193 The Emergency Psychiatric Assessment
• The emergency psychiatric evaluation is a focused medical assessment with the primary goal of distinguishing between acute medical and psychiatric conditions.
• Primary mental disorders include disturbances in thought, mood, or personality. The onset of such disorders generally occurs at younger ages.
• Delirium and dementia are causes of global cognitive impairment that may be mistaken for psychiatric disease in emergency department patients, especially the elderly.
• Approximately 50% of patients seeking emergency psychiatric services have a poorly treated or undiagnosed medical illness contributing to their symptoms.
• Provisional diagnoses should drive the need for and extent of diagnostic testing.
• Acute interventions should improve the patient’s cooperation, reduce agitation, prevent secondary harm, and initiate treatment of the primary mental disorder.
Epidemiology
Cases of psychiatric illness in emergency department (ED) patients have increased 15% in the past decade and now account for 6% of ED visits. Declining inpatient psychiatric beds and limited community mental health resources complicate the care for this population of patients.1
Pediatric ED visits for psychiatric illness are less well studied, although the predominance of cases occur in the adolescent age group. Suicide prevention is the overriding concern. Teen suicide has tripled since 1950 and is the third leading cause of death in adolescents.2
Pathophysiology
Controversy surrounds the “medical clearance” process, more appropriately referred to as the “focused medical assessment.” The evidence available to guide emergency practice remains limited and conflicting. Much of the debate revolves around the differing expectations and priorities of emergency physicians (EPs) and psychiatric consultants. The responsibilities of the EP are to obtain an appropriate history, identify the degree of stress, rule out medical cause, recognize the need for developing specific interventions, arrange psychiatric consultation, and plan disposition.3
Definitions
The fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) distinguishes “mental disorders that are due to a general medical condition” from “primary mental disorders.”4 The terms organic and functional are no longer used to differentiate between illnesses of medical and psychiatric origin (Box 193.1). Clinical practice teaches us that the separation between mental and medical causes is often blurred.
Box 193.1 Medical Causes of Disturbed Behavior versus Primary Mental Disorders
Dementia
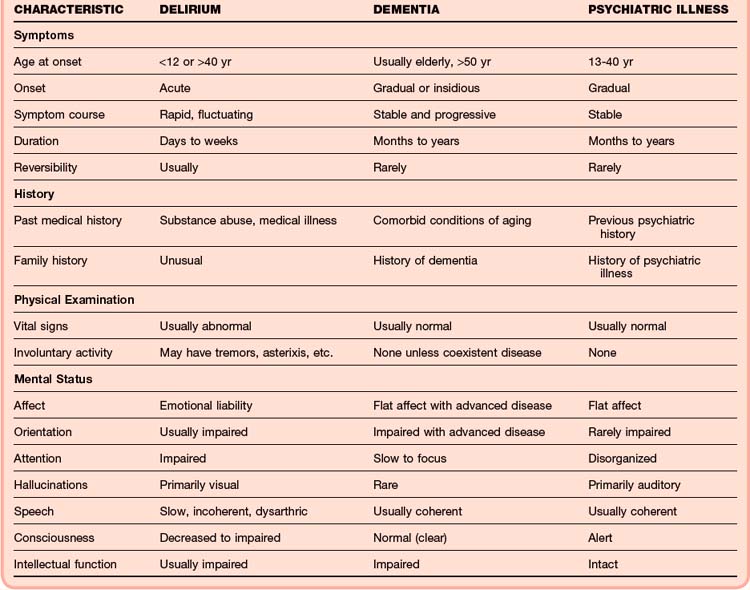
Pervasive disturbance of cognitive function is the hallmark of dementia. Deficits commonly involve memory, judgment, personality, and language. Patients have no clouding of consciousness. The earliest sign of dementia is subtle memory loss, which may promote anxiety, depression, and psychosis. Patients with dementia may experience an acute worsening of symptoms when stressors overwhelm their intellectual and physiologic reserves. As the disease progresses, patients become less capable of recognizing concomitant medical illnesses (Table 193.1).
Presenting Signs and Symptoms
The prevalence of coexisting medical illness in psychiatric patients has been reported to be as high as 50%.1 Untreated medical illness often causes deterioration of baseline cognitive function in patients with a known psychiatric disorder. The prevalence of medical disease in patients seen in the ED with an acute exacerbation of an existing mental illness may be as high as 80%.3 Up to 50% of patients demonstrate a causal relationship between acute medical and psychiatric complaints.5 Five groups are regarded to be at high risk for medical illness: older patients, patients with history of substance abuse, patients without a psychiatric diagnosis, patients with preexisting medical disorders, and patients from a lower socioeconomic level.6
The EP must answer six key questions during the focused medical assessment:
1. Is the patient stable or unstable?
2. Is the behavior the result of an underlying medical illness?
3. What is the severity of the primary mental disorder?
4. Is psychiatric consultation necessary?
5. Does the patient need to be detained to facilitate emergency treatment?
6. What capability does the psychiatric facility have to treat medical conditions?
History
A focused history of the present illness that reviews current symptoms, elicits precipitating circumstances, assesses risk severity, and establishes a time course should be obtained. Critical historical elements include past medical and psychiatric illnesses, medication use (Table 193.2), substance abuse or addiction, and a family history of psychiatric illnesses.
Table 193.2 Medications That Cause Psychiatric Symptoms
| DRUG CLASS | REACTIONS |
|---|---|
| Amphetamines | |
| Antibiotics | |
| Anticholinergics | |
| Antidepressants | |
| Antiepileptics | |
| Antihypertensives | |
| Barbiturates | |
| Benzodiazepines | |
| Dopamine receptor agonists | |
| Histamine receptor antagonists | |
| Nonsteroidal antiinflammatory agents | |
| Opioids | |
| Procaine derivatives | |
| Salicylates | |
| Statins (HMG-CoA reductase inhibitors) |