(1)
Chennai Breast Centre, Chennai, India
At least six prospective randomized studies have shown the equivalence for breast-conserving treatment and mastectomy. Breast conservation rates vary in different countries. Other than technical considerations, factors like cost, availability of radiotherapy facilities, follow-up, and medical professional’s views on breast conservation have influenced the practice of breast conservation.
The aim of breast conservation is to minimize local recurrence and achieve a good cosmetic outcome. Failure to offer breast-conserving treatment to suitable and appropriate patients is becoming a medicolegal issue. The exact reasons why a person who fulfills the criteria for breast conservation surgery is treated by mastectomy should be recorded in the case notes.
For breast conservation to be successful, it must be possible to ensure the following criteria is met with:
1.
Achieve clear margins
2.
Access to good radiotherapy
3.
Follow-up to detect local recurrence promptly
Breast conservation is associated with a higher risk of recurrence when it is not followed up with radiotherapy after surgery and when cut margins are positive. Earlier it was thought that local control had no influence on overall survival, but the EBTCG meta-analysis has shown that optimal local therapy does offer a survival advantage.
The definition of free margin has been extensively debated. It is now widely accepted that a 1 mm free margin is acceptable for an invasive carcinoma and for ductal carcinoma in situ a 2 mm margin would be required. Young age, presence of extensive intraduct component, and presence of lymphovascular emboli are also risk factors for local recurrence after breast conservation therapy.
Accurate preoperative assessment of the size and the extent of the tumor is essential for deciding whether breast conservation surgery is an option to mastectomy. Routine methods for assessing the extent of the disease include a clinical examination, mammography, breast ultrasound, and MRI of the breast.
Size and Location
The breast size to tumor size ratio is an important determinant in deciding breast conservation. Preoperative chemotherapy or oncoplastic techniques could make it feasible to conserve the breast where the tumor is proportionately bigger than the size of the breast.
Central, medial, and inferior quadrant tumors are challenging to conserve and get good cosmetic outcomes. As normal involution progresses, the medial and inferior parts of the breast are replaced by fat and any volume loss in this area tends to result in very inferior cosmetic results. Oncoplastic procedures may be required to achieve a good cosmetic result.
Extent of the Disease
Estimation of the local extent of the disease is very important for surgical planning. Extensive intraduct carcinoma is a well-known risk factor for increased local recurrence after breast conservation. The presence of microcalcifications within and beyond the mass can be clearly assessed on a mammogram with additional spot compression and air gap magnification views. Breast conservation should not performed in patients with large areas of microcalcifications and with microcalcifications extending up to the nipple. They are best treated by mastectomy (Fig. 40.1). Extensive intraduct carcinoma is defined DCIS involving at least 25 % of borders of invasive duct carcinoma. Predominant intraduct component means that over 75 % of the tumor is DCIS within the lesion. The presence of extensive intraduct carcinoma is a risk factor for local recurrence after breast-conserving surgery (Fig. 40.2a–c).


Fig. 40.1
Irregular pleomorphic calcifications extending up to the nipple. This patient will not be suitable for a nipple-sparing mastectomy
Fig. 40.2
(a–c) Images showing invasive cancer with (a) predominant DCIS, (b) extensive intraductal component, and (c) foci of DCIS in the periphery of the tumor
On breast ultrasound, the duct extensions from the solid invasive component could indicate the extent of ductal carcinoma in situ beyond the lesion. The surgeon often uses his/her finger to guide the excisions, usually a 1 cm concentric margin all around and posteriorly up to chest wall. If the duct extensions are missed, then the possibility of local recurrence is high (Figs. 40.3a, b and 40.4).
