CHAPTER 16 Supraclavicular block
Clinical anatomy
In the neck, the brachial plexus lies in the posterior triangle (Fig. 16.1), covered by the investing layer of deep cervical fascia, platysma, and skin. It is crossed by the supraclavicular nerves, the inferior belly of the omohyoid muscle, the external jugular vein, and the transverse cervical artery and vein. It emerges between the anterior scalene and middle scalene muscles; its upper part lies above the third part of the subclavian artery, while the lower trunk formed by the union of the eighth cervical and first thoracic nerve roots is placed behind the artery; the plexus next passes behind the clavicle.
Surface anatomy
Important landmarks for the supraclavicular block include the interscalene groove behind the posterior border of the sternocleidomastoid muscle, the clavicle, and the subclavian pulse (Fig. 16.2). The interscalene groove can be identified by placing a finger behind the sternocleidomastoid muscle and then rolling laterally. Maneuvers to help identify landmarks include asking the patient to flex their neck against resistance to identify the sternocleidomastoid muscle. Sniffing accentuates the scalene muscles. The groove can be followed toward the clavicle. The belly of the omohyoid muscle crosses the groove, and 1 cm above the clavicle the subclavian pulse is usually palpated. The external jugular vein crosses the interscalene groove and posterior border of the sternocleidomastoid muscle at the level of the cricoid cartilage. The needle insertion site is immediately posterior to the subclavian pulse.
Sonoanatomy
The ultrasound transducer should be held between the thumb, index and ring fingers of the non-dominant hand. Placing the little finger and ulnar aspect of the hand on the patient will stabilize the transducer. Firm even surface pressure with the ultrasound transducer usually produces the best images. Above the clavicle, the ultrasound transducer (38-mm linear array high frequency transducer) is oriented in a coronal oblique axis to the neck (Fig. 16.3). This is the transverse ultrasound transducer orientation. Such transverse imaging facilitates identification of nerves and associated relations. It also allows verification of circumferential spread of local anesthetic around nerves. A curvilinear transducer can also be used for this block. Perform a systematic anatomical survey from medial to lateral and superficial to deep.
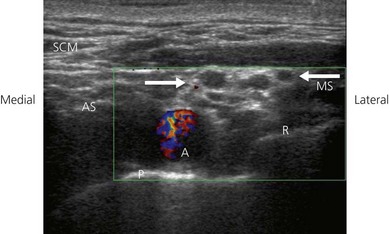
The supraclavicular ultrasound-guided technique focuses on the supraclavicular fossa, where the superior, middle, and inferior primary trunks divide into their anterior and posterior branches. The plexus runs superficially at this level, and high-frequency transducers are thus needed (10 MHz) to identify the relevant structures (Fig. 16.4). Technical difficulties are encountered in studying the supraclavicular region due to the presence of the supraclavicular depression, which complicates both manipulation of the ultrasound transducer and needle puncture. First locate the subclavian artery. Identify the hyperechoic first rib deep to the subclavian artery and its shadow beneath. Identify the pleura and air artifact beneath. This is different from the shadow beneath the first rib. The brachial plexus is found lateral and posterior to the subclavian artery. The subclavian artery and brachial plexus lie between the scalene muscles.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree