(1)
Chennai Breast Centre, Chennai, India
Nipple discharge is a distressing symptom because of the fear of breast cancer associated with it. Approximately 95 % of women presenting with nipple discharge can either have a physiological or benign cause for the discharge.
Physiological Nipple Discharge
It is the fluid discharge from the nipple of a normal breast with no underlying cause of concern. A small quantity of fluid can be expressed in most lactating women and also nonlactating women. This fluid is secreted by apocrine glands and varies from yellow to green to brownish black in color and thin watery to thick sticky secretion. The discharge is usually not spontaneous. The fluid may be seen to be discharged from one or both nipples and multiple ducts on stimulation of the nipple, after a warm bath or during breast compression for mammography.
Duct Ectasia
Duct ectasia is usually due to progressive involution of ducts. With increasing age, the myoepithelial layer of the major ducts loses its elasticity and contractility resulting in progressive duct dilatation and thickening of its walls. The stagnant secretions within the blocked duct get thicker and inspissated. Most women with duct ectasia are asymptomatic and it is often an incidental finding on ultrasound. Some describe a feeling of intense surge resembling the milk surge with breast-feeding. Expressing small amounts of discharge usually helps to relieve the symptoms. Some women present with multiple duct discharge, greenish brown to black nipple discharge. There may also be associated nipple retraction because of shortening of ducts due to repeated inflammation. The retraction is slit-like (letter box nipple) in contrast to retraction due to malignancy, where the entire nipple gets pulled in (Fig. 22.1).


Fig. 22.1
Slit-like nipple retraction seen following recurrent periductal inflammation
Mammographic Features
Mammogram may not show any abnormality in women with duct ectasia. With repeated inflammation, the retroareolar region might appear more dense. Occasionally, a dilated duct may be seen as a faint tubular opacity in the retroareolar region (Fig. 22.2).
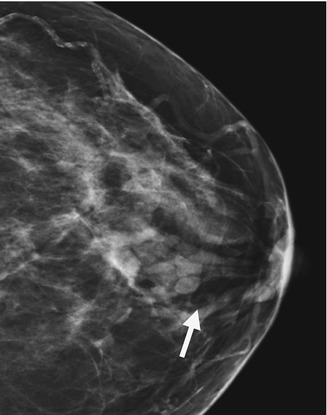
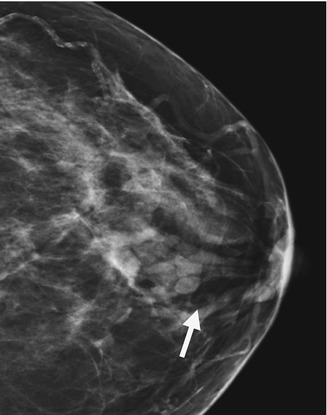
Fig. 22.2
CC view – Arrow shows dilated ductal shadow in the retro areolar region
Ultrasound Features
Duct ectasia is usually bilaterally symmetric. Fluid within the dilated ducts in early stages may be clear and therefore appear anechoic. In later stages, the fluid within the ducts gets thicker with stagnation and absorption, appearing mildly echogenic to hypoechoic fluid within the dilated duct in the retroareolar region (Fig. 22.3a, b).
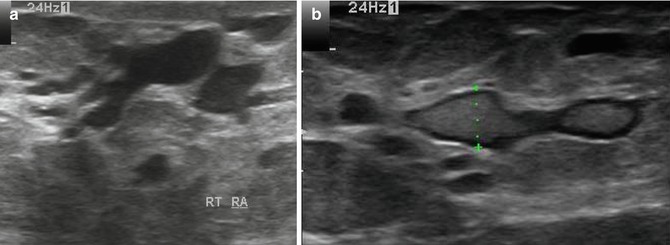
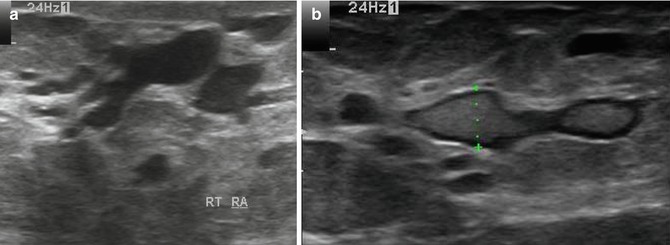
Fig. 22.3
(a) Ultrasound image shows multiple fluid-filled dilated ducts. (b) Dilated duct with mildly echogenic fluid due to inspissated secretions
When associated with inflammation, typically the inflammation is periareolar with localized edema and collection of pus. The infection is usually due to mixed aerobic and anaerobic organisms. A broad spectrum antibiotic like amoxycillin with clavulanic acid is effective.
Nipple discharge cytology in bilateral, multiple duct discharge that is milky or yellow is not useful and is not recommended. Reassurance is all that is required for such patients. Intervention like major duct excision or division is required only in unilateral, spontaneous discharge from single duct with copious discharge that is clear, pink, or bloody in color and with repeated bouts of inflammation.
Galactorrhoea
Copious, bilateral milky discharge in nonpregnant or lactating women is called galactorrhea. Intake of drugs like serotonin reuptake inhibitors, antipsychotics like riseperidone, opiates, methyldopa, H2 receptor antagonists like cimetidine, and proton pump inhibitors can cause milky nipple discharge. Endocrine causes like hypothyroidism and hyperprolactinemia also can cause milky nipple discharge. Serum prolactin levels of over 1,000 mu/L should prompt investigations for a possible pituitary adenoma. Hyperprolactinemia is characterized by galatorrhoea, amenorrhoea, and infertility. Galactorrhoea disappears after appropriate therapy. Cabergoline is preferred over bromocriptine because bromocriptine produces significant side effects on fetal outcomes in some women (Fig. 22.4).


Fig. 22.4
Dilated ducts fill with echogenic debris
Single Duct Discharge: Intraductal Papilloma
Unilateral serous, serosanguinous, or bloody nipple discharge from a single duct orifice is usually surgically significant. Intraductal papillomas are benign wart-like growths within the ducts and usually the cause for single duct discharge in over 90 % of women. A small proportion (10 %) may be due to ductal in situ carcinomas or invasive ductal carcinoma. Most intraductal papillomas are close to the nipple. A complete clinical examination should be performed in patients with single duct discharge. It is usually possible to identify the trigger point or zone which when pressed will elicit the jet of nipple discharge. Papillomas tend to secrete fluid into the ducts which distends the duct and results in nipple discharge. Papillomas are soft and friable, therefore they can fragment or partially infarct. This may actually result in bloody nipple discharge. Sometimes, the papilloma will obstruct the duct and continue to secrete fluid causing a secondary cyst formation or an intracystic papilloma.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







