172 Sepsis
• Sepsis encompasses a spectrum of diseases: infection with signs of a systemic inflammatory response, severe sepsis, and septic shock.
• Treatment in the emergency department includes early, presumptive administration of antibiotics and early, aggressive fluid resuscitation, with the use of central venous pressure monitoring and vasopressors when appropriate to optimize resuscitation.
• Patients with severe sepsis and septic shock must be monitored closely and should be admitted to an intensive care unit.
Epidemiology
In the United States alone, more than 750,000 cases of sepsis occur, and approximately 215,000 deaths result from this disease annually.1 Over the 25-year period between 1972 and 1997, little change occurred in the mortality rate (ranging from 40% to >60%) for patients with septic shock.2 More recent advances in the early treatment of severe sepsis and septic shock have shown improvements in mortality and thus promise for patients and their treating physicians.3–5
Pathophysiology
Sepsis is defined as a condition in which an identified or suspected source of infection leads to a systemic inflammatory process, known as the systemic inflammatory response syndrome (SIRS) (Box 172.1). Severe sepsis refers to sepsis that has progressed to cellular dysfunction and organ damage or evidence of hypoperfusion, whereas septic shock refers to sepsis with persistent hypotension despite adequate fluid resuscitation. SIRS can develop when an exaggerated response of the body’s immune system to infection results in the release of inflammatory cytokines (tumor necrosis factor-α, interleukin-1, and interleukin-6) as the immune cells encounter the organisms’ endotoxins.6 These cytokines can lead to activation of the coagulation cascade with subsequent thrombosis and disseminated intravascular coagulation, as well as the release and activation of nitric oxide, thought to be the key mediator in vasodilation and shock.4,7 Progression of shock can lead to poor oxygen delivery and use at the tissue level, thereby creating an environment in which lactic acid is generated and mixed venous oxygenation is impaired.
Box 172.1 Definition of Systemic Inflammatory Response Syndrome
The presence of two or more of the following four items constitutes sepsis:
• Temperature lower than 36° C or higher than 38° C
• Heart rate greater than 90 beats per minute
• Respiratory rate greater than 20 breaths per minute or partial pressure of arterial carbon dioxide lower than 32 mm Hg
• White blood cell count lower than 4000 or higher than 12,000 cells/mm3 or more than 10% bands
Presenting Signs and Symptoms
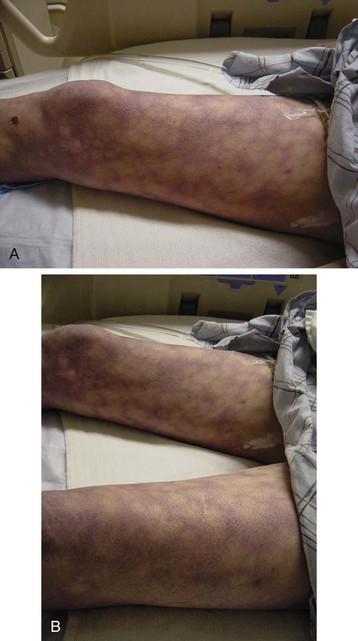
The patient with classic severe sepsis or septic shock appears ill, with fever (less commonly hypothermia) and chills, an increased respiratory rate, and tachycardia. Patients may have cold skin showing outward signs of decreased perfusion (Fig. 172.1), and they may have mental status changes.
The presentation may or may not direct the clinician to the potential source of infection. For example, dyspnea and crackles on a lung examination may point to a pneumonia source, or left lower quadrant tenderness on an abdominal examination may point to diverticulitis as the source. Determining the site of infection in the emergency department (ED) may be difficult, and even retrospectively, an initial source is not determined in up to 15% of patients (Box 172.2).8
More objective measures (SIRS criteria, lactate level, mixed venous oxygenation) are used to determine whether a patient has sepsis because patients can sometimes appear surprisingly well even when they have severe sepsis or septic shock. Their only complaint may be fever, even though other SIRS criteria and hypotension may be present, especially in relatively younger, healthier, immunocompetent patients (see Fig. 172.1).
Differential Diagnosis and Medical Decision Making
The diagnostic work-up may vary among patients, but most patients require standard testing to start. Serum lactate has become an important risk stratification tool because both the initial serum lactate level and lactate clearance have been shown to be important predictors of mortality.9,10 Further work-up should be guided by the suspected source of infection. For example, concern about a possible abdominopelvic infection (e.g., diverticulitis, acute cholecystitis) may warrant a computed tomography scan of the abdomen or pelvis or a right upper quadrant ultrasound scan, whereas concern about a possible central nervous system infection (e.g., meningitis) may warrant lumbar puncture. A procalcitonin level determination may be helpful in guiding therapy and predicting outcomes, whereas future molecular assays may help in more rapid identification of pathogens.11,
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree