CHAPTER 94 SEPSIS, SEPTIC SHOCK, AND ITS TREATMENT
sepsis and septic shock, especially when associated with single or multiple organ dysfunction, are important causes of morbidity and mortality in trauma patients. Thus, an organized approach directed at preventing infectious complications as well as a strategy ensuring early diagnosis and treatment of infections, when they occur, are important components of trauma care. Over the last decade, progress has been made in developing such strategies, not just in trauma patients, but in all intensive care unit (ICU) patient populations. In fact, because sepsis and septic shock are such a major cause of mortality, an international group of experts from nine different societies met, and, through a Delphi-type process, developed a series of guidelines for the optimal treatment of sepsis and septic shock. These evidence-based recommendations were published in 2004 and are called the Surviving Sepsis Campaign guidelines.1
INCIDENCE
In trauma patients, injury not only predisposes to infection by promoting bacterial contamination of normally sterile tissues and spaces, but also induces the development of an immunocompromised state with infection and infection-related multiple organ failure being common causes of late death after trauma. Although the exact incidence of sepsis and septic shock in trauma patients is not fully known, the incidence of sepsis and septic shock is increasing nationally and affects an estimated 751,000 patients per year in the United States with an overall mortality in excess of 30%.2 This mortality rate is even higher in the presence of multiple organ failure, where mortality rates up to 85% have been reported. This increase in the incidence of sepsis and septic shock appears to involve trauma patients as well and can be attributed to several factors, including the aging of the population, which results in more elderly patients with significant comorbidities sustaining trauma. Additionally, advances in medical and surgical care have resulted in more severely injured patients surviving their initial injuries and thus being at risk for the subsequent development of infectious complications. Lastly, certain trauma-related variables appear to increase the risk of developing an infectious complication and these include the presence of preoperative shock, colon injuries, central nervous system (CNS) injuries, and injury to multiple organs as well as the administration of blood transfusions, due to their immunosuppressive effects.3
MECHANISM OF INFECTION
Infections in trauma patients may occur for many reasons. These include the global immunosuppressive effects of a major injury, patient-related factors, consequences of injuries to specific organs such as the intestine, as well as infections occurring after operations or due to the need for invasive monitoring or mechanical ventilation. For example, risk factors for sepsis include extremes of age and chronic underlying medical conditions, such as malnutrition, alcoholism, malignancy, and diabetes mellitus, all of which compromise the immune system.2 There is also evidence to suggest that some patients may have a genetic predisposition for the development of sepsis, as well as increased mortality when an infection is acquired.4 For example, genetic polymorphisms have been identified in the genes for TNF, IL-6, IL-10, IL-1 receptor antagonist, heat shock protein, CD14, and lipopolysaccharide binding proteins.2 There is even evidence that gender influences the risk of post-trauma sepsis with males being more susceptible than premenopausal females.5 Thus, genetic factors and to a lesser extent sex hormonal status may help explain the heterogeneity observed among patients developing infections after trauma as well as in the evaluation of new therapeutic molecules in patients with sepsis.
Another reason why infectious complications are relatively common in trauma patients is that traumatic injury itself leads to bacterial contamination of spaces that are normally sterile, while the presence of hematomas and devitalized or necrotic tissue causes an anoxic microenvironment that impairs the ability of the host’s antibacterial factors to effectively clear bacteria if these hematomas or devitalized tissue sites become infected. Clinical examples of this phenomenon are secondary infections of major liver injuries or splenic injuries treated with splenic artery embolization. Likewise, pulmonary contusions, which occur in 10%–25% of patients after blunt chest injury, are associated with impaired immune function and an increased susceptibility to infectious complications. Additionally, many of our therapeutic maneuvers potentially predispose patients to an increased risk of infection. For example, invasive monitoring lines allow bacteria colonizing the skin surface direct access to the bloodstream, while endotracheal tubes and Foley catheters also promote the development of pneumonia and urinary tract infection (UTI). In fact, the incidence of nosocomial infections in mechanically-ventilated trauma patients is relatively high and increases as the ICU length of stay increases, reaching over 50% in patients in the ICU more than 7–10 days. This increased infection rate appears to be associated with up to a three-fold increase in mortality, especially in patients with moderately severe injuries who might otherwise be expected to survive.6
DIAGNOSIS
The making of an early and accurate diagnosis of infection or septic shock is an important, but potentially difficult, aspect of the care of the trauma patient. One reason for this difficulty is that the common signs of infection, such as fever, leukocytosis, and tachycardia are relatively common in noninfected trauma patients and represent the host’s inflammatory response to injury. The fact that noninfectious septic responses are common after major trauma and can be indistinguishable from an infectious-mediated septic response therefore confounds diagnostic decision making. Furthermore, the need for ventilatory support and sedation in many of these patients further impairs the ability of the clinician to accurately question and examine the patient. Additionally, the presence of postoperative pain after procedures, such as a laparotomy, further limits the accuracy of abdominal symptoms or physical examination in the patient at risk for developing abdominal sepsis. For all of these reasons, vigilance, a high level of suspicion and knowledge of the likely sites of infection in each specific patient are required to facilitate the early diagnosis of an infection. Likewise, it is important to recognize that certain physiologic changes in the otherwise stable patient may be an early sign of a serious infection. Examples of these physiologic derangements, in addition to the standard signs of fever and tachycardia, include new onset ileus, a change in sensorium, fluid sequestration manifesting as an increasing need for fluids to maintain urine output, the development of a metabolic acidosis, or worsening of the patient’s respiratory status.
