Chapter 63 Stroke and Intracerebral Hemorrhage
Stroke and intracerebral hemorrhage are significant causes of morbidity and mortality in children. In recent years, childhood stroke has become more commonly recognized. Because of the heterogeneous etiologies, risk factors, and presentations in children, the diagnosis, treatment, and management of stroke present many challenges compared with the adult population. Previous studies have found the incidence of pediatric stroke to be between 2.3 and 13 per 100,000 children per year.1–4 Boys have been observed to be at higher risk than girls, and children of African descent are at higher risk than white or Asian children.5 Peak incidence of stroke and intracerebral hemorrhage occurs during the first year of life except in the case of subarachnoid hemorrhage, which peaks in adolescence.5 Childhood stroke encompasses a wide spectrum of disease and can be categorized into three groups: arterial ischemic stroke, cerebral venous sinus thrombosis, and intracranial hemorrhage. The pediatric intensivist must be familiar with the various etiologies of childhood stroke and be facile in integrating a complete diagnostic and treatment approach to prevent further brain injury and minimize morbidity and mortality.
Arterial Ischemic Stroke
Pathophysiology
The pathophysiology of ischemic stroke is initiated when circulating blood supply to the brain is decreased or absent, resulting in the deprivation of necessary substrates for metabolism (see also Chapter 62). The brain does not have extensive glucose stores, which results in a fairly rapid pathologic cascade after the onset of ischemia.6 Brain tissue has limited capacity for anaerobic metabolism, which exacerbates substrate deprivation. The decrease in arterial blood supply is the result of thrombus formation, embolus, arterial stenosis, or in many cases a combination of these factors.
The extent and progression of ischemic injury is related to a multitude of factors (Box 63-1). Cerebral perfusion pressure plays a major role, and the maintenance of a steady and adequate cerebral perfusion pressure is critical to minimizing the extent of ischemia. The extent of collateral circulation in the area of affected brain and the duration of the ischemia influences outcome as well. Ischemia of shorter duration or slower onset is better tolerated by the brain, and regions with extensive collateral circulation are at less risk for infarction. Hypercoagulable states can increase the rate of progression and size of thrombus formation, and elevated temperature following brain injury has been associated with poorer outcomes in animal models and humans.7–10 Disturbances in serum glucose levels (hyperglycemia or hypoglycemia) can increase the extent of ischemic injury.11
Cerebral blood flow (CBF) is coupled to the cerebral metabolic rate, which changes with age in the immature brain. Infants have similar CBF rates compared with adults (50 to 60 mL/100 g brain tissue/min). CBF rises in children and peaks between the ages of 3 to 8 years at 80 mL/100 g/min.12 It then decreases to the adult level by mid to late adolescence. In response to ischemia, cerebral autoregulation mechanisms increase CBF by local vasodilation (in collateral vessels), and brain tissue responds by increasing the oxygen extraction rate.
Following a decrease in CBF, energy failure at the cellular level leads to a phase of neuronal hyperexcitability. The loss of membrane ion gradients and the failure of glutamate reuptake with widespread neuronal depolarization results in further increases in extracellular glutamate and excitotoxicity. Excitotoxicity results in a cascade of oxidative stress, failure of cellular systems, and ultimately cell death. The perfusion threshold below which infarction occurs has been reported to be 5 to 8 mL/100 g/min within the first few hours of onset.13,14 In regions of focal ischemia, the central area of lowest perfusion is defined as the ischemic core and is beyond therapeutic rescue when ischemia is of sufficient severity and duration to cause cell death. Surrounding