Fig. 40.3
(a) Magnification view showing irregular linear calcifications beyond the mass. (b) Wide local excision specimen mammogram confirms the removal of the linear group of calcifications beyond the mass
Fig. 40.4
Ultrasound image showing an irregular hypoechoic mass with a duct extension towards the nipple. The duct is likely to be filled with DCIS. Excision of the palpable mass with the usual 1 cm margin at surgery might miss the duct extension resulting in residual disease with margin positive excisions
DCIS does not respond the same way as invasive cancer does with neoadjuvant chemotherapy. The invasive component may disappear with neoadjuvant chemotherapy but DCIS can persist even after chemotherapy, which makes it difficult to plan conservation even after neoadjuvant chemotherapy.
Multifocal tumors (tumors occurring in the same quadrant) and satellite nodules may be present, which should be taken into account when planning the surgical procedures (Figs. 40.5 and 40.6).
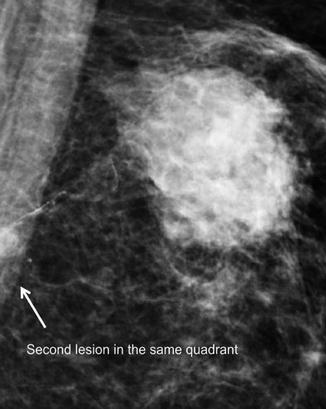

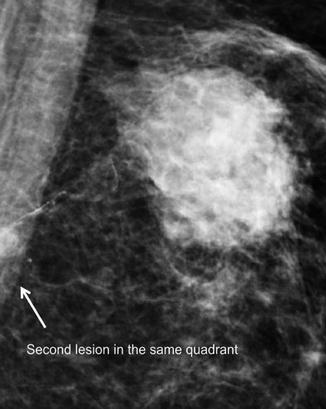
Fig. 40.5
Mammographic image showing a multifocal malignancy

Fig. 40.6
Trapezoidal ultrasound image showing multifocal malignancy
Patients with multicentric tumors (tumor occurring in different quadrants ) in the same breast are not suitable for breast-conserving surgery. They are best treated by mastectomy (Fig. 40.7).
Fig. 40.7
MLO view showing multicentric malignancy involving all quadrants of the breast
The contralateral breast should then be carefully evaluated. It is not uncommon to find bilateral breast cancer and it is too easy to get distracted with the obvious one and miss a subtle contralateral cancer (Fig. 40.7).
Bilateral breast cancers suitable for breast conservation can be treated by bilateral breast conservation (Fig. 40.8).
Fig. 40.8
(a, b) CC and MLO views showing a right-sided circumscribed malignancy and left-sided small spiculated malignancy. (c) Optical magnification of the left MLO view showing a spiculated lesion with architectural distortion. (d) Specimen x-ray, left breast malignancy. (e) Bilateral breast conservation after radiotherapy
Surgical Management of Nonpalpable Breast Cancers
Nonpalpable cancers can be localized prior to surgery by different methods. If the cancer is seen on breast ultrasound, then the lesion can be localized by a skin mark placed over the tumor using an indelible ink with the help of ultrasound or by using hook wire placed under ultrasound guidance.
If the calcifications are seen only on mammogram, then a stereotactic wire guidance will be required to localize the lesion.
Once the lesion is localized with a wire by ultrasound guidance or stereotactic guidance, a mammogram in orthogonal views is taken to confirm the wire’s location (Fig. 40.9a–d).
Fig. 40.9
(a, b) MLO and CC views showing architectural distortion. (c) CC view after wire placement, to check position of wire. (d) Ultrasound-guided hook wire placement has been done
It is also useful to check the location of the tip of the wire on ultrasound. Some of the wires come with a threaded end close to the hook, which reverberates very well and is easy to spot on ultrasound. A skin mark over this area helps the surgeon in planning the incision as it is easier to excise the cancer if the incision is placed directly over the cancer.
The specimen should be oriented and sent for a specimen x-ray to assess the completeness of excision.
The ROLL (Radio occult lesion localization) technique can also be used to localize the lesion. The radioisotope is injected in the area of the tumor and the surgeon uses a gamma probe to locate the tumor and performs the excision.
Breast Conservation Techniques
Removal of more than 10 % of breast volume is likely to result in poor cosmesis without oncoplastic techniques. Therefore, simple excisions should be limited to small tumors. Skin incision should be appropriately placed. The Langer’s lines (lines described around the predominant orientation of collagen fibers) around the breast are circular and incisions around these lines give a better cosmetic results. More recently, Kraissl’s lines have been described, which are the lines of maximum resting skin tension and these run more transversely. Incisions along these lines give the best possible outcomes.
For inferior quadrant lesions, i.e., lesions in the 6’o clock position, a vertical incision should be used. Transverse incisions in the inferior quadrant and tissue loss and approximation in a transverse orientation produces a poor cosmetic result. The distance from the nipple to the inframammary crease is short and any loss of tissue in the transverse orientation further reduces this distance and results in a nipple pointing downwards like a parrot beak. Radial incisions are better in the inferior quadrant. Breast tissue excisions and closure should also be planned in a radial fashion like spokes in a wheel.
For lesions closer to the nipple and areola, a circumareolar approach is useful. For lesions in the upper outer quadrant, it is very tempting to do a combined incision for axillary clearance and breast surgery through the same incision. This must be avoided as it results in poor cosmetic outcomes. However, if only a sentinel lymph node biopsy is required, then it may be possible to do tumor excision and sentinel lymph node biopsy through the same incision as there is no tissue loss after SLNB in the axilla, and a drain in the axilla is not necessary after sentinel lymph node biopsy.
Routine excision of the skin is unnecessary except for very superficial tumors and in tumors producing tethering.
Once the skin incision is made, the skin flaps are raised to 2 cm beyond the lesion with a 1 cm margin all round the tumor. It is not always necessary to resect up to the pectoral fascia for superficial tumors, but for deeper tumors the posterior margin should include the pectoralis fascia. Once the tumor is resected, it should be oriented, weighed, and sent for a specimen x-ray. The specimen x-ray is useful to see if the tumor is close to margins. Some surgeons take a cavity shave separately for margin assessment. Hemostasis is secured and the cavity is marked with liga clips. The breast tissue is mobilized and the defect is closed primarily. If the breast tissue is not mobilized and closed primarily, the seroma in the cavity organizes and the resultant scar cicatrizes and produces an undesirable cosmetic result. It is important to remember that extensive mobilization of the breast tissue in both the premammary zone plane and the retromammary zone plane leads to fat necrosis and a poor cosmetic outcome. In most simple wide local excisions, it is possible for the glandular tissue to flop back to approximate with mobilization just under the skin (premammary zone). Excising the breast tissue in a radial fashion like spokes in a wheel allows the pillars of glandular tissue fall together nicely after simple excisions providing a better cosmetic outcome.
Sometimes, the NAC (nipple areolar complex) is pulled towards the lumpectomy site which affects the cosmetic outcome. This can easily be corrected by recentralizing the NAC. It is performed by excising a crescent of periareolar skin opposite from the lumpectomy site. This simple maneuver prevents the NAC deviation and recentralizes the nipple.
Oncoplastic Techniques
Oncoplastic techniques have made it possible to extend the breast conservation options to many women thereby avoiding a mastectomy. Larger volumes can be resected and the volume lost can be corrected by replacement or displacement techniques. The choice of oncoplastic techniques depends on a number of factors like tumor location, size, breast size and ptosis, surgeons’ skills, and patients’ expectations.
Volume Replacement Technique
Volume replacement should always be considered if the resultant cavity after tumor excision is too large to close primarily. It is particularly useful in patients who wish to avoid contralateral breast procedure to symmetrize and in women with small breasts. The disadvantages of volume replacement include donor site morbidity like donor site scar, seromas, and wound healing problems in the donor site. Flap loss is uncommon but possible, in which case revision surgery will be required. These techniques require additional operating time and prolonged convalescence.
Several approaches are available to replace the volume lost from the breast. Myocutaneous and local adipose tissue-based flaps are very versatile and reliable.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







