Figure 11.1. Sympathetic nervous system pathways. Sympathetic preganglionic cell bodies reside in the intermediolateral gray matter of the spinal cord (T1-L2) and receive input from neurons descending from the brainstem and from local interneurons. Preganglionic sympathetic fibers (cholinergic) exit the spinal cord within the corresponding spinal nerve and enter the sympathetic chain ganglia through the white rami communicantes where they may (i) synapse with a postganglionic sympathetic neurons (adrenergic), (ii) pass through the sympathetic chain ganglion without synapsing and reenter the spinal nerve of origin through the gray rami communicantes and synapse with a postganglionic neuron in one of the distant prevertebral ganglia, or (iii) travel along the sympathetic chain to synapse with a postganglionic neuron in a different ganglion in the sympathetic chain.
b. There is a great deal of overlap in sympathetic innervation so that a single spinal nerve may carry sympathetic activity arising in multiple spinal cord segments.
3. The preganglionic neuron may pass through the paravertebral ganglion to synapse with the postganglionic neuron in a prevertebral ganglion (e.g., superior cervical, superior mesenteric) or the adrenal gland.
C. Plexuses. Aggregations of sympathetic nerves and prevertebral ganglia in the thoracic, abdominal, and pelvic cavities are termed plexuses. There are four generally recognized plexuses: cardiac, pulmonary, celiac, and hypogastric, which innervate the heart, lungs, abdominal viscera, and pelvic organs, respectively.
1. Plexuses lie along the anterior aspect of the vertebral bodies or the aorta and the nerves derived from them course along nearby blood vessels to reach their target organs.
III. Indications
A. Autonomic indications. Blocks performed specifically to interrupt sympathetic nervous system activity are generally done to produce vasodilatation in an effort to improve blood flow in a particular area (1) or to treat hyperhydrosis. For example, block of the sympathetic chain has been used successfully to increase blood flow in the setting of vascular insufficiency, particularly in patients who are not candidates for surgical revascularization (2). More recently, stellate ganglion block has been shown to be effective in producing long-lasting (weeks to months) relief from severe “hot flashes” associated with menopause (3).
B. Sensory indications. Sympathetic blocks are probably most often used to treat malignant and nonmalignant pain. In this context, they are employed not to block the sympathetic ganglia per se; rather the intent is to block afferent sensory fibers that travel with the sympathetic fibers and pass through or near the sympathetic ganglion. Blockade of the celiac plexus to treat malignant and nonmalignant intra-abdominal pain is a classic example. Celiac plexus blockade combined with intercostal blocks can be used for upper abdominal surgery. Ganglionic blockade has also been used to supplement surgical general anesthesia and to provide postoperative analgesia.
IV. Drugs
A. Local anesthetics. All local anesthetics used for peripheral nerve blocks are appropriate for ganglionic blocks. Because motor block is not an issue when performing ganglionic blocks (there are no somatic motor fibers present), dilute local anesthetic solutions can be used if desired (e.g., 0.25% bupivacaine, 0.5% lidocaine). Shorter-acting agents might be useful for diagnostic blocks or for efficacy trials before surgical extirpation or neurolytic block.
B. Neurolytic agents. Both alcohol and phenol have been used successfully to produce neurolytic block of ganglia. Alcohol is often preferred for use around great vessels (e.g., celiac block) because it is thought to be less likely to damage them. Both agents can cause unintended damage to nearby neural structures, for example, spinal nerves or spinal cord.
V. Specific blocks
A. Stellate ganglion block
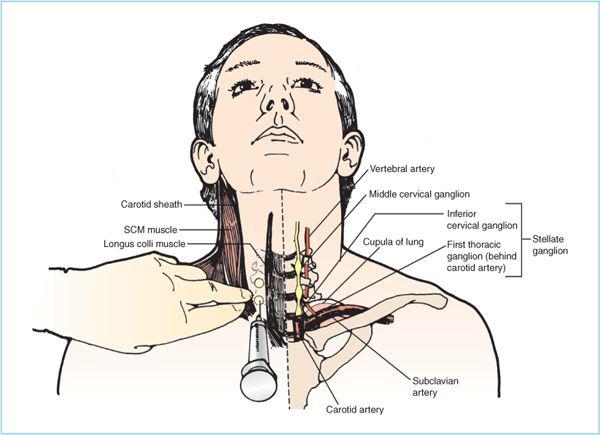
1. Anatomy. The stellate ganglia are formed by a variable fusion of the first (sometimes second, third, and even fourth) thoracic ganglion and the lower two cervical segmental ganglia, which is why it is sometimes called the cervicothoracic ganglion. Position is somewhat variable but “on average” the ganglion lies just anterior to the lateral edge of the C7 and T1 vertebral bodies. At this level, a good portion of the ganglion is behind the vertebral and subclavian arteries and medial to the cupola of the lung (Figure 11.2).
