187 Soft Tissue Injury
• Retained foreign bodies (FBs) can cause pain, infection, delayed healing, nerve and tendon injury, masses, and functional impairment.
• Specific injuries, such as those caused by broken glass or surfaces with gravel and stepping on objects, are particularly prone to retained FBs.
• Wounds should be explored for FBs with adequate anesthesia and lighting in a bloodless field.
• Plain radiographs are useful in evaluating for radiopaque FBs and should be ordered commonly.
• Plain films may miss nonradiopaque FBs such as wood, plastic, and vegetative matter. They may also miss radiopaque FBs that are tiny, obscured by bone, or in areas that are difficult to obtain quality images, such as the face or sole of the foot.
• Ultrasound scans and portable fluoroscopic studies may aid in localization and removal of FBs. Computed tomography and magnetic resonance imaging are rarely indicated.
• Neither exploration nor imaging alone can rule out an FB. The two should be used in combination in most instances. No wound is too small or superficial to harbor an FB.
• Careful discharge instructions are crucial and can minimize the morbidity and medicolegal risk associated with retained FBs. Patients should be informed that it is impossible to detect all FBs, be told what to expect in the event of a missed FB, and be given appropriate referral should these circumstances arise.
• Direct exploration of wounds plus visualization of tendons placed through a full range of motion is necessary for proper evaluation of tendon injuries.
• A detailed neurovascular examination is required to identify possible nerve lacerations.
• Most tendon and nerve lacerations can be repaired on an outpatient basis. Ensuring appropriate and timely follow-up is important.
Retained Foreign Bodies
Epidemiology
Open wounds are frequent reasons for emergency department (ED) visits. The true incidence of foreign bodies (FBs) in wounds is unknown, but with more than 5 million estimated lacerations repaired in EDs in 2007,1 wound FBs surely occur in such a significant number that all emergency physicians (EPs) will encounter them. Wound FBs are frequently missed on initial evaluation. Seventy-five of 200 FBs encountered in a hand clinic were missed by the initial physician.2 Furthermore, missed FBs pose high medicolegal risk for EPs, with one report listing it to be among the top three causes of litigation after wound care.3
Most wound FBs are wood, glass, or metal. The upper extremity is the most common location (58%), followed by the lower extremity (36%). The head and neck (4%) and the trunk (1%) are far less common. Most cases will be seen on the day of injury (75%), but some (8.7%) will initially be evaluated weeks, months, or years later.4
Pathophysiology
A retained FB can lay harmlessly dormant for a long period and then can react with surrounding tissue. When a tissue reaction occurs, several sequelae are possible. An infection may occur. The patient’s body may dissolve, extrude, or encapsulate the FB and form a granuloma, and subsequent rupture of the granuloma from minor trauma can cause delayed infection. The extent of tissue reaction depends primarily on the chemical composition of the material. Inert material causes less tissue inflammation, whereas reactive material can cause intense tissue reactions (Box 187.1) and rarely even allergic reactions. Even when an FB does not cause a tissue reaction, it can have other effects. The FB may cause local compression on neighboring structures such as nerves, tendons, joints, or vessels, thereby causing pain or structural damage. Local migration or, more rarely, distant embolization can also occur.
Presenting Signs and Symptoms
The classic example of a wound FB is a patient who sees or knows that foreign material is present in a wound, such as a splinter, glass in the sole of the foot that the patient cannot remove, or an obviously soiled wound. Alternatively, it is also common for a patient to have a wound and not to know that foreign material is present. The chief complaint of such patients is simply that they have a wound. Certain mechanisms are highly suggestive of wound FBs (Box 187.2).5–8 Some unique wound FBs include shrapnel, fishhooks, bullets and BBs, cactus spines, and marine material (Table 187.1). Some patients may exhibit sequelae of a retained FB from the near or distant past, such as a mass, persistent pain, infection, functional impairment as a result of nerve or tendon injury, arthritis, vascular injury, or embolization.
Box 187.2 Scenarios Suggestive of Foreign Bodies in Wounds
History of punching through a window
Motor vehicle collision wounds from glass
Wounds on the sole of the foot
Objects that fragment while in one’s hand
Pain at a site of intravenous drug use
Foot laceration while walking in a stream
Wound infection, especially if persistent
Perioral wounds in the presence of broken teeth
Table 187.1 Treatment—Special Circumstances
| TYPE OF FOREIGN BODY | TIPS AND COMMENTS |
|---|---|
| Fishhooks | Anesthetize the area, advance the tip of the fishhook through the skin, cut the barb, and withdraw the hook. |
| Splinters | Do not pull long splinters out because they tend to fragment. Instead, excise along the long axis or elliptically. |
| Needle tips | Removal may require excision of a block of tissue. |
| Shrapnel | When extensive, emergency department removal of all shrapnel may not be feasible or indicated. Remove as much as reasonably possible, with a focus on dangerous locations, and refer the patient for further treatment. |
| Bullets, BBs | These items are often left in situ, but objects larger than 4.5 mm in diameter tend to track skin and clothing into wounds, so visualize, irrigate, and leave open when possible. Remove these objects only if they are easily accessible or in the pleura (risk for lead poisoning). |
| Cactus spines | Use fine-tipped forceps or glue to remove them. |
| Marine envenomations | Treatment (hot water immersion, vinegar, shaving) depends on the type of spine or nematocyst. |
| Traumatic tattooing | Sources include pencils and blacktop. Débride with a scrub brush. Management is difficult. Consider referral to dermatology or plastic surgery for dermabrasion or laser treatment. |
Neither the presence nor the absence of FB sensation on the part of the patient can confidently rule in or exclude an FB. In a series of 164 wounds caused by glass, 41% that contained glass caused an FB sensation, with a positive predictive value of 31% and a negative predictive value of 89%.5
Differential Diagnosis and Medical Decision Making
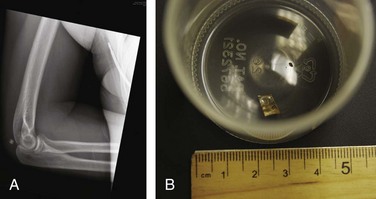
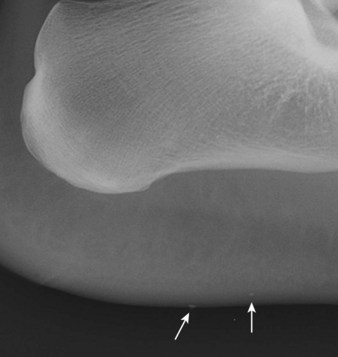
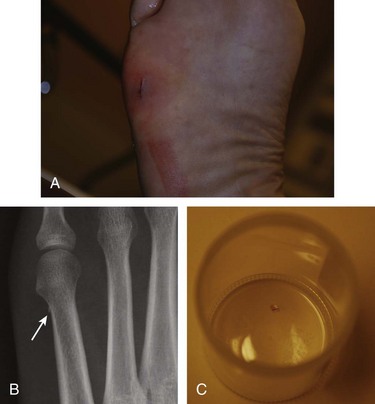
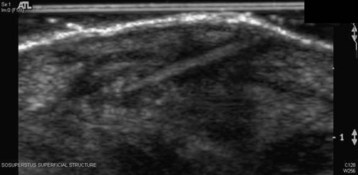
No wound is too small or superficial to harbor an FB, and thus the possibility of an FB must be considered for all wounds. Most wound FBs are initially diagnosed by physical examination (78%), but many are diagnosed primarily by imaging studies (22%).4 Exploration alone is insufficient to rule out an FB,5,9,10 even when the entire wound is thought to be visualized. Therefore, imaging should be used liberally. Selection of the proper imaging modalities requires knowledge of the radiographic properties of the material (Box 187.3 and Figs. 187.1 through 187.3). Even when a suspected FB is not radiopaque, plain film radiographs with an underpenetrated soft tissue technique could be considered because other useful soft tissue or bony findings and reactions may be present. Furthermore, failure to order radiographs has been associated with unsuccessful legal defense in cases of retained FBs.11 Ultrasound scanning is particularly useful for nonradiopaque FBs (Fig. 187.4).7 Low-power portable fluoroscopy, when available, is useful to aid in removal of radiopaque FBs. Computed tomography and magnetic resonance imaging are rarely indicated. However, computed tomography may be useful for ocular or periorbital FBs (Table 187.2).12,13
Table 187.2 Features of Available Imaging Techniques
| IMAGING MODALITY | POSITIVE FEATURES | NEGATIVE FEATURES |
|---|---|---|
| Radiography | ||
| Ultrasound | ||
| Portable fluoroscopy |