Figure 5.1. The three-ring (“control”) syringe. This adaptation to the plunger of a standard 10-mL syringe allows greater control of injection, easier aspiration, and the opportunity to refill the syringe with one hand.
5. The connection to the hub of the needle affects the ease of fixation of the needle. The Luer-Lok adapter, which screws tightly onto the matching needle hub, does not require forceful friction to provide a seal and is therefore less likely to cause unwanted movement of the needle when attaching the syringe. This coupling also provides a connection less likely to leak on injection. A tight seal is critical when using resistance to identify the epidural space.
6. Therefore, an ideal tray would have Luer-Lok syringes in 1-, 3-, and 10-mL sizes with a three-ring adapter on the latter, plus a glass syringe for epidural localization.
III. Needles
Although local infiltration can be performed with almost any needle, special adaptations can facilitate success with regional techniques.
A. Regional-block needles
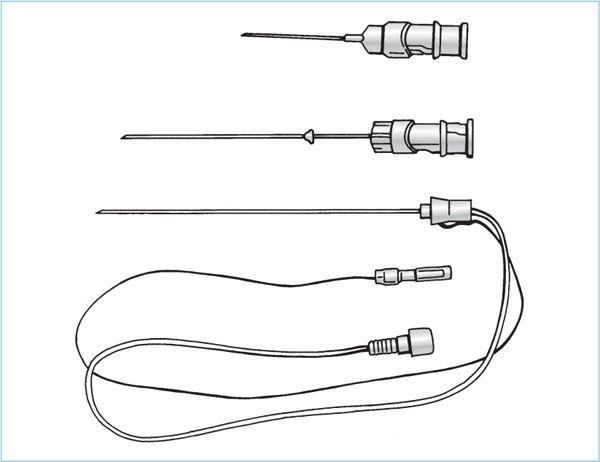
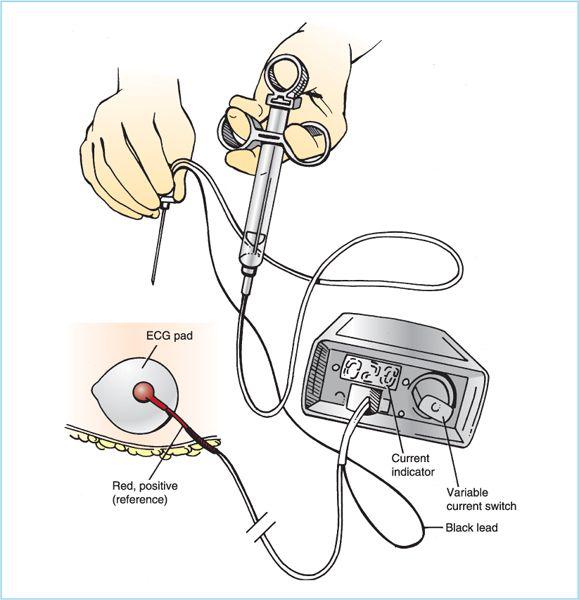
1. Peripheral nerve blocks are most commonly performed with special needles adapted for use with nerve stimulators (see subsequent text). These needles are usually approximately 22 gauge in size, with a specially adapted Luer-Lok hub or side-arm extension that includes a 20- to 40-cm (8- to 16-in.) wire connection for attachment to the negative lead of the nerve stimulator (Figure 5.2). The needles are also sheathed with a nonconducting cover to concentrate the electrical current at the tip, which is most commonly a short-beveled design. The incidence of nerve injury is presumed to be less with shorter-bevel needles (16 versus 12 degrees) (Figure 5.2). The short-bevel needle may offer more resistance to advancement. Larger (19 gauge) insulated stimulating needles are also available with curved tips that allow passage of catheters.
2. Regional anesthetics can also be performed with traditional unsheathed needles using the paresthesia technique or localization with other landmarks. The gauge employed is a compromise between ease of injection and discomfort caused. Smaller needles (25 to 32 gauge) are best for skin infiltration because their insertion is less uncomfortable. The 23-gauge size is suitable for superficial blocks, such as axillary or intercostals on thin patients. A larger, more rigid shaft is usually required for any deeper needle insertions. The 22-gauge 38 or 50 mm (1.5- or 2-in.) size is needed for most regional techniques. A 127 or 152 mm (5- or 6-in.) 20-gauge needle is used for deep blocks, such as the celiac plexus, where free aspiration is desired.
Figure 5.2. Regional anesthesia needles. For superficial blocks, such as the axillary, short 25-gauge needles (top) with a shorter-bevel angle (compared to standard Quincke-type needle points) are very effective. For deeper injections, longer needles may be equipped with a “safety bead” on the upper shaft (middle) to prevent loss of the needle in the subcutaneous tissue if it separates from the hub. Needles used for peripheral nerve stimulator blocks (bottom) include the direct attachment for the nerve stimulator connection and the short tubing for the injection syringe. This tubing serves to remove the weight of the syringe from the needle hub, allowing finer control.
B. Spinal needles
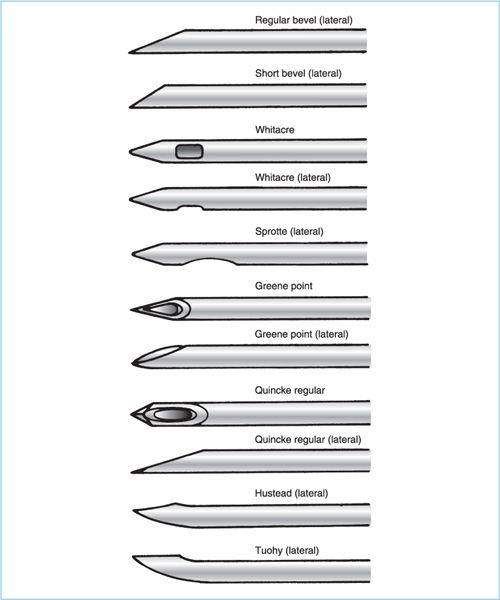
1. Spinal needles are necessarily longer (90–127 mm [3.5–6 in.]) and usually styletted to prevent occluding the lumen with a plug of skin or subcutaneous tissue before the dura is punctured. A number of bevel designs have been introduced since the original Quincke (sharp bevel) style was first used, and most are designated by the name of their inventor (Figure 5.3). The rounded Greene and Whitacre points are designed to be less traumatic to the dura itself, apparently splitting or spreading rather than cutting the longitudinal fibers, thereby promoting more rapid sealing of the dural hole. Experience with the rounded-bevel design (especially the Whitacre and the Sprotte derivation of it) has shown an impressive reduction in the incidence of postdural puncture headache.
Figure 5.3. Standard regional anesthesia needle bevels.
2. The gauge of spinal needles is also important in terms of the probability of a headache, although it is apparently not as important as the needle type (see Chapter 6). Smaller needles create smaller holes and less transdural leak, but they are more difficult to insert and to aspirate. The 25-gauge rounded-bevel needle is the size most frequently chosen as a reasonable compromise.
C. Epidural needles
1. Epidural needles are of a larger gauge, both to permit better assessment of loss of resistance and to allow the passage of catheters. An 18-gauge thin-walled needle is the smallest that will pass a 20-gauge catheter, and 16- or 17-gauge needles are commonly used for catheters. A 19-gauge needle is satisfactory for single injections. A 22-gauge needle has been used, but the perception of resistance is more challenging through the narrower opening.
2. A conventional Quincke-point needle can be used for a single injection technique, although some practitioners prefer the blunter, short-beveled Crawford needle for epidural or caudal insertion. The Tuohy needle with a curved point was first introduced to facilitate the passage of catheters. Hustead modified this needle to reduce the bevel angle slightly in the hope of reducing the chance of shearing the catheter during passage (Figure 5.3). The angle of both of these bevels may allow better direction of the catheter into the main axis of the epidural canal, but the greater curvature and the offset of the point of the needle from the mid axis of the shaft also make them more likely to deviate from the intended path during advancement. The longer bevel also creates the possibility that the tip of the needle may communicate a loss of resistance before the full opening of the bevel is completely through the ligamentum flavum. These needles may need to be advanced another 2 to 3 mm beyond their initial penetration of the ligament before a catheter will pass. Most of these needles are manufactured with 1-cm markings along the shaft to allow better appreciation of the needle depth or movement.
3. Tuohy needles have also been manufactured with additional channels and end holes to facilitate simultaneous insertion of spinal needles for combined spinal–epidural (CSE) anesthesia (2).
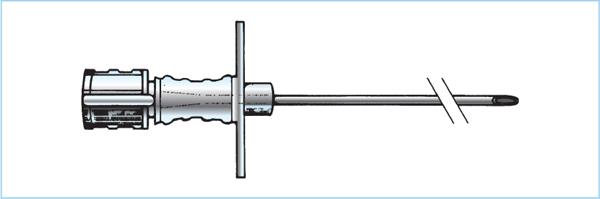
4. The hubs of epidural needles have also been adapted in some cases with “wings” to allow better control of the depth of advancement, particularly in the thoracic region (Figure 5.4).
Figure 5.4. Wing adapters on needle hub. The flanges attached to the hub of a standard epidural needle allow greater control of the advancement of the tip when the flanges are grasped between the thumb and forefinger while the other fingers rest on the skin and control the depth of insertion. These flanges come in several modifications.
D. Introducers are useful in spinal and epidural anesthesia. These are short, large-bore, sharp-pointed needles. For spinal anesthesia, these can be inserted through the skin and into the interspinous ligament. They create a rigid path to guide the more flexible small-gauge spinal needles. They offer the added advantage of allowing the tip of the spinal needle to bypass the skin and therefore avoid contamination with preparatory solution or residual skin bacteria. For epidural use, a skin hole made with these needles reduces the resistance to insertion of the epidural needle and allows more sensitive appreciation of the ligaments themselves.
IV. Catheters
A. A multitude of catheters is available for insertion through epidural or peripheral nerve block needles.
1. For basic catheters, the primary difference among them is the construction material, which gives different performance characteristics. Newer catheters of nylon, polyamide, or polyvinyl offer compromises between flexibility (increased risk of kinking) and rigidity (risk of puncturing dura or veins), and the appropriate balance is a matter of personal choice among the wide selection available.
2. Another feature offered in epidural catheters is the presence of lateral injection ports proximal to a closed, soft-tip end. This may reduce the chance of dural puncture, and the presence of multiple holes reduces the chance of occlusion of the catheter by tissue or blood clot blocking a single hole. However, multiple holes may also allow unrecognized dural or venous puncture, because a test dose may not give a reliable response if only one hole is in a vessel or into the dura. Many practitioners prefer a single-port catheter for this reason. On the other hand, aspiration is more likely to be an effective test with multiple-orifice catheters (3).
3. Marks at 1- or 5-cm (0.5–2 in.) intervals along the first 20 cm (8 in.) are useful in guiding insertion of the catheter to the correct depth. Radiopaque markers on the catheter are useful in documenting position of chronic indwelling catheters or catheters for injection of neurolytic agents. The selection of any or all of these features is again a matter of personal experience and choice.
4. A spring-wire reinforced flexible catheter combines the ideal features of easy passage, minimal trauma, and low risk of occlusion or migration. If the catheter is to remain in place for several days for postoperative analgesia, these devices allow adaptation of the catheter to patient movement, and may reduce the frequency of catheter migration.
5. The most complex version of the continuous catheter is the addition of a stimulating wire to the tip of a catheter for continuous peripheral nerve block. Use of such catheters allows continuous identification of the nerve as the catheter is advanced, and may increase the probability of effective location of the tip after full insertion (4), although at a higher cost.
B. Adapters are needed to allow injection from a syringe into a catheter. These are usually of the Tuohy-Borst type, where screwing one fitting onto another tightens a rubber sleeve around the catheter and holds it in place. There are as many connectors available as there are catheters, and the selection is again a personal choice based on cost, reliability, and ease of use. All connectors should have a Luer-Lok adapter for fitting a syringe and a cap to provide sterility of the fitting between injections. All catheters used for repeated injections on surgical wards should be clearly labeled as epidural or peripheral nerve catheters, ideally with a colored label, to prevent unintentional injection of intravenous drugs.
C. Epidural catheters can also be inserted into the subarachnoid space, although the larger needles used for the standard catheters may increase the risk of headache. At one point, smaller microcatheters (27 gauge or smaller) were employed through smaller needles to reduce this problem. Unfortunately, problems with neurotoxicity (see Chapter 3) led to their withdrawal from the market.
V. Infusion devices
In the last 10 years, anesthesiologists have become more actively involved in the continuation of regional techniques in the postoperative period for pain relief (see Chapter 23). There are several continuous-infusion devices available to assist in the delivery of local anesthetics or local anesthetic–opioid mixtures for postoperative pain relief (5).
A. For inpatient use, there are small electrically driven pumps that provide, in addition to a continuous infusion, a patient-controlled option that allows supplemental doses at times of increased need. These devices are individually programmable and demonstrate a high degree of flexibility. They usually contain a locked chamber for the infusion itself, because opioids are used commonly in this setting. It is important that such devices have the potential for a continuous infusion, as well as a lockout interval to prevent excessive dosage by the patients. Mechanical failures with such devices are rare, and they are highly effective for inpatient postoperative analgesia.
B. The use of continuous catheters for peripheral nerve blocks also benefits from the attachment of a continuous-infusion pump. Several modalities are available.
1. The simplest are elastomeric bulbs that contain a fixed amount of local anesthetic under a constant pressure, which is then delivered at a fixed rate through a flow valve connected to the catheter. These pumps can provide continuous infusions for 24 to 48 hours for brachial plexus and lower-extremity analgesia. The limitation of the elastomeric pumps is the fixed delivery volume, although newer devices have added a bolus capacity.
2. There are also spring-loaded mechanical pumps that are similar to the bulbs in their simplicity. They also rely on a constant tension to deliver the solution, and have been equipped with bolus capability.
3. Alternatively, small battery-operated, programmable, mechanical pumps are available, which have the same options as the inpatient infusion devices; that is, they can deliver both continuous infusion and incremental additional boluses on patient demand. Again, mechanical problems with these pumps are rare and they appear to provide a useful option for prolonging postoperative analgesia in both inpatients and outpatients.
VI. Nerve localization
Although many blocks can be performed using simple injection around an easily identified landmark (saphenous nerve at the knee, perivascular axillary block), deeper injections require confirmation of nerve localization. The historical method is to elicit a paresthesia. Recent advances allow easier identification, and may reduce the chance of unintentional nerve injury.
Figure 5.5. Nerve stimulator attached to regional-block needle. The negative (black) lead is attached to the exploring needle, whereas the positive (red) is connected to a reference electrocardiogram (ECG) pad used as a “ground.” The stimulator is set to deliver 1 to 2 mA of current to detect the nerve. The current is reduced further as the needle is advanced closer to the nerve. Motor stimulation at a current of 0.5 mA or less suggests that the needle is adjacent to the nerve.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree