
Shortness of Breath
C. Keith Stone
Shortness of breath refers to difficult, labored, or uncomfortable breathing. Shortness of breath results when ventilatory demand exceeds respiratory function. A mismatch between supply and demand of oxygen and failure of CO2 elimination is the mechanism that produces the sensation of shortness of breath. Table 8.1 details the most frequently encountered causes and the most common etiologies of acute shortness of breath seen in the emergency department (ED).
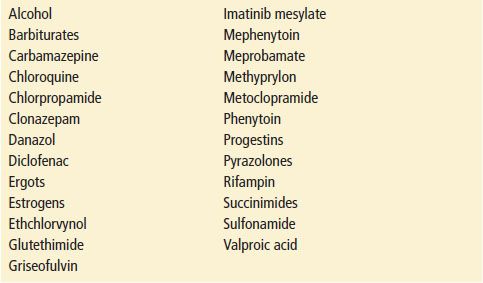
TABLE 8.1
Causes of Acute Shortness of Breath
CLINICAL PRESENTATION
Patients commonly present to the ED complaining of shortness of breath. The clinical evaluation is guided by the history—is the shortness of breath new onset without any previous determination of the underlying cause or is the patient experiencing an acute exacerbation of a chronic respiratory, cardiovascular, or neuromuscular condition (1)? Once the initial assessment ensures that the airway is patent and oxygenation is adequate, a thorough history should be obtained. The duration and onset of the sensation of shortness of breath; associated chest pain or palpitations; precipitating factors such as exertion, exercise, or anxiety; associated paresthesias of the mouth and fingers; the number of pillows the patient uses to sleep; concomitant coughing or sputum production; exercise tolerance; tobacco use; recreational drug use; and occupational history are several important factors that can help narrow the differential diagnosis. Past medical history of asthma, chronic obstructive pulmonary disease (COPD), congestive heart failure (CHF), coronary artery disease, and valvular heart problems should be sought. Paroxysmal nocturnal dyspnea (PND), breathlessness that occurs while sleeping, is usually associated with left ventricular failure. Orthopnea, the presence of shortness of breath in the recumbent position, is also associated with left ventricular failure but can be associated with COPD.
On physical examination, the patient’s vital signs, mental status, body position, use of accessory muscles, conjunctival and mucous membrane color, skin and nail bed color, upper airway examination, neurologic examination, cardiovascular and pulmonary examinations may give valuable clues to the etiology.
DIFFERENTIAL DIAGNOSIS
Anaphylaxis
Anaphylaxis is a severe allergic reaction involving one or more body systems that produces signs and symptoms such as hives, flushing, pruritus, angioedema, stridor, shortness of breath, bronchospasm, tachycardia, and hypotension. Death from anaphylaxis usually results from respiratory obstruction or cardiovascular collapse. Symptoms typically occur within 2 minutes of exposure to the triggering antigen but occasionally may occur as late as 2 hours (2). See Chapter 175 for further discussion.
Upper Airway Obstruction
Obstruction of the upper airway may be the consequence of foreign body aspiration, epiglottitis, croup, angioedema, peritonsillar or retropharyngeal abscess, or neuromuscular dysfunction. The nature of the presenting picture depends on the site and degree of the obstruction as well as the underlying cause. Cough, stridor, shortness of breath, aphonia, or hoarseness may be present. These conditions may not cause complete airway obstruction, but rapid deterioration is possible in these patients, and the emergency physician must be ready to provide immediate airway intervention. Alternative techniques to conventional direct laryngoscopy may be necessary; these include fiberoptic-guided intubation/video-assisted devices, bougie-assisted endotracheal intubation, blind nasotracheal intubation, lighted or optical stylets, flexible or rigid fiberoptic scopes, supraglottic airway devices (LMA, intubating LMA, PLMA), retrograde intubation, percutaneous transtracheal jet ventilation, and surgical airways (3). See Chapter 1 for further discussion.
Pulmonary Embolism
Pulmonary embolism (PE) is an obstruction of the pulmonary artery or one of its branches by an embolus, usually a blood clot derived from the deep venous system of the leg or pelvic veins. The diagnosis of PE is often subtle and may be difficult to make. The actual incidence of PE in the United States is unknown, but it is estimated to be greater than 650,000 cases annually and estimates are that the diagnosis is missed more than 400,000 times each year (4).
