Fig. 30.1
Sir Ivan “Paddy” Magill (1888–1986) holding an equine version of his tracheal tube
Magill contributed to academic anaesthesia and the recognition of anaesthesia as a specialty through the founding of the Association of Anaesthetists of Great Britain and Ireland (AAGBI) in 1932, and through the inauguration of the Diploma in Anaesthesia (DA) in 1935, under the auspices of the Anaesthetic Section of the Royal Society of Medicine [12]. Other hospitals appointed specialist anaesthetists, but, even so, only 50 existed in the whole of the UK. Numerous hospitals employed general practitioners, many with limited training, as anaesthetists for general surgical procedures and for the administration of ethyl chloride or nitrous oxide for dental extractions.
Between 1901 and 1925, many universities established honorary or part-time anaesthetic appointments, mostly within surgical departments, to enable the teaching of undergraduates.
The Chair of Anaesthetics at the University of Oxford [22]
Oxford had no clinical medical school in the early 1930s. The then Minister of Health, Neville Chamberlain, (yes the same Neville Chamberlain who in September 1938 and as Prime Minister returned from Munich stating “I believe it is peace for our time”) consulted with the Regius Professor of Medicine, Farquhar Buzzard, about the desirability of setting up a postgraduate medical school. Douglas Veale, who had been Chamberlain’s private secretary, moved to Oxford to become the University Registrar. Hugh Cairns, an Australian neurosurgeon who had trained with Harvey Cushing in Boston, was interested in this concept and wrote two extensive memoranda proposing a research-orientated medical school at Oxford. Buzzard, Veale and Cairns targeted Lord Nuffield for support. Nuffield, as William Morris, had developed a major automobile industry in Oxford and became one of Britain’s great philanthropists. (Fig. 30.2) Nuffield initially offered the University £ 1.25 million to establish “a school where professors and their assistants may pursue their research in clinical medicine unhampered by the claims of private practice or the routine teaching of students [22]. In a presidential address to the 104th Annual Meeting of the British Medical Association at Oxford in 1936, Buzzard stated that “The task of the heads of medical research departments, who must all be recognized leaders in their field, would be to link observations at the bedside with those made in laboratories” (translational research is not new!) [23]
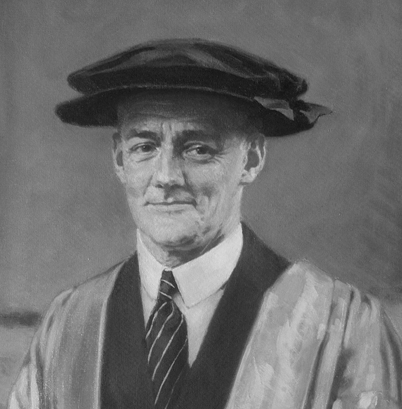
Fig. 30.2
Lord Nuffield (William Morris) (1877–1963), philanthropist and benefactor of anaesthesia, in academic regalia
Buzzard and Veale proposed that the grant be used to fund professors and departments of medicine, surgery, and obstetrics (and gynaecology). However, as a young man Nuffield had experienced problems following general anaesthesia for dental extractions, and was adamant that he wanted a Chair of Anaesthetics as part of his endowment. In August 1936, Cairns wrote to Howard Florey (Professor of Pathology, representing pre-clinical disciplines) that a Department of Anaesthetics would be: “quite feasible’to serve primarily as a training ground which could turn out all the young anaesthetists of the country at large, and probably many from the Dominions”. Meeting with Nuffield’s secretary, Veale “…wondered whether Nuffield really meant a Professorship, not a Readership, suggesting that anaesthetics might not be a subject of professorial status” [22]. Veale also proposed allocating a lower salary for this position, £ 1500 compared with £ 2000 for the other professors. Nuffield increased his gift to £ 2 million provided that a Chair of Anaesthetics was included, and that Robert (later Sir Robert) Macintosh, a New Zealander, would be appointed to the chair (Fig. 30.3). The University reluctantly agreed to Nuffield’s proposal, in doing so establishing anaesthesia as an academic subject, and creating the first Chair of Anaesthetics in Britain, the British Commonwealth, and Europe [22].
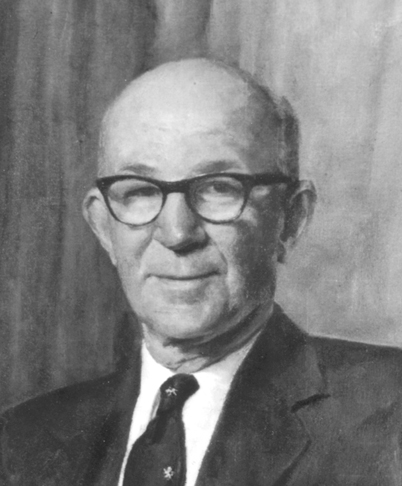
Fig. 30.3
Sir Robert Macintosh (1897–1989), the first Nuffield Department of Anaesthetics chair
The Oxford hospitals created three major problems for the four new Nuffield professors, especially Macintosh. Who controlled a hospital service; who controlled fees from paying patients, and who controlled secondary costs to the hospital? After many discussions Macintosh won dominion in that “… the Honorary Anaesthetists had no objection to Professor Macintosh being in general charge over the Department …” (p35) [22]. The Oxford hospitals insisted that the newly appointed Nuffield professors, and their medical assistants, would not undertake private practice, and the University introduced a £ 500 per annum bonus to a Nuffield Professor who did not accept fees from private patients. The third issue concerned the building of new departmental accommodations for the Nuffield professors. The Departments of Surgery (Hugh Cairns) and Obstetrics (Chassar Moir) controlled new wards and operating facilities, but Macintosh endured a prolonged battle for suitable accommodation. From the outset, and throughout the war years, Macintosh’s department, now named theNuffield Department of Anaesthetics (NDA) was housed in a temporary structure on the roof of another hospital building. The final purpose-built department came into being after Macintosh’s retirement in 1965!
During the war years (1939–1945), the NDA had a heavy teaching commitment, training postgraduate specialists to achieve the new Diploma in Anaesthesia, and thereby supply the burgeoning demand for anaesthetists in the armed forces. Macintosh was an Air Commodore in the Royal Air Force and travelled widely to ensure that equipment for that service was up to standard. During the war years, the NDA developed a submarine escape apparatus using CO2 absorption, and studied the physiological effects of flying at high altitude (up to 40,000 feet). A novel, but unsuccessful, study designed a system that would allow Winston Churchill to breathe oxygen at altitudes greater than 8000 feet while smoking the cigars to which he was habituated [22]. Edgar Pask (1912–1966) allowed himself to be anaesthetized and subject to ventilatory arrest by forced hyperventilation with 15% ether in order to test the efficacy of various methods of resuscitation. To test the efficacy of 17 types of life-jackets, Pask allowed himself to be anaesthetized, have his trachea intubated, and then to be submerged under water on four separate occasions [22].
Macintosh’s main contribution to research in anaesthesia was to develop, in co-operation with Hans Epstein, and Morris Motors (Nuffield’s factory), an accurate portable draw-over vaporizer for ether (the Oxford vaporizer). The vaporizer allowed delivery of controllable ether vapour concentrations and thus safer anaesthesia, to be administered under field (armed forces) conditions, with or without added oxygen [24]. The principles of the Oxford vaporiser were later applied to the design, in 1956, of the EMO (Epstein, Macintosh, Oxford) vaporiser, and a subsequent miniature vaporizer, both robust and reliable devices. They formed the basis of future vaporizer designs. Macintosh also designed a laryngoscope blade that quickly gained worldwide acceptance.
Was Anaesthesia Safe?
In 1943, George Godber, Chief Medical Officer of Health (CMO), surveyed hospital services, finding that “virtually all the anaesthetists were also in general practice [25]. Unstated was the conclusion that the resulting occasional anaesthetist must compromise safety.
Immediately After World War II
Soon after World War II, four more universities created Departments of Anaesthesia. In 1946, the University of Bristol created a department headed by Ronald Woolmer (as a Senior Lecturer, later upgraded to Reader). In 1957, Woolmer was appointed Professor in the Research Department of Anaesthesia at the Royal College of Surgeons in London. Edgar Pask, became a Reader in the University of Newcastle-upon-Tyne in 1947, and full Professor in 1949. William Mushin (1910–1993), previously First Assistant in the NDA, was appointed Director of Anaesthesia to the Cardiff group of hospitals. In 1952 he was elected to a Chair of Anaesthesia in the Welsh National School of Medicine. T Cecil Gray (1913–2008) gained an MD in 1947, and was appointed Head of Department (Reader) in the University of Liverpool (Fig. 30.4). He was subsequently granted a Personal Chair in 1959. Gray and his Liverpool colleagues (Halton, G Jackson Rees, Utting, and Robinson) popularized the use of curare (d-tubocurarine) in British anaesthesia, and created the ‘Liverpool technique’ based on nitrous oxide anaesthesia, muscle relaxation induced by curare, and manually controlled ventilation [26]. Shafer, who argues that Gray’s real innovation was that of balanced anaesthesia with a combination of drugs rather than a single inhalational agent, recently reviewed Gray’s enormous contribution to modern anaesthetic practice [27].
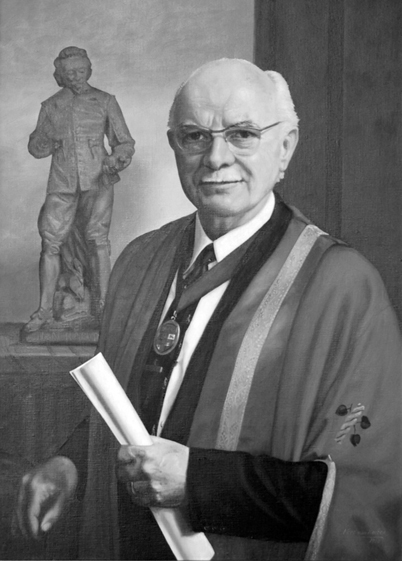
Fig. 30.4
T. Cecil Gray (1913–2008) in his robes as Dean of the Royal College of Anaesthetists
Open cardiac surgery, mostly in adults, was made possible in 1952–1953 by pump-oxygenators (either the Melrose design developed at the Hammersmith Hospital, or the American Mayo-Gibbon machine), or profound hypothermia as pioneered at the Westminster Hospital. Induced hypotension techniques were developed to facilitate neurosurgery and plastic surgery. In the late 1940s, John Gillies (1895–1976) in Edinburgh, pioneered total spinal anaesthesia for the surgical treatment of hypertension by thoraco-lumbar sympathectomy, achieving drastic decreases in blood pressure (to less than 50 mm Hg) [28]. Subsequently, ganglion-blocking and adrenoceptor-blocking drugs combined with head-up tilt made the process potentially much safer [29].
1948–1988
The Faculty of Anaesthetists of the Royal College of Surgeons of England
After World War II, academic aspects of anaesthesia progressed on several fronts. The Goodenough Committee proposed that medical schools should create clinical academic departments, and that universities should support whole-time staff [30]. Representations by the Association of Anaesthetists to the Spens Committee led to the recognition that anaesthetists should be accorded equal status (and thus pay) with other hospital-based specialists [31]. The inauguration of the National Health Service (NHS) in 1948, led to the recognition that the number of suitably qualified consultant (specialist) anaesthetists was too small to staff the major hospitals of the country. The specialty moved rapidly to upgrade the Diploma of Anaesthesia (DA), then organised jointly by the Royal Colleges of Physicians and Surgeons, to a two-part examination: Primary (basic sciences) and Final (clinical anaesthesia). The Association of Anaesthetists requested the Royal College of Surgeons to establish a Faculty of Anaesthetists. The Board of the resulting new Faculty met on 23 March 1948 under its first Dean, Archibald Marston. It was considered that a proposed Fellowship (1952) of the new Faculty (FFARCS) “would greatly enhance the academic status of the Faculty as well as being a means to encourage anaesthetists to attain the highest distinction in their speciality”. The GMC now considered anaesthesia to be a postgraduate subject, and consequently omitted the teaching of anaesthetics from the undergraduate curriculum in 1947, a regressive step that was corrected in the 1980s.
The training of specialist anaesthetists, which increasingly included intensive care, followed the pattern taken by other medical and surgical specialties. After internship, trainees occupied training posts in NHS hospitals, at senior house officer and then registrar status. The NHS assumed responsibility for trainee employment, while the Faculty (of Anaesthetists) controlled the setting and supervision of standards of training, and of examinations. After passing the final examination, trainees progressed to Senior Registrar posts for 3 to 5 years advanced training, after which they could apply for NHS consultant posts. Senior Registrars were encouraged to spend time abroad, expanding their research and clinical training, mostly in North America, Europe, Australia or New Zealand.
In the UK and the Republic of Ireland, unlike other countries in Europe, universities were not responsible for medical specialist training. The relevance of this statement will become evident later in this essay.
During its first forty years, the Faculty of Anaesthetists was accommodated in the Royal College of Surgeons, and the organization of its parent, the Royal College of Surgeons, largely determined the organization of the Faculty. Although the Faculty became financially independent, it enjoyed close support and good relations with its parent College. The Faculty had three major responsibilities: postgraduate (specialist) education, examination for the primary and final fellowship, and the setting of professional standards in anaesthesia, intensive care and, increasingly, treatment of severe and chronic pain.
The Faculty of Anaesthetists of the Royal College of Surgeons in Ireland, established in 1959, developed along almost identical lines, and until 1995 there was a reciprocal recognition of training standards and examinations between the two Faculties.
So, as the sixties began, academic anaesthesia was advancing well. Between 1960 and 1971, 15 new university departments headed by chairs of anaesthesia emerged. Britain differed from Germany and many other European countries, where a higher degree (doctorate, Habilitation) was an absolute requirement for advancement to an academic chair. John Nunn at Leeds (Fig. 30.5), and Alex Crampton Smith (Fig. 30.6) (as Macintosh’s successor) at Oxford were the great facilitators of scientific research, and sought to raise the calibre of the specialty by promoting research doctorates (PhD and MD). NHS hospitals increasingly supported Intensive Care, and a few university anaesthesia departments (Leeds, Oxford, Glasgow, Royal Postgraduate Medical School’Hammersmith) concentrated research efforts on this new sub-specialty.
