Scoring for Injury and Emergency Surgery
Edward Kwon
John Fildes
I. Introduction
Injury severity scoring in trauma plays many important roles in the management of the injured patient, beginning with quantifying injuries. This allows the stratification of patients based on the types of injuries and predicts the probability of survival based on severity of injury. These two main functions play a particularly important role in field triage, identification of patients who may require higher levels of care, and allocation of resources.
In addition, scoring systems play a valuable role in research allowing similarly injured patient populations to be compared. Scoring systems in trauma surgery are widely used in research and measurement of outcomes of the injured patient.
Scoring systems in emergency general surgery are not as well established as for trauma.
Types of scoring systems. Three major types of scoring systems are used to assess the severity of injury: Anatomic, physiologic, and combined. Anatomic scoring systems as suggested by the name, consider solely the anatomic characteristics of injuries for stratification, the best known of which include the Abbreviated Injury Scale (AIS), Injury Severity Score (ISS) and the individual organ injury scales. Physiologic scoring systems utilize various physiologic markers such as blood pressure, heart rate, and similar variables to assess severity including the Glasgow Coma Scale (GCS), Revised Trauma Score (RTS) and the Acute Physiology and Chronic Health Evaluation II Score (APACHE II). Combined scoring systems are a composite of anatomic and physiologic scoring systems utilized mainly to predict outcomes. Examples of combined systems include the Trauma and Injury Severity Score (TRISS) and “A Severity Characterization of Trauma (ASCOT).”
II. Scoring Systems in Injury and Trauma
Anatomic scoring
Abbreviated Injury Scale (AIS). The AIS was developed in 1969 by a Joint Committee of the American Medical Association called the Society of Automotive Engineers and the Association for the Advancement of Automotive Medicine and has undergone several revisions, most recently in 2008. AIS is a consensus derived scale rather than a scoring system, which classifies injuries into six separate body regions including head/neck, face, thorax, abdomen/pelvis, extremities, and external structures. Injuries are then further stratified into types of injuries and assigned a score of 1 to 6 with 1 representing minimal injury and 6 a fatal injury (Table 60-1). The AIS is a useful descriptive tool to catalogue similar injuries rather than a predictive model, as there is no linear correlation between classified injuries and outcomes, and does not account for multiple injuries in a given patient.
Table 60-1 General Categories of the Abbreviated Injury Scale
Abbreviated injury scale
Injury
Score
Minor
1
Moderate
2
Serious
3
Severe
4
Critical
5
Unsurvivable
6
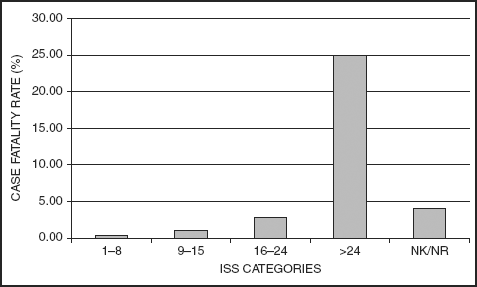
Injury Severity Score (ISS). The ISS was proposed in 1974 to more accurately assess severity of injury by recognizing that patients who did not have similar injuries may still have similar overall injury severity based on multiple injuries. ISS is based on the AIS and calculated by the squaring of the highest AIS scores in the three most severely injured areas and adding the scores. An AIS score in any anatomical region of 6 automatically equates to an ISS of 75 and is considered fatal. A higher ISS score correlates with severity of injury and mortality. An ISS score between 1 and 8 (minor) is associated with a mortality of 1%; ISS 9 to 15 (moderate), a mortality of 2%; ISS 16 to 24 (severe), a mortality of 7%; and ISS
>24 (very severe) a mortality of >30% (Table 60-2). The major limitations of the ISS are because it is based on the AIS; ISS does not account for multiple injuries in a given body region, underestimates severity and weighs all body regions equally. For example, an AIS injury of 5 in an extremity is equal to an AIS injury of 5 in the head although an extremity AIS of 5 is associated with a much lower mortality. Despite these limitations, the ISS is the most popular scoring system.
Table 60-2 Case Fatality Rates by Injury Severity Score from the 2010 National Trauma Data Base
New Injury Severity Score (NISS). The NISS was created in 1997 to address the limitation of the ISS in its inability to account for more than one injury in a given anatomic region. NISS is calculated in the same manner to the ISS but uses the three highest AIS scores regardless of anatomic region, thus allowing for multiple injuries in a single anatomic region. The NISS has been found to have increased correlation with mortality compared to ISS. However, ISS remains the standard anatomic ISS.
American Association for the Surgery of Trauma (AAST) Organ Injury Scale (OIS). The OIS was developed in 1987 by a committee appointed by the AAST as a method to accurately describe and stratify the severity of injuries to individual organs (see the Injury Scales Appendix). The individual organ scales
were developed by literature examination and expert consensus. Individual organ injuries are given a score from 1 to 6 based on specified parameters; such as anatomic location within an organ, size of injury, laceration versus hematoma, and blunt versus penetrating, thereby reflecting severity (Table 60-3). The OIS score provides a common descriptive terminology for individual organ injuries based on severity making it particularly useful for clinical research, prognostication, and therapeutic planning as well as its wide acceptance.
Table 60-3 Example of AAST OIS Score for Splenic Injury
Gradea
Injury type
Description of injury
ICD-9
AIS-90
I
Hematoma
Subcapsular, <10% surface area
865.01
2
865.11
Laceration
Capsular tear, <1 cm parenchymal depth
865.02
2
865.12
II
Hematoma
Subcapsular, 10–50% surface area
865.01
2
Intraparenchymal, <5 cm in diameter
865.11
Laceration
Capsular tear, 1–3 cm parenchymal depth that does not involve a trabecular vessel
865.02
865.12
2
III
Hematoma
Subcapsular, >50% surface area or expanding; ruptured subcapsular or parenchymal hematoma; intraparenchymal hematoma ≥5 cm or expanding
3
Laceration
>3 cm parenchymal depth or involving trabecular vessels
865.03
865.13
3
IV
Laceration
Laceration involving segmental or hilar vessels producing major devascularization (>25% of spleen)
4
V
Laceration
Completely shattered spleen
865.04
5
Vascular
Hilar vascular injury which devascularizes spleen
865.14
5
aAdvance one grade for multiple injuries up to grade III.
Anatomic profile (AP). The AP was developed in 1990 to address the limitations of the ISS counting only injury to the single most severe injury in a given body region and the assignment of equal weights to injuries regardless of body region. The AP divides injuries into three different body regions including head/spine, neck/thorax, and other. All injuries within a given body region with an AIS >2 are then modified and weighted and used in an equation to calculate the AP score. Despite the increased sensitivity of the AP in comparison to the ISS in predicting mortality, it has not gained wide acceptance.
International classification of diseases injury severity score (ICISS). Proposed in 1996, the ICISS is a scoring system, which is based on ICD-9 codes rather than AIS scores. Survival risk ratios (SRR) are determined for each ICD-9 code utilizing trauma databases to identify the number of patients who survive each coded injury and dividing that number by the total number of patients with that particular injury. The product of all of the SRR for a given patient is then calculated to give the ICISS. The ICISS more accurately predicts survival and mortality compared to ISS and also has the advantage of requiring only the ICD-9 codes to calculate which is readily available as all hospitals utilize ICD-9 coding for reimbursement.
Physiologic scoring
Glasgow Coma Scale (GCS). Introduced in 1974, the GCS scoring system is one of the most widely used and accepted trauma scoring systems. The GCS score is used to stratify neurologic injury based on three clinical findings: Eye opening,
verbal expression, and motor response. Each component is given a score based on the best response with a range of 1 to 4 for eye opening, 1 to 5 for verbal, and 1 to 6 for motor response to yield the sum overall GCS of 3 to 15 (Table 60-4). The GCS score allows the stratification of neurologic injury in a rapid and simple manner making it particularly useful for field and hospital triage, management decisions (intubation, intracranial pressure monitoring, and surgical decompression), as well as prognostication and research. While used outside neurotrauma, the GCS is not designed for other conditions and has an uneven utility in those settings.
Table 60-4 Glasgow Coma Scale
Eye opening (4)
Spontaneous
4
To voice
3
To pain
2
None
1
Verbal response (5)
Oriented
5
Confused
4
Inappropriate
3
Incomprehensible
2
None
1
Motor response (6)
Follows commands
6
Localizes to pain
5
Withdraws to pain
4
Flexion (decorticate posturing)
3
Extension (decerebrate posturing)
2
None
1
Total GCS
3–15
Table 60-5 Revised Trauma Score
Glasgow coma scale (GCS)
Systolic blood pressure mm Hg (SBP)
Respiratory rate per minute (RR)
Coded value
9–12
76–89
>29
3
6–8
50–75
6–9
2
4–5
1–49
1–5
1
3
0
0
0
RTS = 0.9368 GCS + 0.7326 SBP + 0.2908 RR. 
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