the ischemic core is an area of decreased perfusion above the threshold of ion pump failure and irreversible damage but below the threshold of functional impairment, known as the ischemic penumbra, first described in experimental models.14 The ischemic penumbra varies with duration of the interruption of blood flow, and the threshold for infarction in the penumbra rises with time, which emphasizes the need for timely intervention to promote recovery. Interventions that promptly restore flow at the site of vascular occlusion and optimize reperfusion of the ischemic penumbra are currently the most effective therapies for stroke in adults.15
Epidemiology
The incidence of pediatric AIS has been estimated at two to three per 100,000 children per year in the United States, but it has been reported to be as high as 13 per 100,000 children in France.1,4,5,16
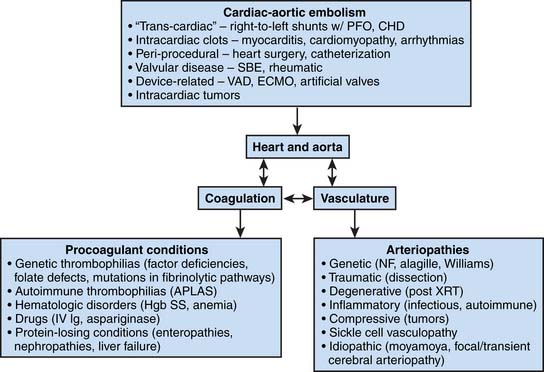
A classification system based on mechanism has been developed for adult AIS, but this system is not applicable for neonatal strokes or for the vast majority of childhood strokes. An alternative conceptual framework for classifying stroke in childhood begins by separating neonatal from childhood stroke, and then subdividing the causes into broad pathophysiologic groups: cardiac-aortic embolism, vascular disease, and coagulation disorders (Figure 63-1). About half of children with first-time stroke have conditions known to be associated with risk of stroke (symptomatic AIS), and about half are previously healthy children at the time of stroke presentation (cryptogenic stroke). After completion of a comprehensive risk factor evaluation, 80% to 90% of children are found to have at least one risk factor, and many children have multiple risk factors.18,19 Risk factors for neonatal stroke differ significantly from those for childhood stroke. For a detailed review of neonatal stroke, including a discussion of definitions and risk factors, the reader is referred to a recently published summary of a National Institute of Health workshop on this topic.18 The risk of recurrent AIS in children has been reported to be from 6% to 14%.19,20 In a study from the United Kingdom, moyamoya syndrome and low birth weight were found to be the most important predictors of recurrent pediatric stoke.19
Etiologies and Risk Factors
Sickle Cell Disease
Incidence of stroke in children with sickle cell disease (SCD) has been reported to be 200 times higher than in the general pediatric population.21 High blood flow velocity on transcranial Doppler (TCD), silent brain infarction, low hemoglobin, hypertension, and history of acute chest syndrome all have been identified as stroke risk factors in children with SCD.22 A familial predisposition to stroke in SCD also has been reported.23 Approximately 20% of patients will have silent brain infarcts on magnetic resonance imaging (MRI). Stroke in SCD is associated with the development of large vessel stenosis in the middle cerebral or distal internal carotid artery (moyamoya syndrome), the mechanism of which is unclear (also see Chapter 84).24
Moyamoya Disease and Syndrome
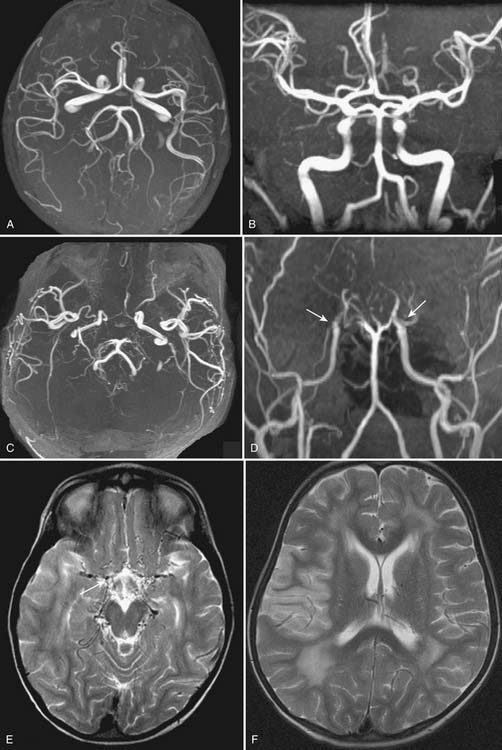
Moyamoya syndrome is a condition characterized by progressive stenosis of the distal intracranial internal carotid arteries and their proximal branches that predisposes patients to stroke. It was first described in 1957 in Japan. Moyamoya is a term in Japanese meaning “something hazy or a puff of smoke,” representing the characteristic finding on angiography (Figure 63-2).25,26 Patients with no known associated comorbidity are categorized as having moyamoya disease. The highest incidence has been reported in Japan at three cases per 100,000 children, and much lower rates have been reported in Europe and the United States (0.086/100,000).27,28 Moyamoya syndrome in children usually presents as ischemic stroke or transient ischemic attacks. Ischemic strokes can be repetitive and are commonly found in watershed territories. Presentations can vary from infrequent, intermittent attacks to a rapid and fulminant course.
