147 Tetanus
 Epidemiology
Epidemiology
Tetanus is now rare in the Western world, with only 28 cases in the United States in 2007,1 but it is still a common problem in developing countries, where 80% of cases occur in Africa and Southeast Asia. Immunization programs targeting infants and pregnant women have coincided with a decline in the incidence of tetanus over recent years, but the estimated global incidence remains high, with an estimated 290,000 people dying from the disease in 2006.2 In developing countries, neonatal deaths account for a large proportion of cases, and maternal and neonatal tetanus are responsible for an estimated 180,000 deaths/year (Figure 147-1).3 In developed countries, the elderly are particularly at risk, owing to missed boosters and reduced antibody levels.4 Drug users are also at risk from injection site contamination, especially those using subcutaneous administration methods. Up to 18% of infections in the United States occur in injecting drug users.
 Pathophysiology
Pathophysiology
Tetanus is caused by a potent neurotoxin from the gram-positive bacterium, C. tetani (Figure 147-2). C. tetani is a ubiquitous organism capable of surviving in the environment as highly resistant spores and has been isolated from soil, street dust, and human and animal feces.5 Once in a suitable anaerobic environment, these spores germinate, the bacteria multiply, and toxin is released. The most common sources of infection are minor lacerations to the limbs or the umbilical stump in neonates (Figure 147-3).6 In 20% of cases, no source of infection can be found.7 More unusual entry sites include dental infection, ear piercing, unsterile surgery, or injections.
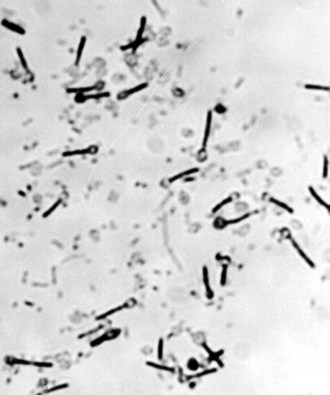
Figure 147-2 Clostridium tetani: a gram-positive bacillus with terminal spores.
(Courtesy J. Campbell, Oxford University Clinical Research Unit, Hospital for Tropical Diseases, Ho Chi Minh City, Vietnam.)
Tetanus toxin is preferentially taken up by motor nerves, either locally or after circulation in the bloodstream. It enters the nerve and is transported by a specific component of the neuronal retrograde transportation system up the axon. It crosses the synapse and enters the γ-aminobutyric acid (GABA) G presynaptic nerve terminal.8 The toxin is a zinc-dependent endopeptidase and cleaves vesicle-associated membrane protein II (VAMP II, or synaptobrevin) at a single peptide bond. This molecule is essential for synaptic release of neurotransmitters, and cleavage disrupts synaptic transmission. The toxin preferentially affects the GABA inhibitory interneurons afferent to motor nerves in the spinal cord and brainstem. By preventing inhibitory discharge, unrestricted motor nerve activity occurs, resulting in the increased muscle tone and spasms characteristic of tetanus. In severe forms of tetanus, the autonomic nervous system is also affected, perhaps as a result of toxin action within the brainstem, giving rise to marked cardiovascular instability.9,10
 Clinical Features
Clinical Features
Two main forms of tetanus exist. The majority of tetanus cases are generalized, affecting all muscle groups. However, a milder form—localized tetanus—also exists, affecting muscle groups in the immediate vicinity of a wound. A subgroup of localized tetanus—cephalic tetanus—is also recognized and is associated with a higher mortality,11 perhaps owing to early laryngospasm or autonomic disturbance resulting from brainstem involvement. Cephalic tetanus is often associated with lower motor neuron palsies affecting the third or seventh cranial nerves (Figure 147-4). Localized tetanus of any variety may progress to the generalized form.
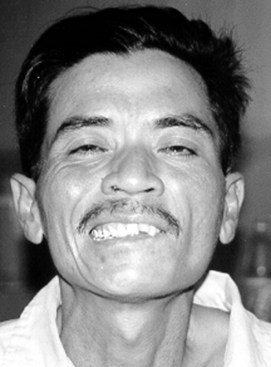
Figure 147-4 Cephalic tetanus associated with lower motor neuron palsy of seventh cranial nerve on left side of face.
After infection, a period of time known as the incubation period elapses before symptoms arise; this period is usually between 4 and 14 days. Initial symptoms include muscle stiffness, with muscle groups with short neuronal pathways affected first; hence, trismus and back pain are present in most cases on admission. Involvement of the facial and pharyngeal muscles produce the characteristic “risus sardonicus” and dysphagia (Figure 147-5). Increased tone in the muscles of the trunk results in opisthotonus. Muscle groups adjacent to the initial site of infection are often particularly severely affected, producing an asymmetric picture.
The time from the first symptom to the first spasm is termed the period of onset. Both the period of onset and incubation period have prognostic significance, with shorter times being associated with more severe disease (<48 hours for period of onset and <7 days for incubation period).12 Spasms may be spontaneous but can also be provoked by physical or emotional stimuli. Laryngospasm can occur early in the disease process, often in isolation, resulting in acute upper airway obstruction. Respiration may also be affected by spasms involving the chest muscles. Without facilities for mechanical ventilation, respiratory failure due to muscle spasm is the most common cause of death.5 Hypoxia is common in tetanus,13 either due to spasms or difficulties clearing the copious bronchial secretions and aspiration.
Muscle spasms are usually most severe during the first and second weeks of illness but may persist for 3 to 4 weeks, after which rigidity may remain for several more weeks. In severe tetanus, autonomic disturbance usually appears during the second week. Signs of sympathetic overactivity usually predominate, evident as periods of tachycardia and hypertension. Severe tetanus is associated with a hyperkinetic circulation, particularly if muscle spasms are poorly controlled.14 Changes in blood pressure are mainly due to changes in systemic vascular resistance, with little alteration in the cardiac index.15 Circulating catecholamines, in particular epinephrine, are increased in patients with tetanus compared to others with similar-severity critical illness.16
Acute renal failure is a recognized complication of tetanus, with dehydration, rhabdomyolysis due to spasms, and autonomic disturbance all contributing.17,18 Other complications include tendon avulsions, vertebral fractures secondary to muscle spasm, gastrointestinal bleeding, venous thrombosis, and thromboembolism (Table 147-1).19
TABLE 147-1 Complications of Tetanus
| System | Complication |
|---|---|
| Cardiovascular | Hyper/hypotension |
| Tachy/bradycardia | |
| Arrhythmias | |
| Ischemia | |
| Venous thrombosis/thromboembolism | |
| Respiratory | Type I and type II respiratory failure |
| Acute respiratory distress syndrome (ARDS) | |
| Aspiration pneumonia | |
| Ventilator-associated pneumonia | |
| Other | Acute renal failure |
| Gastrointestinal bleeding | |
| Sepsis | |
| Vertebral fractures | |
| Bed sores |








