injury without incurring secondary injury from the autoimmune inflammatory response. However, overwhelming CARS appears responsible for post-traumatic immunosuppression, which leads to increased susceptibility to infections and sepsis. With time, SIRS ceases to exist and CARS is the predominant force.
CYTOKINE RESPONSE
Following trauma, IL-12 production is decreased, stimulating a shift in favor of TH2 cells and the subsequent production of antiinflammatory mediators IL-4, IL-10, IL-13, and transforming growth factor beta (TGF-β). This decrease in IL-12 and resultant increase in TH2 cells correlates with adverse outcomes. A listing of pro and anti-inflammatory mediators appears in Tables 2 and 3.
Table 2 Proinflammatory Mediators
| Mediator | Action |
|---|---|
| IL-1 | IL-1 is pleiotropic. Locally, it stimulates cytokine and cytokine receptor production by T cells as well as stimulating B-cell proliferation. Systemically, IL-1 modulates endocrine responses and induces the acute phase response. |
| IL-6 | Il-6 induces acute-phase reactants in hepatocytes and plays an essential role in the final differentiation of B cells into Ig-secreting cells. Additionally, IL-6 has antiinflammatory properties. |
| IL-8 | IL-8 is a major mediator of the inflammatory response. It functions as a chemoattractant and is also a potent angiogenic factor. |
| IL-12 | IL-12 regulates the differentiation of naive T cells into TH1 cells. It stimulates the growth and function of T cells and alters the normal cycle of apoptotic cell death. |
| TNF-α | TNF-α is pleiotropic. TNF-α and IL-1 act alone or together to induce systemic inflammation as above. TNF-α is also chemotactic for neutrophils and monocytes, as well as increasing neutrophil activity. |
| MIF | MIF forms a crucial link between the immune and neuroendocrine systems. It acts systemically to enhance the secretion of IL-1 and TNF-α |
Ig, Immunoglobulin; IL, interleukin; MIF, migration inhibitory factor; TNF, tumor necrosis factor.
Table 3 Anti-Inflammatory Mediators
| Mediator | Action |
|---|---|
| IL-4 | IL-4, IL-3, IL-5, IL-13, and CSF2 form a cytokine gene cluster on chromosome 5q, with this gene particularly close to IL-13. |
| IL-10 | IL-10 has pleiotropic effects in immunoregulation and inflammation. It downregulates the expression of TH1 cytokines, MHC class II antigens, and costimulatory molecules on macrophages. It also enhances B-cell survival, proliferation, and antibody production. In addition, it can block NF-kappa B activity, and is involved in the regulation of the JAK-STAT signaling pathway. |
| IL-11 | IL-11 stimulates the T-cell–dependent development of immunoglobulin-producing B cells. It is also found to support the proliferation of hematopoietic stem cells and megakaryocyte progenitor cells. |
| IL-13 | IL-13 is involved in several stages of B-cell maturation and differentiation. It upregulates CD23 and MHC class II expression, and promotes IgE isotype switching of B cells. It downregulates macrophage activity, thereby inhibiting the production of proinflammatory cytokines and chemokines. |
| IFN-α | IFN-α enhances and modifies the immune response. |
| TGF-β | TGF-β regulates the proliferation and differentiation of cells, wound healing, and angiogenesis. |
| α-MSH | α-MSH modulates inflammation by way of three mechanisms: direct action on peripheral inflammatory cells, actions on brain inflammatory cells to modulate local reactions, and indirect activation of descending neural anti-inflammatory pathways that control peripheral tissue inflammation. |
CSF, Colony-stimulating factor; IFN, interferon; Ig, immunoglobulin; IL, interleukin; MHC, major histo-compatibility complex; MSH, melanocyte stimulating hormone; TGF, transforming growth factor; TH, T helper.