Arterial Dissection
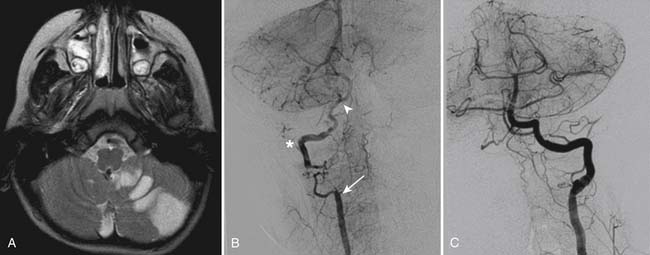
A spontaneous or traumatic tear in the intimal layer of an arterial vessel can lead to arterial occlusion and artery-to-artery embolism. Arterial dissection is a significant cause of pediatric stroke and has been reported to be the cause for 7.5% of ischemic strokes.29 Traumatic vertebral artery dissections in children are usually the result of sports injuries, and symptoms may appear quickly or can be delayed up to days (Figure 63-3). In many cases, the precipitating injury does not seem severe enough to result in vertebral artery dissection. Recurrence in cases of arterial dissection is highest in the first 4 to 6 weeks after the initial presentation, and thereafter it falls to less than 1% per year. Factors associated with recurrence are incompletely understood but may include predisposing conditions such as pro-thrombotic conditions, fibromuscular dysplasia, Marfan syndrome, autosomal-dominant polycystic kidney disease, coarctation of the aorta, and Ehlers-Danlos syndrome type IV.30
Congenital and Acquired Heart Disease
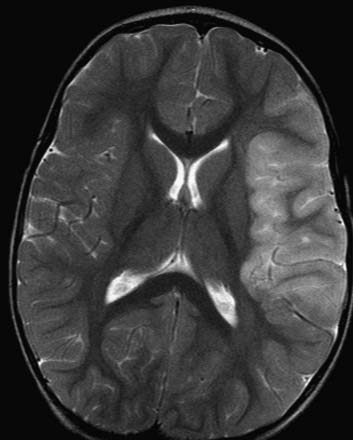
Among children with cardioembolic causes for stroke, those with complex congenital heart disease with right-to-left shunts are at greatest risk, but stroke has been observed in children with other heart defects. Children with uncorrected congenital heart disease are at highest risk, and emboli can arise at the atrial, ventricular, and arterial level. Prosthetic heart valves increase the risk for endocarditis and stroke. Patients with left-sided endocarditis have neurologic complications rates of 20% to 40%, with half of these events being strokes.31 Cardiac surgery and catheterization also can be complicated by thromboembolic stroke (Figure 63-4). Stroke secondary to cardiac arrhythmias or acute myocarditis is uncommon in children but has been reported. Cardiomyopathy and congestive heart failure place children at higher risk for stroke and are associated with muscular dystrophy, mitochondrial disorders, and other metabolic disorders.