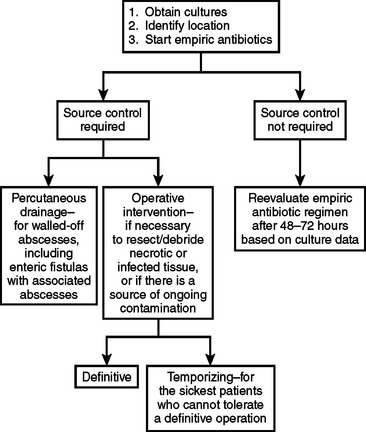
Since pneumonia, line sepsis, and infections at the sites of injury or previous operations are especially common in severely injured trauma patients, special attention should be focused on these areas in the at risk patient in whom infection is suspected. In fact, ventilator-associated pneumonia is one of the most common causes of infection-related death in the ICU and can be difficult to diagnose, as are episodes of life-threatening line sepsis. Whenever an infection is suspected, diagnostic studies to determine the causative organisms should be performed before the start of antibiotic therapy, although commencement of antibiotic therapy should not wait for diagnostic studies to be completed since the early treatment of an infection appears to reduce morbidity and mortality (Figure 1). Specifically, when infection is suspected, two sets of blood cultures should be drawn—one percutaneously, and one through any intravascular catheter more than 48 hours old. The rationale for drawing cultures from existing vascular lines is to screen for line sepsis and if the blood culture from the vascular line comes back positive earlier than the percutaneously drawn blood culture (i.e., >2 hours), this suggests that the vascular access device is a likely source of the infection.7 Additionally, as appropriate, cultures of urine, cerebrospinal fluid, and body fluids should be obtained. Bronchoscopy and bronchoalveolar lavage with quantitative cultures should be used for the diagnosis of ventilator-associated pneumonia. Radiologic imaging studies with sampling of potential sources of infection can also be helpful, especially in patients at risk of having intra-abdominal septic sites.
STAGING
An international sepsis definitions consensus conference of the American College of Chest Physicians and the Society of Critical Care Medicine attempted to define a staging system for sepsis. This was called PIRO (predisposition, insult or infection, response, and organ dysfunction). Predisposition includes premorbid conditions that influence the likelihood of infection, sepsis, morbidity, and survival. Insult or infection refers to the specific organism causing the septic response, the sensitivity pattern, and whether the infection is community acquired or nosocomial. Response attempts to quantify the clinical manifestations of the systemic inflammatory response syndrome (SIRS), by using markers such as procalcitonin, IL-6, HLA-DR, TNF, PAF, and C-reactive protein. Organ dysfunction refers to the type and number of dysfunctional organs, and whether it is reversible or irreversible.8 Organ dysfunction is judged by other scoring systems discussed elsewhere in this text, including multiple organ dysfunction syndrome (MODS) score, logistic organ dysfunction system (LODS), and sequential organ failure assessment (SOFA). Although the PIRO classification is not in wide use, it provides a conceptual framework for staging sepsis (Table 1).
Table 1 PIRO Staging of Sepsis
| Predisposition | Premorbid conditions influencing the likelihood of infection, sepsis, morbidity, or survival (age, sex, hormonal state, genetic polymorphisms) |
| Insult/infection | Insult or organism associated with the sepsis response (type of organism, sensitivity pattern, community or nosocomial acquisition) |
| Response | Clinical manifestation of the SIRS response (procalcitonin, IL-6, TNF, C-reactive protein) |
| Organ dysfunction | Type and number of dysfunctional organs (reversible vs. irreversible dysfunction), severity of dysfunction (judged by scoring systems such as MODS, LODS, and SOFA) |
IL, Interleukin; LODS, logistic organ dysfunction score; MODS, multiple organ dysfunction score; SIRS, systemic inflammatory response syndrome; SOFA, sequential organ failure assessment; TNF, tumor necrosis factor.
Adapted from Magnotti LJ, Croce MA, Fabian TC: Is ventilator-associated pneumonia in trauma patients an epiphenomenon or a cause of death? Surg Infect (Larchmt) 5:237–242, 2004.
MEDICAL AND SURGICAL MANAGEMENT
Management of sepsis due to an infectious process begins with prompt recognition that an infection is likely, determination of the probable site of infection and assessment of the severity of the physiologic derangements. Based on the source and cause of the infection, specific therapy may be limited to antibiotics or require a combination of antibiotics plus operative or interventional source control. The choice of antibiotics depends on the suspected site of infection and the organisms that commonly inhabit that location (Table 2). Antibiotic choice may have to be modified for patients likely to have an abnormal flora, such as patients who have had a previous course of antibiotics or those who have been colonized by hospital-acquired pathogens. In these circumstances, treatment is initiated with a single agent or combination of agents with the lowest possible toxicities, whose spectrum of activity is broad enough to cover all suspected pathogens. Since victims of major trauma are at increased risk of developing multiple infections, it is crucial that antibiotics are stopped as soon as possible to limit the emergence of antibiotic-resistant bacteria. There is no good evidence to suggest that antibiotic treatment should exceed 7–10 days, except in unusual circumstances. Likewise, in determining the length of antibiotic use, it is also important to differentiate between prophylaxis and therapy, especially in the trauma patient in whom injury-induced bacterial contamination may have occurred. For example, in a trauma patient undergoing laparotomy for blunt or penetrating trauma, the patient receives preoperative antibiotics (usually a second-generation cephalosporin), which are usually stopped within 24 hours postoperatively. However, if a major degree of contamination is present, as in a colon injury where the incidence of abdominal abscess formation reaches over 25%,9 the antibiotics should be continued for 3–5 days, since they serve both prophylactic (for the wound) and therapeutic roles (for the peritoneum).
Table 2 Common Organisms and Antibiotic Choice Based on Location of Suspected Infection
| Site | Common Community-Acquired Organisms and Treatment | Common Nosocomial Organisms and Treatment |
|---|---|---|
| Lung | Streptococcus pneumoniae, Haemophilus influenzae, Legionella, Chlamydia, Pneumocystic carinii | Aerobic Gram-negative bacilli |
| Macrolide and third-generation cephalosporin or levofloxacin | Cefepime or imipenem-cilastatin with aminoglycoside | |
| Abdomen | Escherichia coli, Bacteroides fragilis | Aerobic Gram-negative rods, anaerobes, Candida |
| Imipenem-cilastatin or piperacillin-tazobactam with or without aminoglycoside | Imipenem-cilastatin with or without aminoglycoside, or piperacillin-tazobactam with or without amphotericin B | |
| Skin/soft tissue | Group A Streptococcus, Staphylococcus aureus, Clostridium, polymicrobial, enteric Gram-negative rods, Pseudomonas Aeruginosa, anaerobes, Staphylococci | Staphylococcus aureus, aerobic Gram-negative rods |
| Vancomycin with or without imipenem-cilastatin or piperacillin-tazobactam | Vancomycin with cefepime | |
| Urinary tract | Escherichia coli, Klebsiella sp., Enterobacter sp., Proteus sp. | Aerobic Gram-negative rods, Enterococci |
| Ciprofloxacin with or without aminoglycoside | Vancomycin with cefepime | |
| CNS | S. pneumoniae, Neisseria meningitidis, Listeria monocytogenes, E. coli, H. influenzae | P. aeruginosa, E. coli, Klebsiella, Staphylococcus |
| Vancomycin, third-generation cephalosporin, or meropenem | Cefepime or meropenem with vancomycin |
Adapted from Balk RA: Optimum treatment of severe sepsis and septic shock: evidence in support of the recommendations. Dis Month 50:163–213, 2004.
However, even in spite of appropriate initial surgical management, postoperative intra-abdominal infections remain a major cause of morbidity and mortality in the trauma victim. Although the peritoneal cavity is relatively resistant to a bacterial challenge, the presence of adjuvant substances such as fibrin or hemoglobin allows bacteria to evade the normal host defenses and can result in intra-abdominal infection. Thus, if there is suspicion of a postoperative intra-abdominal infection, the primary goal is to determine whether the patient has intra-abdominal sepsis, and if so, to determine the necessity and timing of reoperation versus percutaneous therapy. In this situation, the most useful diagnostic modality in a stable patient is a helical abdominal computed tomography (CT) scan. Abdominal CT scan has a sensitivity of 97% and a specificity of 65% in diagnosing an intraabdominal source of sepsis.10 If there are no signs of overwhelming sepsis and the CT scan shows evidence of a localized abscess, whether in the peritoneal cavity or at the site of an injured organ, such as the liver, the intra-abdominal infection usually can be managed nonoperatively with fluid resuscitation, CT-guided drainage of the abscess and broad-spectrum antibiotics. This is especially useful in the patient who has undergone multiple abdominal operations, where relaparotomy can be difficult. Even though anastomotic leaks and breakdowns may result in severe sepsis or the formation of an enterocutaneous fistula, these patients still may be candidates for percutaneous drainage if there is no evidence of continuing contamination, if the catheter drainage route does not traverse bowel or uncontaminated organs and the infectious source is controlled by catheter drainage.11 In contrast, when these conditions can not be met, or in the patient with diffuse peritonitis, prompt reoperation to control the source of infection and provide drainage is mandatory and can be life-saving.