Fig. 4.1
John Snow
Snow Tells How to Give Anesthesia
In 1847, the medical community needed to know how to deliver anesthesia smoothly and safely and how to control the depth of anesthesia with as much precision as the available anesthetics and extant equipment permitted. Expressions such as a greater depth or level of anesthesia indicated achievement of a greater anesthetic effect. Enter Snow’s classic book on the delivery of ether [12]. A decade later, he supplied his second classic book’on the delivery of chloroform [13]. To digress a moment: Snow’s genius extended beyond anesthesia. He was the father of epidemiology, famously diagnosing the cause of an 1854 cholera epidemic in London that killed 500 people in 10 days (in the preface of the referenced book) [13]. To deal with the epidemic, Snow told the vestrymen of St. James district to remove the handle from the Broad Street pump (p xxi). His studies revealed that the dead had drawn from the Broad Street well. The vestrymen of St. James’s (the district containing the well) were “incredulous, but had the good sense to carry out the advice. The pump-handle was removed, and the plague was stayed.”
Snow, born in York, on 15 June 1813, was the eldest son of a farmer. In 1827 he was apprenticed to a surgeon. Other apprenticeships followed. For a few years Snow became a vegetarian (he determined later that it was not healthful) and temperance advocate. He came to London to study at the Hunterian School of Medicine, becoming a physician in 1838. His friend Richardson described Snow as “Not particularly quick of apprehension, or ready in invention, he yet always kept in the foreground by his indomitable perseverance and determination in following up whatever line of investigation was open to him (p v).”[13]
John Snow’s observations on anesthesia were as brilliant (although not as flamboyant) as his prescription for stopping the cholera epidemic. Regarding ether [12], Snow described 5 degrees (i.e., stages) of anesthesia, anticipating by more than half a century, Guedel’s classic four Stages (and many Signs) of anesthesia [14]. Snow observed (p 1): “In the first degree of etherization I shall include the various changes of feeling that a person may experience, whilst he still retains a correct consciousness…and a capacity to direct his voluntary movements.” Aha! So in the first degree, the patient is awake, aware, and remembers.
Snow continued (p 2): “In…the second degree, mental functions may be exercised, and voluntary actions performed, but in a disordered manner.” The patient is still awake and aware’but there may be no memory of that awareness.
Snow (p 10) noted that anesthesia produces amnesia and described much of MACawake (the anesthetic concentration preventing awareness in half of subjects who, however, respond appropriately to commands such as “open your eyes”) [15] a century before the concept was developed: “…and if…the patient is allowed to recover still further during the operation, it will probably happen that in the second degree he will either lie perfectly calm, or talk in his dreams about subjects totally unconnected with pain, or the operation which is still going on.”
Snow repeatedly returned to the notion of dreams occurring in the second degree of anesthesia but “there can be no dreams or ideas of any kind in the third and fourth degrees….” (p 11). This accords with the modern determination that dreams occur during recovery from anesthesia and not during anesthesia [16]. “In the third degree, there is no evidence of any mental function being exercised, and consequently no voluntary motions occur; but muscular contractions, in addition to those concerned in respiration, may sometimes take place” (pp 1–2) [12]. Thus, in the third degree, the patient may respond to surgery with movement.
Snow, like Morton, noted another component of the third or even the second degree, one that anticipated Joseph Artusio’s 1950s publications [17,18] on ether analgesia (p 10). Unlike Morton, the far more perceptive Snow knew what he had. “I believe that pain is seldom felt in the stage of which we are treating–the third degree succeeding the fourth (i.e., during recovery from the fourth degree)’and of course never remembered afterwards, as there is no knowledge or mental perception of it.”
The analgesia noted above for the second or third degree, seemed to be most obvious during recovery from anesthesia and not during induction of anesthesia. Snow speculated that this might be the result of ether acting on peripheral nerves rather than on the central nervous system, an intriguing idea that might fit with the known lesser blood flow to nerves and the greater affinity of anesthetics for nerves as compared to brain. The smaller flow and the greater affinity would delay the establishment of a sufficient ether concentration in the nerves, and hence delay the appearance of analgesia. Snow’s idea remains to be tested.
“In the fourth degree, no movements are seen except those of respiration, and they are incapable of being influenced by external impressions.”