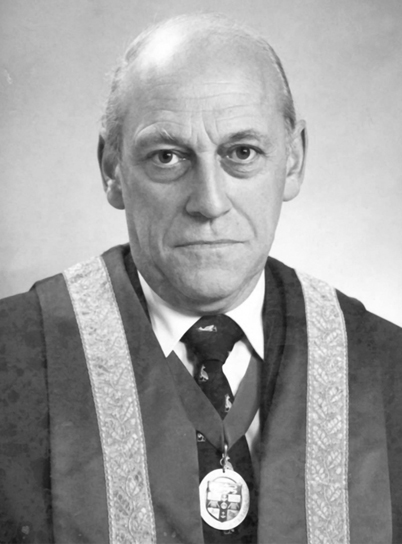
Fig. 30.5
John Nunn in his robes as Dean of the Royal College of Anaesthetists
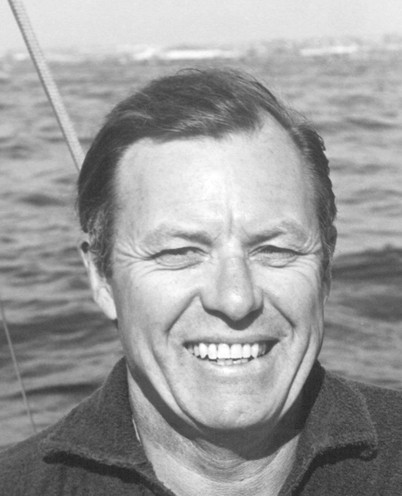
Fig. 30.6
Alex Crampton Smith (1917–2010) on the high seas
Anaesthetic Research Society and Publication of Research
The Anaesthetic Research Group began in 1958 as a discussion forum for research in progress, rather than completed work [32]. Initially some established professors (Macintosh, Gray, Mushin, and Pask) were not supportive, but by 1967, the group meetings attracted substantial pre-publication presentations of research from both university and NHS departments. The group was reformed as the Anaesthetic Research Society in 1968. Two anaesthesia journals, theBritish Journal of Anaesthesia (founded in 1923), andAnaesthesia (founded in 1946), contributed enormously to the development of clinical and research aspects of anaesthesia and intensive care during this period, by supplying a distinguished print forum for the work of investigators in anaesthesia. TheLancet and BMJ only accepted articles of general interest to medical practitioners, and specialist journals such as theJournal of Physiology, Journal of Applied Physiology, andCardiovascular Research were relevant to only a handful of researchers.
Drug Development
The success of the pharmaceutical industry in developing new drugs, greatly influenced four categories of progress in clinical anaesthesia: inhalational agents, opioid analgesics, intravenous anaesthetics, and muscle relaxants. Working at Imperial Chemical Industries (ICI), near Manchester, in the early 1950s, Suckling [33] and Raventós [34] developed halothane. Introduced into clinical practice in the late 1950s [35,36], and delivered with a calibrated vaporizer, the Fluotec, halothane rapidly replaced the flammable anaesthetics, diethyl ether and cyclopropane. Although halothane caused hypotension, and indeed was used specifically for induced hypotension [29], this was widely considered to be safe because it had been described as a vasodilator [36]. However, studies in animals [37] and humans [38] showed that halothane produced a concentration-dependent depression of the myocardium.
In 1961, Tunstall [39] described the first use of a pre-mixed gas, nitrous oxide (50%) and oxygen (50%), for analgesia during childbirth. This development was to be of considerable benefit in obstetrics, and also in accident and emergency medicine.
Paul Janssen, in Belgium, developed a new series of synthetic opioids modelled on pethidine (meperidine). They were initially introduced in the UK in 1964, to add to the technique of neuroleptanalgesia [40], a technique combining an opioid (phenoperidine) with a neuroleptic drug (haloperidol) to produce a ‘vegetative’ state that could be augmented with nitrous oxide anaesthesia. Subsequently, fentanyl (1965), alfentanil (1976), sufentanil (1976) and remifentanil (1993) became widely used as the analgesic components to supplement ‘balanced’ inhalation anaesthesia and, from the mid-sixties onwards, of total intravenous anaesthesia.
Although thiopentone had been the standard induction agent, methohexitone and Althesin became popular in the UK and Ireland. Althesin, a combination of the steroids alphaxolone (the main effective anaesthetic) and alphadolone, solubilized in Cremophor EL, was developed by Glaxo Ltd (Uxbridge, Middlesex) in 1972. It was widely used as an induction agent and later as a continuous infusion [41,42]. The rapid recovery from single or multiple doses of Althesin was a great advantage over thiopentone. The latter rapidly declined in popularity in the UK, whereas in the US it remained the main agent for induction of anaesthesia. Althesin was withdrawn from human use following reports of complement-mediated anaphylactoid reactions to Cremophor EL [43]. Glaxo Ltd subsequently developed a water soluble steroid anaesthetic, Minaxolone [44], but teratogenicity issues in animals caused it to be withdrawn. Finally, in 1980, Glen and colleagues at Pharmaceuticals, near Manchester, developed a new intravenous anaesthetic: di-isopropyl phenol [45]. This lipid-soluble anaesthetic was also initially solubilized in Cremophor EL, but concerns that anaphylactic reactions might occur [46] led to its reformulation in a lipid emulsion [47]. Released in 1986, propofol, became the most popular agent world-wide for intravenous induction of anaesthesia, for the sedative component of total intravenous anaesthesia, and for continuous sedation in intensive care.
In 1967, Baird and Reid reported on the clinical use of pancuronium, a new muscle relaxant developed by Organon Laboratories, of Cambridge [48]. Pancuronium became widely used as a medium duration neuromuscular blocking agent (NMB), that had mild vagolytic effects on the cardiovascular system. In 1981, atracurium was released by the Wellcome Research Laboratories, of Beckenham, Kent, as a novel NMB that underwent spontaneous degradation by the Hofmann reaction [49,50]. Cis-atracurium, a stereoisomer of atracurium, has largely superseded the parent drug.
The Eighties
Archie Brain designed, and in 1983 introduced, a remarkable advance in airway management, the laryngeal mask airway (LMA) [51]. This simple device evolved into the most widely used new airway since the introduction of the oral airway and tracheal tube. Although the main use of the mask has been in anaesthesia, it has also been applied in emergency medicine, in situations where manipulation of the head or neck is difficult because of potential cervical spine injury, or during rescue in confined spaces. Modifications include channels for gastric suction (LMA ProSealTM, LMA SupremeTM), and for guiding endotracheal tubes into the larynx (ILMA’Intubating Laryngeal Mask Airway) and LMA-FastrachTM [52].
A pilot study by Lunn and Mushin of mortality associated with anaesthesia [53] led to the initiation of a joint venture between anaesthetists and surgeons and the publication in 1987 of the first report of the Confidential Enquiry into Perioperative Deaths (CEPOD) [54]. This initial report quoted a mortality, within 30 days of surgery, of 0.7% in a cohort of half a million patients, with more than half the deaths in patients over 75 years old. The authors recommended that all anaesthetists and surgeons should audit their personal and departmental clinical practices, to enhance quality assurance for patient care; and that they should review consultants’ supervision of trainees. NCEPOD (N for National) continued on an annual review basis, evaluating perioperative deaths in a range of patient age groups or surgical interventions. During the first 11 years, the number of deaths reported was fairly consistent (range: 18,132 to 20,442 deaths per annum), but the number of deaths attributed to anaesthesia decreased progressively and is now considered to be between 1 and 2 deaths per million anaesthetics. In 2004 the same acronym, NCEPOD, changed to mean National Confidential Enquiry into Patient Outcome and Death, thus expanding the objectives. A similar system had been established in 1952, as the Confidential Enquiry into Maternal Deaths (CEMD) and the Confidential Enquiries into Stillbirths and deaths in Infancy (CESDI) [55].
The most recent (2011) NCEPOD report [56] compared data on mortality for patients undergoing major non-cardiac surgery in the UK and US in comparable hospitals over the same time period. Applying the P-POSSUM (Portsmouth modifiedPhysiological andOperativeSeverityScore for the enUmeration ofMortality and morbidity) index, the authors concluded that patients in the UK with a predicted 0–5% mortality risk had an actual mortality (2.5%) that was eight times higher than their counterparts in the US (0.3%). A critique of this report [57] pointed out that the US spends significantly more (15.3%) of its GDP on health care than does the UK (8.2%), and has nearly 6 times the number of intensive care beds than does the UK. Their conclusion that “…the NHS needs to invest in more critical care beds to improve outcomes in high risk surgical patients.” was tempered in an accompanying editorial [58] which identified several strategies that could, with economy, improve outcomes.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