Focal and “Transient” Cerebral Arteriopathy
Focal cerebral arteriopathy refers to a group of childhood cerebral arteriopathies of uncertain cause; they manifest most typically as arterial ischemic stroke in the middle cerebral artery territory and are associated with findings on vascular imaging of focal stenosis or occlusion in the proximal middle cerebral artery.32 The natural history is variable, with spontaneous remission and normalization of the vessel in some children, stable chronic partial occlusion in others, and progressive stenosis involving other areas of the circle of Willis in other children. In some children there is a period of progression over months to a year and eventual stabilization, often referred to as “transient cerebral arteriopathy.”33 This pattern is typical of that seen in children with stroke and vasculopathy attributed to prior varicella (postvaricella vasculopathy),33 and it is among the childhood arteriopathies associated with significant risk of recurrence.3
Vasculitis
Vasculitis of intracranial vessels in children can be due various etiologies and affect a wide variety of vessel sizes (Box 63-2). Cerebral vasculitis should be considered in children with stroke and fever, elevated markers of inflammation (c-reactive protein or sedimentation rate), skin findings, or renal dysfunction. Primary vasculitis of the intracranial vessels in children is rare and usually presents with headache and altered mental status but without elevation in the sedimentation rate. Intracranial infections can cause a secondary vasculitis leading to AIS. Bacterial meningitis, mycotic infections, and tuberculous meningitis all have been associated with stroke. Lyme disease and rickettsial infections can involve intracranial vessels, leading to stroke. Varicella infections have been reported to cause a cerebral vasculopathy in children.34 Takayasu’s arteritis should be considered in older children, especially girls of Asian descent. Patients with systemic lupus erythematosus are at higher risk for stroke. Direct intracranial vasculitis in persons with systemic lupus erythematosus is rare, but stroke also can occur as a result of embolism from Libman-Sacks endocarditis and a hypercoagulable state (antiphospholipid antibodies) (also see Chapter 98).35
Hypercoagulable States
Various pro-thrombotic states are common in children with stroke, and often are combined with other major stroke risk factors such as congenital heart disease (Box 63-3).36 Elevated lipoprotein a and deficiencies in antithrombin III, protein C, and protein S have been identified in children with AIS. Antiphospholipid antibody syndrome has been associated with recurrent fetal loss, thrombocytopenia, and cardiac valve disturbances, but its association with increased AIS in children is unclear.37 Homocystinuria is an uncommon condition but can cause arterial ischemic stroke. Clinical manifestations include marfanoid features, mental retardation, seizures, and arteriosclerotic vascular disease. The spectrum of microangiopathic hemolytic anemias including hemolytic-uremic syndrome and thrombotic thrombocytopenia purpura can present with various neurologic manifestations including ischemic infarction. In adolescent girls both pregnancy and use of oral contraceptives must be considered risks factors for AIS.38 The importance of pro-thrombotic risk factors is further evidenced by the observation that certain pro-thrombotic conditions are associated with higher recurrence risk.20
Metabolic Disorders and Toxins
Metabolic disorders are rare causes of stroke-like syndromes or lesions that are not the result of vascular-occlusive infarcts but, for the purposes of this chapter, will be discussed here. Chief among these disorders is MELAS (mitochondrial myopathy, encephalopathy, lactic acidosis, and stroke).39 The exact mechanism of ischemia in MELAS is likely multifactorial, including direct cytotoxicity from mitochondrial failure and glutamate toxicity, as well as loss of normal coupling of cellular metabolism and CBF.40 Illicit drug use has been associated with stroke. Cocaine use has been associated with both ischemic and hemorrhagic stroke, and there have been reports of stroke in young adults using amphetamines and ecstasy (3,4-methylenedioxymethamphetamine).41–43
Clinical Manifestations
AIS in infants and children can be difficult to correctly diagnose. Stroke typically is not high on the practitioner’s differential diagnosis in the pediatric population, and the presenting symptoms are attributed to more common conditions such as a viral syndrome, migraine, or oppositional behavior. Compared with adults, children may not articulate their symptoms well. Infants usually fail to display localized deficits and typically present with seizures or altered mental status. Many stroke “mimics” exist in childhood that require advance imaging for accurate diagnosis, including migraines, demyelinating disorders, tumors, hypertensive encephalopathy, psychogenic, postictal paralysis, infections, and metabolic disorders.44 These factors can lead to delays in presentation as well as delay in diagnosis.45
AIS usually presents with acute neurologic deficits in an arterial distribution and typically conforms to a pattern of ischemia in either the anterior (carotid) or posterior (vertebrobasilar) circulations. Deficits associated with each are related to the regions of brain supplied by the affected artery or arteries. The anterior circulation includes the internal carotid, anterior cerebral, and middle cerebral arteries. Ischemia in anterior circulation produces unilateral motor and sensory deficits.46 The location of the lesions can influence presentation. Typically cortical infarcts will affect both motor and sensory function in the face and upper extremity more than in the lower extremity. Subcortical infarcts will produce the same density deficits in the face and upper and lower extremities. Many patients will have visual field cuts with a gaze preference. If the stroke occurs in the dominant hemisphere, patients can present with aphasia. Extinction and neglect are seen when the infarction occurs in the nondominant hemisphere. The posterior circulation includes the vertebrobasilar arteries that supply the brainstem, cerebellum, and the occipital lobe.46 Cerebellar strokes closely resemble acute cerebellitis, typically including severe headache, lethargy, vomiting, ataxic gait, unilateral limb ataxia, and dysarthria.47,48 Unilateral brainstem deficits include pure motor deficits without cortical symptoms, oculomotor deficits, diplopia, vertigo, tongue deviation, or dysarthria/dysphagia.49 Infarcts in the distribution of the posterior cerebral artery present typically with visual field deficits and gaze preference. Seizures herald the onset of stroke in 10% to 20% of childhood-onset AIS and in the vast majority of neonatal cases of AIS.
Imaging and Laboratory Evaluation
The goals of initial investigation are to verify the occurrence of AIS and the location to determine the likely causative stroke mechanisms so a specific treatment plan can be initiated.10 If AIS is suspected, strict attention to maintenance of adequate airway, breathing, and circulation and close monitoring of neurologic status should be performed throughout the acute evaluation process.
Neuroimaging typically starts with a head computerized tomography scan (CT) because it is widely available and can quickly demonstrate hemorrhage as the cause of symptoms. The major disadvantages of CT, in addition to exposure to ionizing radiation, are that it is insensitive and nonspecific and does not provide information about vascular disease. Ischemic changes on CT typically are not visible until 12 to 24 hours after onset and are indistinguishable from lesions that mimic stroke such as tumor and demyelinating disease. MRI with diffusion weighting is far superior for the diagnosis of AIS and the differentiation of stroke from other diagnoses such as acute disseminated encephalomyelitis or methotrexate toxicity.50 Moreover, vascular imaging can be obtained readily with the initial diagnostic brain imaging using MRI, and it should be obtained for both the head and the neck in all children suspected of having a first ischemic stroke (see Figure 63-3). When a metabolic stroke-like syndrome is suspected, such as MELAS, magnetic resonance spectroscopy may be helpful. If MRI is not available, vascular imaging can be achieved with CT angiogram.51 Diagnostic imaging can be challenging for the pediatric patient, and care must be taken not to compromise oxygenation, ventilation, and perfusion to at-risk tissues with sedation or general anesthetics. Careful planning and coordination of diagnostic imaging is necessary to obtain optimal imaging in a timely and safe manner. This coordination is best accomplished through direct consultation and dialogue involving the primary team caring for the patient, the sedation team, and the radiology technicians and physicians responsible for specifying and executing the imaging protocol (also see Chapter 56).
Laboratory evaluation in the early screening stage should include a complete blood cell count, comprehensive metabolic panel, and coagulation profile (Box 63-4). If AIS is confirmed, a thrombophilia workup should be performed and consultation with a hematologist should be considered. It is critical that blood samples be taken for key tests prior to the initiation of anticoagulation therapy (see Box 63-4). If stroke symptoms are associated with an acute febrile illness, a lumbar puncture should be considered as well as serologies for other infectious etiologies (e.g., mycoplasma infection and Lyme disease). Lumbar puncture may need to be delayed if intracranial hypertension as a result of stroke and peri-infarct edema are suspected, particularly for patients with large strokes. When an embolic etiology of AIS is suspected, urgent cardiac evaluation is warranted, including an echocardiogram with a bubble study and an electrocardiogram (ECG). Although uncommon, AIS has been reported in children with cardiac arrhythmia.52
Box 63–4 Laboratory Evaluation of Suspected Stroke in Infants and Children
Screening Studies on Admission for Children with Acute Neurologic Deficit
Supplementary Studies for Children with Atypical Infarcts or Suspected Metabolic Stroke
Treatment
Regardless of the etiology of AIS, management should focus on optimizing perfusion and oxygenation, neuroprotection (minimizing expansion of the ischemic core and secondary injury and rescuing the penumbra), rehabilitation, and prevention of recurrence (Box 63-5). Specific therapies should be tailored based on the stroke mechanism. Reviews of existing evidence and summaries of evidence-based and consensus-based management guidelines have been published recently.10,53