Snow’s description of movement with incision in the third degree, and its absence in the fourth degree, anticipated by a century, the discovery of MAC (the minimum alveolar concentration preventing movement in response to incision in 50% of patients) [19]. Indeed, Snow wrote: “Ether contributes other benefits besides preventing pain. It keeps patients still, who otherwise would not be” (p 53) [12]. And (p 6): “If this degree of etherization is not well established when the operation begins, the first cut may cause a sudden contraction of the whole muscular system.” And thus Snow appreciated the need for equilibration of the site of action with the ether delivered to that site. And (p 7): “In (the fourth) degree of etherization the patient always remains perfectly passive under every kind of operation; and…the muscles are completely relaxed….” He even described the use of a supramaximal stimulus as important to a test of the efficacy of anesthesia (p 36) [12]: “…there may be insensitivity to a slight lesion’as a suture in the skin, for instance’at a time when a greater wound would cause signs of pain.” Thus Snow observed that one level of anesthesia may permit a muscular response to a supramaximal stimulus, but one degree deeper prevented that response once equilibrium had been obtained. Snow only needed the ability to measure the concentration of ether in the lungs (the alveoli) to have described MAC, the modern standard by which the unit depth of anesthesia is defined [20].
“In the fifth degree…respiratory movements are more or less paralysed and become difficult, feeble, or irregular.” Snow advised against entering the fifth degree, concerned that undue depression of breathing and the heart might follow.
Snow described eye signs, changes that allow the assessment of anesthetic depth (p 5) [12]: “The patient may have moved his eyes about in the second degree, and even directed them to objects, but in this degree (deeper anesthesia) they are stationary, or if they do move, their motions have nothing of a voluntary character…The eyelids may be either open, or partly or tightly closed, but in either case, if lifted or moved by the finger, the orbicularis palpebrarum (the eyelid) contracts.” These degrees (or Guedel’s variation on them) were used to define depth of anesthesia for the next century.
Snow was amazingly perceptive. He anticipated that ether might be metabolized (p 84) [12]: “It is not improbable that some of the ether inhaled is decomposed in the body; but this does not alter the question of de-etherization…for assuredly by far the greater portion of the ether escape by the breath exhaled.” Actually, he may have erred there because by far the lesser portion of some inhaled anesthetics escape by exhalation [21,22]. We don’t know about ether.
He recognized that age and breathing affected ether kinetics (the movement of ether into and out of the body; p 43) [12]: “Elderly people are slower in recovering than young ones as their respiration is less active, and the ether takes a longer time to evaporate in the breath. For the same reason, if sickness has been caused by the ether, the patient is longer in recovering, as it depresses the respiratory movements.”
Snow recognized the importance of control over the concentration of ether and the connection between concentration and the degree of anesthetization (p 15) [12]: “I have spoken of a knowledge of the strength of the vapour as being essential to a correct determination of the state of the patient at all times: and this brings us to the apparatus for the administration of the vapour, as, without a suitable one, the proportions of air and of vapour cannot be determined.” He recognized the importance of controlling the temperature of the vaporizer (with a water jacket) to avoid changes in the concentration of anesthetic (Figs. 4.2 and4.3). He recognized the need to supply sufficient surface area to assure the saturation of the gas passing through the vaporizer with anesthetic. His vaporizer allowed for the introduction of air to dilute the ether stream (anticipating the modern “variable bypass vaporizer” by more than a century.)
Fig. 4.2
Snow found that as temperature of an anesthetic increased, so did the concentration in the air overlying the anesthetic. (From Snow J: On the Inhalation of the Vapour of Ether in Surgical Operations: Containing a Description of the Various Stages of Etherization, and a Statement of the Result of Nearly Eighty Operations in Which Ether Has Been Employed In St. George’s and University College Hospitals. London: John Churchill; 1847. pp 1–88.)
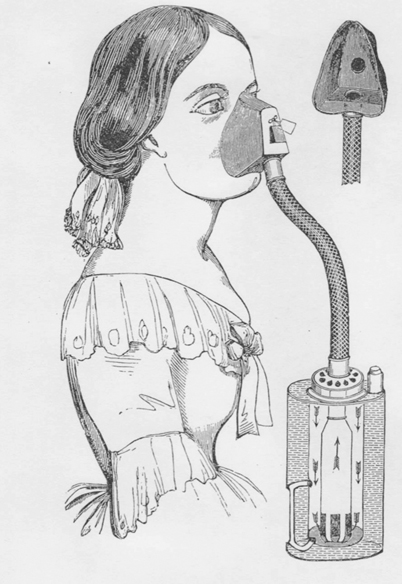
Fig. 4.3
A genteel lady breathes ether or chloroform from a vaporizer constructed to ensure the fullest concentration of anesthetic. A jacket filled with water buffers the vaporizer against temperature changes and thus against changes in the anesthetic concentration issuing from the vaporizer. A valve on the mask may be slipped more or less to one side to allow room air to dilute the anesthetic drawn from the vaporizer. When in place over the hole exiting from the mask, the valve allows no room air in but allows easy exit of the gases inspired by the patient (p 82) [12]. (From Snow J: On the Inhalation of the Vapour of Ether in Surgical Operations: Containing a Description of the Various Stages of Etherization, and a Statement of the Result of Nearly Eighty Operations in Which Ether Has Been Employed In St. George’s and University College Hospitals. London: John Churchill; 1847. pp 1–88.)
Snow made the inspiratory tube leading from his vaporizer large enough to minimize resistance to breathing. And he provided a mask covering mouth and nose and a valve that produced a non-rebreathing system (Fig. 4.3).
He noted (p 21) that “…many of the apparatuses at first invented did not allow of easy respiration, but offered obstructions to it, by sponges, by the ether itself, by valves of insufficient size, but more particularly by tubes of too narrow caliber; and there is reason to believe that, in many instances, this was the cause of failure, and that in others the insensibility, when produced, was partly due to asphyxia….” His valves were “…made of vulcanised India rubber; they (were) light, (were) attached so as to rise with the least appreciable force and they closed again, of themselves, in any posture in which the patient can be required to be placed.”
Snow was a plodding sedulous genius.
Simpson Disagrees with Snow
Simpson disagreed with Snow’s complex approach to anesthetic delivery. Simpson preferred delivery by a few drops of chloroform on a handkerchief. And, in various forms, much of the world agreed with him well into the twentieth century. The handkerchief approach precluded a calibrated delivery, a precision of control over anesthesia depth. Thus it demanded the evaluation of anesthetic effect found in Snow’s degrees to guide anesthetic delivery, but those degrees had a subjective element that made them imperfect guides.
More Observations by Snow
Snow recognized that impurities might compromise the delivery of the ether and described how to secure a purer ether (pp 23–4) [12], particularly by using water to remove the alcohol that was frequently a contaminant. He observed that the water that therefore also entered the ether was salutary (pp 22–3) [12]. “I…allow this small quantity of water to remain in the ether, in order that the air which is inhaled with the vapour of ether may be always saturated also with vapour of water, when it will be more bland, and less irritating, than if it contained but little moisture…”, a finding duplicated a century later with another kind of ether [23]. What a clever fellow.
Snow developed an understanding and delivery of anesthesia with powers of observation and carefully thought out rudimentary apparatus. He had the endearing arrogance of the great anesthetist (p 33) [12]: “…there is no person who cannot be rendered insensible by ether….” No one can resist; no one.
Snow Turns to Chloroform
Like Ross Terrell a century later [24], Simpson and Snow sought the better anesthetic. In 1847, Snow turned his attention to Simpson’s “British” anesthetic. His resulting classic book compared ether and chloroform [13]. The five degrees of anesthesia were essentially unchanged. Snow experimented with animals, making discoveries confirmed a century later. Like later investigators [25], Snow (pp 72–3) [13] found that a greater body temperature increased anesthetic requirement.
Snow Explains Why Chloroform Kills
More than 50 reports of deaths associated with chloroform use appeared in the 10 years following its discovery. Hannah Greener, aged 15, was first, dying at Winlaton, near Newcastle on 28 Jan 1848. Reports came from North America (first, Cincinnati), France (Boulogne), India (Hyderabad), Germany (Berlin), Jamaica (Kingston), Sweden (Stockholm), Austria (Vienna), and on the high seas near Mauritius. But mostly from Great Britain. Snow recognized that chloroform was more dangerous than ether, believing “…that ether is altogether incapable of causing the sudden death by paralysis of the heart, which has caused the accidents which have happened during the administration of chloroform” (p 362) [13]. He thought that the chloroform deaths were preventable, often a consequence of the excessive use of chloroform, producing what he called cardiac syncope. “…accidents from this agent would arise by its suddenly paralyzing the heart, if it were not sufficiently diluted with air; and a careful review of all the recorded cases of fatal accident shows that nearly every one of them has happened in this way….” (p 251) [13].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







