CHAPTER 80 SOFT TISSUE INFECTIONS
Soft tissue infections occur frequently and account for approximately 48.3 in 1000 outpatient visits. The severity of these infections varies from trivial to life-threatening.
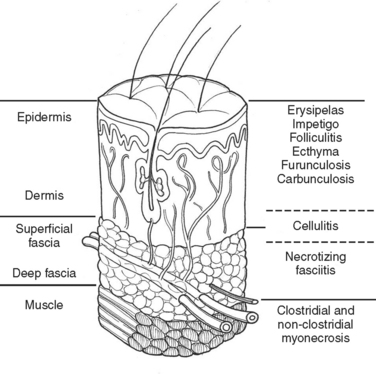
Much of our knowledge regarding the treatment of soft tissue infection has been based on the experience gained during military conflicts. For instance, hospital gangrene was described first by Joseph Jones, a Confederate surgeon during the Civil War. The treatment of battlefield infections has influenced civilian practice. This review will begin with a description of the anatomically more superficial infections and progress to the deeper, life-threatening infections (Figure 1).
DEEP INFECTION
In the medical literature, deep structure infection has masqueraded under a variety of pseudonyms. The term “necrotizing soft tissue infection” (NSTI)is used here. Table 1 lists a variety of terms that may appear in the medical literature to describe this infective process.
Table 1 Terms Used to Describe NSTI
| Meleney’s synergistic gangrene | Hospital gangrene |
| Streptococcal gangrene | Fournier’s gangrene |
| Gas gangrene | Acute dermal gangrene |
| Suppurativa fasciitis | Necrotizing erysipelas |
| Phagedena | Phagedena gangrenosum |
| “Flesh-eating disease” | Necrotizing fasciitis |
| Clostridial cellulitis |
CLINICAL PRESENTATION
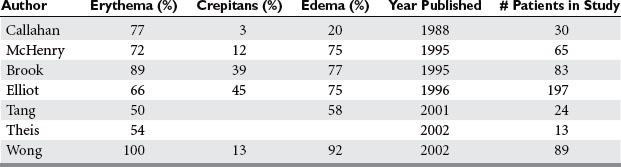
Signs and symptoms of NSTI can be quite nonspecific (Table 2). Pain, erythema, and swelling of the affected area are most frequently present. This same constellation of symptoms may be seen in pathologic processes that have a much more benign course and respond effectively to antibiotic therapy alone. “Hard signs” of necrotizing infection include tense erythema, bullae, skin discoloration, and crepitus, pain out of proportion to examination, or anesthesia of the affected area. Unfortunately, many of these are late signs and indicate that the infective process is well established or they occur only in a small percentage of patients.
Signs of systemic toxicity may also be present. These may include pyrexia, tachycardia, hypotension, and organ dysfunction. The progression of symptoms may be rapid over the course of hours to days or more indolent over the course of days to weeks. The rate of progression of symptoms may be ameliorated by partial treatment. Some suggest classifying the disease by its clinical course. Fulminant disease presents in patients with acute onset and rapid progression over the course of hours with shock. Acute disease presents with large surface area involvement and over the course of days. Subacute disease presents for weeks and is usually localized. Differentiating this process from cellulitis or simple abscess can be a challenge. Clinically, failure to improve with appropriate antibiotics or worsening systemic toxicity portends this diagnosis (Table 3).
| Rapid progression: |
| Slower progression: |
< div class='tao-gold-member'> Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|