Figure 11.2. Stellate ganglion block. The stellate ganglion is formed by a variable fusion of the first thoracic (sometimes second, third, and fourth as well) and inferior cervical ganglia (sometimes middle cervical ganglion also). The ganglion generally lies along the lateral border of C7 and T1 vertebrae sometimes extending to the inferior edge of C6 or as low as T4. The bulk of the ganglion lies posterior to the carotid and vertebral arteries and posteromedial to the cupula of the lung. Because of the proximity of multiple “high-risk” structures the block is usually performed at the level of the C6 or C7 transverse processes and sufficient volume (7–10 mL) is used to assure sufficient inferior spread. SCM, sternocleidomastoid.
a. Because of the proximity of multiple “high-risk” structures, the stellate ganglion is generally not blocked directly. Rather the block is made at the C6 or C7 transverse process and ganglionic blockade relies on administration of a sufficient local anesthetic volume to spread caudally to reach the ganglion. Direct block of the ganglion, as would be needed for neurolytic drugs, is probably best accomplished under CT guidance.
2. Technique
a. Position the patient supine with the neck in slight extension.
b. Skin landmarks. Mark the cricoid cartilage and the medial border of the sternocleidomastoid muscle on the side to be blocked. Approximately 2 cm lateral to the edge of the cricoid cartilage, palpate the tubercle of the C6 vertebral process (Chassaignac tubercle). This is usually the most prominent transverse process in the neck. Mark the skin overlying the tubercle. If the block is to be made at C7, place a second mark approximately 2 cm directly caudad of the mark overlying the C6 tubercle. This second mark will lie over the C7 transverse process.
c. After aseptic preparation, raise a skin wheal at the mark to be used for the block.
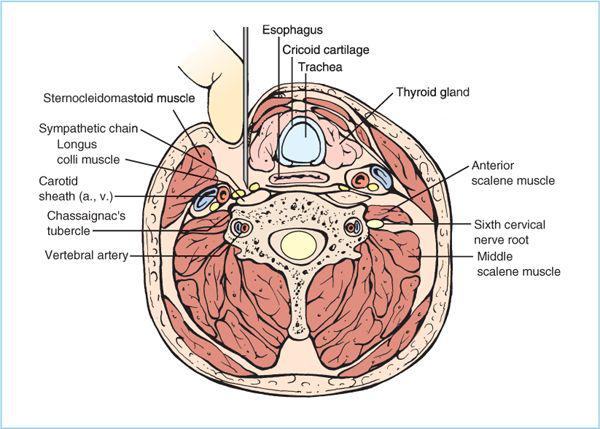
d. Whether performing the block at C6 or C7, gently retract the sternocleidomastoid muscle and carotid artery laterally and insert a 22- or 25-gauge 6-cm needle directly posterior until bone is contacted (Figure 11.3). If bone is not contacted within 5 cm, redirect the needle slightly medially and reinsert. If this fails, slight caudad or cephalad angulation may be required. If the desired tubercle is not easily contacted, reassess the landmarks.
(1) If a brachial plexus paresthesia is elicited, the needle is too far lateral and posterior—redirect accordingly.
e. After contacting bone, withdraw the needle approximately 2 mm so that the needle tip lies above the longus colli muscle in the plane of the ganglion. Gently aspirate looking for blood or cerebrospinal fluid (CSF). If aspiration is negative, very slowly inject 2 mL local anesthetic while observing the patient carefully for central nervous system (CNS) changes. Importantly, if the needle is in the vertebral artery a local anesthetic dose as small as 0.5 mL can produce seizures (4). If the test dose is negative, incrementally inject an additional 5 to 10 mL local anesthetic with frequent aspiration and constant assessment of mental status.