The classic findings of chest pain, shortness of breath, and hemoptysis are found in fewer than 20% of patients with a PE (4). Common complaints in addition to the classic symptoms include malaise, weakness, extremity discomfort, dizziness, or syncope (4). Clinical suspicion plays a key role in the decision to pursue an evaluation for acute PE. Patients at high risk include those who have had a previous PE or deep vein thrombosis (DVT), surgery within the last 3 months, travel more than 4 hours in the past month, trauma to lower extremity and pelvis during the past 3 months, malignancy, cardiopulmonary disease, and women during pregnancy or in the postpartum period (4).
A ventilation–perfusion scan, spiral computed tomography scan, and pulmonary angiogram, used in conjunction with the clinical pretest probability, D-dimer assay, and duplex Doppler evaluation of the lower extremities, will help the physician determine the likelihood of PE and the necessity of anticoagulation and admission. See Chapter 79 for further discussion.
Myocardial Ischemia
Patients with myocardial ischemia classically present with chest pain. However, a significant number of patients present with symptoms other than chest pain, termed anginal equivalents.
Shortness of breath either new onset or associated with exertion, is the most common anginal equivalent symptom, particularly in the geriatric patient (5). Patients with known coronary artery disease or those with significant risk factors for coronary artery disease who present to the ED with shortness of breath in the absence of chest pain should be evaluated for myocardial ischemia. See Chapter 82 for further discussion on the evaluation of coronary syndromes.
Congestive Heart Failure
CHF is a complex clinical syndrome resulting from either a structural or functional disorder of the heart that restricts the ventricular filling or the ejection of blood (6). Acute precipitating factors of CHF include increased sodium intake, noncompliance with medications, acute myocardial infarction, dysrhythmia, or anemia. The most common causes of CHF are coronary artery disease and hypertension, valvular heart disease, and cardiomyopathy.
Pertinent information obtained on history includes the presence of dyspnea, orthopnea or PND, peripheral edema, exercise intolerance, and fatigue. The physical examination may reveal jugular venous distention, rales, cardiac S3 gallop, hepatojugular reflux, ascites, and peripheral edema (6). Pulmonary edema may also lead to bronchospasm and wheezing, often termed cardiac asthma. Chest radiography may reveal cardiomegaly, pulmonary vascular redistribution, Kerley B lines, pleural effusion, and peribronchial cuffing. The measurement of B-type natriuretic peptide (BNP) has become a useful tool for the diagnosis of CHF in patients presenting to the ED with acute shortness of breath. BNP is synthesized as preproBNP in the cardiac ventricles and is released as a result of left ventricular wall stress (7). See Chapter 83 for further discussion.
Chronic Obstructive Pulmonary Disease
Although COPD is a chronic disorder, acute exacerbations of diminished respiratory function often bring patients to the ED. Exacerbations are usually caused by a worsening of airflow obstruction due to increased bronchospasm, increased sputum production from superimposed respiratory infection, environmental irritants (such as tobacco smoke), or cardiovascular deterioration. The patient may present with progressive shortness of breath, increased sputum production, and audible wheezing. Hypoxemia, tachypnea, cyanosis, and agitation may be seen. Signs of hypercarbia such as confusion, stupor, inadequate respiratory effort, or apnea may be seen and indicate severe compromise with impaired gas exchange. Findings on physical examination may include a barrel chest, pursed lips breathing, cyanosis, tripoding, and use of accessory muscles (8). Auscultation may reveal a combination of diminished breath sounds, a prolonged expiratory phase, wheezes, or rales (8). The chest radiograph may reveal an increased anterior–posterior diameter, flattened diaphragms, hyperinflated lungs, attenuation of the peripheral lung markings, and, in cases of superimposed infection, an infiltrate. See Chapter 77 for further discussion.
Asthma
Asthma is a chronic inflammatory condition resulting from bronchial hyperresponsiveness and airway obstruction leading to the clinical manifestations of recurrent episodes of wheezing, chest tightness, shortness of breath, and cough (9). The physical examination may reveal an increased AP diameter of the chest due to air trapping, tachypnea, wheezing, and mild-to-severe respiratory distress. Auscultation may be misleading in the case of severe obstruction; wheezing may be absent, as bronchial airflow is diminished to such an extent that no sound is audible. Chest radiographs may be normal, demonstrate a pneumothorax (PTX) or pneumomediastinum or, in the case of a precipitating infection, reveal an infiltrate. See Chapter 76 for further discussion.
Pneumonia
Pneumonia classically presents as an acute febrile illness with cough and purulent sputum production. Pneumonia should be suspected in patients with newly acquired lower respiratory symptoms (cough, sputum production, or shortness of breath), especially if these symptoms are accompanied by fever, altered breath sounds to include bronchial breath sounds, egophony, or rales.
Classification of pneumonia is based on the environmental contact where the infection was acquired. This classification can then be used to guide the clinician to the likely offending agent and choose the appropriate treatment (10). For ED patients, pneumonia is classified as either community-acquired or healthcare-associated pneumonia (HCAP). Streptococcus pneumoniae remains the most common etiology of community-acquired pneumonia (10). HCAP is typically caused by Pseudomonas aeruginosa, Klebsiella pneumoniae, Legionella, and methicillin-resistant Staphylococcus aureus (10). Immunosuppressed patients may present with staphylococcal pneumonia or pneumonia caused by opportunistic organisms such as Pneumocystis carinii, mycobacteria, or fungal organisms.
A chest radiograph may demonstrate lobar consolidation, as in bacterial pneumonia; patchy infiltrates, suggesting staphylococcal pneumonia, Haemophilus influenzae, or gram-negative pneumonia; interstitial infiltrates, suggesting Mycoplasma, Legionella, or Pneumocystis; or cavitary lesions, as in tuberculosis. However, there is considerable clinical overlap among these entities. Early recognition is important, so that appropriate empiric antibiotic treatment can be administered promptly. See Chapter 74 for further discussion.
Pneumothorax
PTX, or air in the pleural cavity, can occur spontaneously or as the result of trauma (see Chapter 31). Spontaneous PTX typically occurs in tall, thin, young males, and smoking greatly increases the likelihood (11). The cause of the spontaneous PTX is the rupture of a subpleural bleb or bullae, which is usually apical in location in 90% of cases (11). Spontaneous PTX also may be seen in patients with asthma, COPD, and tuberculosis and in AIDS patients with P. carinii pneumonia. Traumatic PTX results from blunt or penetrating trauma to the chest. Concomitant hemothorax, pulmonary contusion, and bronchial rupture may be present.
Patients may present to the ED in obvious respiratory distress or may complain of shortness of breath and pleuritic chest pain. Auscultation may reveal unilateral diminution of the breath sounds associated with increased tympany on percussion. Subcutaneous emphysema also may be present. Signs of imminent cardiovascular collapse such as hypotension, mediastinal shift, and the aforementioned findings may herald a tension PTX, prompting swift needle chest decompression prior to any further examination or diagnostic studies. Chest radiography may reveal an obvious PTX or may only show subtle findings. In the supine patient, the only sign of a PTX may be an abnormally prominent costophrenic angle on the AP or PA view. Ultrasonography at the bedside is a sensitive and specific imaging modality for the diagnosis of PTX. The anterior, lateral, and posterior lung should be scanned from the apex to the base with the patient in either supine or sitting position. If the scan reveals the lung sliding effectively, there is no PTX with a negative predictive value of 100% (11).
Observation is indicated in a patient with a small PTX if there is no significant dyspnea. Patients, who meet this criterion, may be observed in ED for 3 to 6 hours on oxygen. If the PTX does not progress on chest radiograph at the end of the observation period, they may be discharged home with close follow-up within 24 hours (11). Patients with a large PTX, a small PTX but with significant dyspnea, or those that fail observation should undergo invasive management with either aspiration of the pleural space or small bore chest tube placement.
DIAGNOSTIC APPROACH
The most important initial step in the management of shortness of breath is to secure the airway and ensure oxygenation and circulation. The physician should then perform a rapid, complete history and physical examination to elucidate the cause of the shortness of breath and formulate a diagnostic plan if the etiology is not readily identified (12).
Pulse oximetry is an easy, noninvasive monitoring technique that allows low-cost, continuous, reliable measurements of oxygen saturation (12). Every person who presents to the ED complaining of shortness of breath should have his or her oxygen saturation measured. Pulse oximetry may be inaccurate in reflecting oxygen saturation in the presence of high carboxyhemoglobin levels, methemoglobinemia, and low-perfusion states (12), and it does not relay any information about PCO2.
Arterial blood gas measurement may be necessary in evaluating patients who present with shortness of breath. Blood gases demonstrate the severity of gas exchange impairment and are useful as diagnostic tools as well as for establishing a baseline for monitoring therapy. The physician should use discretion, however, when obtaining blood gases. In cases of mild shortness of breath with a normal oxygen saturation on room air, blood gases are not needed.
The chest radiograph is a valuable diagnostic tool in elucidating the cause of shortness of breath and should be obtained in most all cases. Diagnostic radiographic findings can be expected in certain entities, such as pneumonia, PE, and PTX. However, the chest radiograph may be entirely normal, even when significant illness is manifested by shortness of breath. Special views of the chest may be helpful in certain circumstances. The lateral decubitus view may confirm the presence of a pleural effusion. Inspiratory–expiratory or positional films may indicate a bronchial foreign body.
The measurement of BNP can play an important role in the diagnosis of undifferentiated dyspnea. A BNP of 100 pg/dL or greater is consistent with the diagnosis of CHF with a sensitivity of 90%, specificity of 76%, and an accuracy of 81% for differentiating CHF from other causes of dyspnea (7). In addition, BNP has been shown to be useful to predict outcomes for CHF patients to include hospital readmission, and mortality (7). Other diagnostic studies may be helpful when evaluating a patient with shortness of breath. An electrocardiogram (ECG) can show abnormalities of heart rate and rhythm or evidence of ischemia, injury, or infarction. An ECG may also be helpful in evaluating patients with a suspected pulmonary embolus, although suggestive changes are present in only a minority of patients. Anemia is an important cause of shortness of breath, and a check of the patient’s hemoglobin or hematocrit may be useful as part of the workup. Rarely, bedside laryngoscopy or bronchoscopy may provide a definitive diagnosis, especially in the case of upper airway obstruction or suspected foreign body.
CRITICAL INTERVENTIONS
• If the clinical condition warrants consideration of mechanical ventilation, the physician should determine whether the patient is a candidate for noninvasive positive pressure ventilation (NIV) (13). Evidence-based guidelines recommend the use of NIV in patients with severe COPD exacerbations with a pH <7.35 and relative hypercarbia, respiratory failure caused by cardiogenic pulmonary edema with no evidence of shock, and acute coronary syndrome requiring urgent coronary revascularization (13). Contraindications include acute lung injury, cardiorespiratory arrest, severe encephalopathy, severe upper gastrointestinal bleeding, hemodynamic instability, unstable cardiac rhythms, facial or neurologic surgery, facial trauma or deformity, upper airway obstruction, the inability to cooperate or protect the airway, the inability to clear secretions, and patients who are at high risk for aspiration (13). Endotracheal intubation should be performed if any of these contraindications are present.
• In patients with anaphylaxis, a patent airway must be established and maintained. Immediate treatment with epinephrine (1:1,000 dilution in a dose of 0.3–0.5 mL intramuscularly) repeated every 5 to 15 min as needed (2). Intravenous epinephrine is reserved for patients in shock. The typical dose is 5- to 15-μg/min continuous infusion titrated to effect (14). Additional treatment includes antihistamines, to block both H1 and H2 receptors, and steroids. Observation after treatment is needed owing to a delayed, second phase of reactivity that may occur; a period of 24 h of observation in a monitored setting is prudent.
• Once a preliminary diagnosis is made, treatment should be appropriately tailored to alleviate the patient’s shortness of breath. Specific therapies can be found in the chapters devoted to each of the differential diagnoses.