Figure 11.3. Cross-section of stellate ganglion block. Palpate the tubercle of C6 and retract the sternocleidomastoid muscle and carotid sheath laterally. Insert the needle onto the tubercle. Once bone is contacted, withdraw the needle approximately 2 mm so that the needle tip lies above the longus colli muscle. The stellate ganglion lies caudad to the C6 vertebral body and block results from caudal spread of local anesthetic. At this level, only fibers of the sympathetic chain running between the stellate ganglion and the middle cervical ganglion are present. The block is performed similarly at C7 (see text).
3. Signs/symptoms of block. Stellate ganglion block will result in Horner syndrome (ptosis, miosis, facial anhidrosis, enophthalmos, and injected sclera) within 10 minutes. Also, nasal congestion and varying degrees of vasodilatation of the arm will likely occur.
4. C6 versus C7 approach. The C6 approach offers the potential benefit of a lower risk of pneumothorax and intravascular injection. However, sympathetic block of the upper extremity is more complete when the block is performed at C7.
5. Complications. Complications of stellate ganglion block include the following:
a. Hematoma/hemorrhage
b. Pneumothorax
c. Intravascular injection/systemic toxicity
d. Epidural/intrathecal injection
e. Spinal cord trauma
f. Unintended nerve blocks. Vagus, phrenic, recurrent laryngeal, and other nerves can be blocked either by inaccurate needle placement or by excessive local anesthetic spread.
g. Physiological effects. Stellate ganglion block can both shorten (left-sided block) and prolong (right-sided block) QTc; therefore, care should be exercised in patients with preexisting prolonged QTc (5). Stellate ganglion block also decreases cerebrovascular resistance on the ipsilateral side resulting in increased blood flow to that side and a simultaneous decrease on the contralateral side. Whether this poses a risk to patients with cerebrovascular or carotid vascular disease is unknown.
B. Celiac plexus block
1. Anatomy (Figure 11.4)
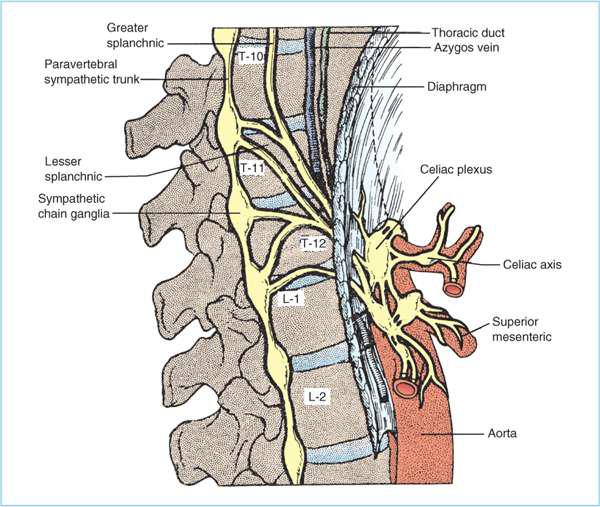
a. Location. The celiac plexus is a variable collection of ganglia and autonomic nerves (both sympathetic and parasympathetic) located anterior to the aorta at the level of the T12 to L1 vertebral bodies (lower on the left than the right).
b. Ganglia. The number of ganglia present in the celiac plexus has been found to range from 2 to 10 with an average of 5.5 (6).
c. Innervation. The celiac plexus receives sympathetic preganglionic fibers from the greater, lesser, and least splanchnic nerves. The greater and lesser splanchnics course from their spinal segments of origin through the mediastinum to pierce the diaphragmatic crura to reach the celiac plexus. The splanchnic or retrocrural approach to the celiac plexus block aims to block these nerves as opposed to the plexus per se. The least splanchnic nerve is derived from the lumbar sympathetic chain ganglia.
Parasympathetic nerves from the vagus also pass through the celiac plexus as do afferent sensory fibers originating in the abdominal organs. It is these afferent sensory fibers that are generally being targeted by celiac plexus block.
Sympathetic postganglionic fibers are distributed to most of the organs of the upper abdomen including liver, spleen, stomach, pancreas, kidneys, small bowel, and large bowel to the splenic flexure.
Figure 11.4. Celiac plexus anatomy: The celiac plexus comprises a variable number of sympathetic ganglia and associated nerves straddling the aorta near the takeoff of the celiac and superior mesenteric arteries. Sympathetic afferents reach the plexus through the greater, lesser, and least splanchnic nerves and sympathetic efferent nerves course along the arterial branches arising from the aorta to supply blood to abdominal organs and viscera. Parasympathetic fibers from the vagus and afferent sensory fibers from the abdomen also travel through the celiac plexus.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree