Maxillofacial Injury
William L. Chung
James M. Russavage
Mark W. Ochs
I. Evaluation of the Patient with Suspected Maxillofacial Trauma
Treatment principles of hard- and soft-tissue injuries
Contusions or lacerations often accompany underlying bony injuries; consider imaging, especially if tenderness or deformity exists.
Treat fractures of the maxillofacial complex before definitive soft-tissue management to avoid repetitive damage to the latter. It may be possible to repair open fractures exposed through any lacerations rather than the standard incision for fracture repair.
Tissue that is contaminated or damaged by crush or contusion is at risk for infection if primary repair is performed. The likelihood of contamination increases proportional to the length of time elapsed since the injury.
The history and mechanism of injury provide evidence of the possibility of retained foreign bodies.
Initial survey
Relieve airway obstruction/ensure adequate oxygenation and ventilation.
Control hemorrhage.
Search for immediately life-threatening injuries (thoracic, abdominal, intracranial, extremity).
Assume cervical spine (C-spine) injury exists and stabilize until it is cleared.
Perform a neurologic assessment.
Secondary survey
Complete head, eye, ear, nose, throat (HEENT) examination.
Scalp and skull evaluation (palpate).
Cranial nerve evaluation (especially optic, CN II). Evaluate structural function(s) in the vicinity of the injury.
Ophthalmologic evaluation (pupil symmetry, reactivity, visual acuity, and ocular movement).
Otologic evaluation (external ear structures and otoscopic examination).
Evaluate nasal structures, sinuses, salivary glands, and associated ducts.
Photography. Useful for:
Accurate record keeping and documentation.
Insurance and legal purposes.
Assess efficacy of therapy.
II. Dentoalveolar Trauma
Anatomy
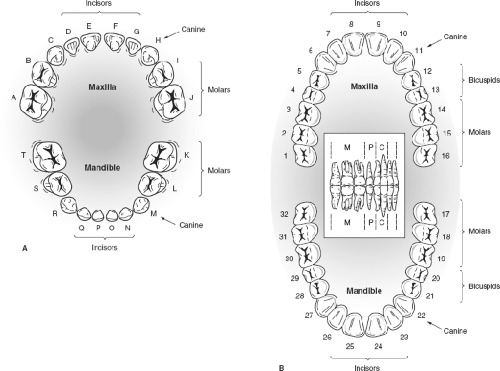
Adult dentition is composed of 32 teeth, including bilateral maxillary and mandibular central and lateral incisors, canines, first and second bicuspids, and three molars. Typically, the third molars (wisdom teeth) are impacted or absent. The teeth are numbered from the right maxillary third molar (no. 1) moving forward and across the arch to the left maxillary third molar (no. 16), then the mandibular left third molar (no. 17) and across to the right wisdom tooth (no. 32) (Fig. 24-1A).
The pediatric dentition consists of 20 total deciduous teeth, including bilateral maxillary and mandibular central and lateral incisors, canines, and two molars
(Fig. 24-1B). The primary dentition is named by capital letters. Exfoliation of the deciduous teeth begins at approximately 6 years of age and the mixed dentition stage continues until 12 to 14 years of age. The teeth are attached to the alveolar processes of the maxilla and mandible by periodontal ligaments. Alveolar bone in younger age groups undergoes plastic deformation when subjected to trauma.
Evaluation
Clinical
Count all of the teeth; attempt to locate any missing teeth at the location of the injury. With unaccounted or missing teeth, look for traumatic impaction into the local bone or surrounding soft tissues. Also, dislodged teeth can be aspirated or swallowed. Chest or neck imaging can help locate swallowed teeth.
Evaluate the occlusion and ask the patient if the bite feels normal; this is a sensitive screening tool to detect a dentoalveolar or facial fracture. Assess next for stability and symmetry. Occlusal discrepancies, new gaps in the dental arch, or lacerations of the usually pink, firm, attached gingival raise the suspicion of a fracture.
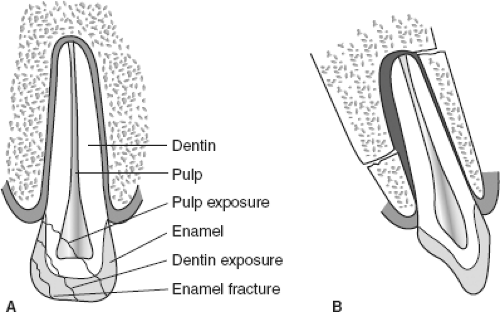
Evaluate damaged or displaced teeth. Fractured teeth can be classified by the depth and location of the fracture (Fig. 24-2A, B). Dislocated teeth can be totally avulsed or subluxated or an associated alveolar fracture may be present.
Radiographs
Management
Age of the patient, type of tooth (deciduous or permanent), status of tooth development, condition of tooth before trauma, patient motivation, time elapsed since injury, and associated injuries all influence the management of dentoalveolar trauma.
Intraoral soft-tissue lacerations are usually best treated by conservative debridement, irrigation, and primary repair with resorbable sutures after stabilization or definitive treatment of the dentoalveolar fracture.
In general, isolated tooth crown fractures need emergent referral if the dental pulp (dark pink or red appearance) is exposed or if teeth are sensitive.
Dislocated or subluxed teeth and dentoalveolar fractures need to be emergently reduced and stabilized with wire and composite resin bonding. Composite resins are opaque white filling material (similar to what orthodontists use to bond brackets to teeth) that is either chemically or UV light activated.
Avulsed deciduous (pediatric) teeth should not be reimplanted because of low success rate and the possibility of damage to the underlying developing permanent dentition.
Avulsed permanent teeth should be replaced into the tooth socket as soon as possible after the trauma. Immediate reimplantation is ideal. If this is not possible, the tooth should be stored in an appropriate storage medium (avulsed tooth storage system, buccal vestibule, milk, saline, or moist towel) and replaced as soon as possible, with less than 30 minutes ideal. A delay of 2 hours or desiccation of the tooth root markedly drops the overall success of reimplantation. Once reimplanted, the tooth requires composite resin splinting to the adjacent stable teeth, and tell patients to avoid heavy chewing/solid ingestion until seen in follow-up within a week.
III. Mandibular Fractures
Mandibular fractures are the second most common of bony maxillofacial fractures. The mechanism of injury is usually blunt trauma from an assault or a motor vehicle crash.
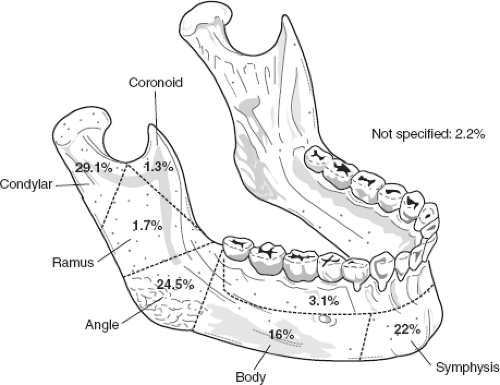
Anatomy and location of injury. Fractures tend to occur at the local site of impact, areas of weakness, and are often multiple. The anatomic regions and associated incidence of fracture are shown in Figure 24-3. In edentulous patients, the incidence of subcondylar fractures accounts for 37% of all mandible fractures and is often paired with a contralateral body fracture. The inferior alveolar neurovascular bundle enters the mandible on the medial aspect of the mid-ramus through the mandibular foramen and traverses an intrabony canal, exiting through the mental foramen located just inferior to the mandibular bicuspid root tips. It is strictly a sensory nerve (V3) supplying the ipsilateral lower lip, teeth, and gingiva.
Evaluation
Clinical
Emergent situations
Airway obstruction. Foreign bodies (e.g., dentures, avulsed teeth) can cause airway obstruction; remove them at the time of initial evaluation.
In addition, airway obstruction can occur with bilateral mandibular parasymphyseal or body fractures. Manual anterior distraction of the flail anterior mandibular segment, allowing the patient to be semi-supine or to sit up, and oral suctioning can provide temporary relief, but a definitive airway should be secured urgently.
Hemorrhage is rarely a significant problem with mandibular fractures.
The inferior alveolar artery traveling in the mandibular canal can be lacerated during the initial injury, but simple fracture reduction, direct pressure, or infiltration with an epinephrine containing local anesthetic is usually adequate for hemostasis.
Persistent or profuse bleeding is often associated with penetrating injury and a secure airway is the primary concern. Then, control bleeding with direct surgical exploration, or rarely, by interventional radiology. Fracture reduction and temporary stabilization are preferred for hemorrhage control. Local packing can cause fracture distraction, allowing continued bleeding.
Occlusion. Malocclusion is one of the first clinical signs detected in patients with a mandibular fracture. If the fracture is in the tooth-bearing segment of the mandible, a noticeable step deformity or interdental gap may be detected.
Floor of mouth ecchymosis is pathognomonic for a mandibular parasymphyseal or body fracture. If the fracture is located in the subcondylar region, a shift of the chin toward the affected side or an anterior or lateral open bite may be present (Fig. 24-4).
Soft-tissue signs, such as ecchymosis, edema, pain, and gingival or mucosal lacerations, may be present at the fracture site.
Sensation. Lower lip and chin paresthesia or anesthesia is common in patients with mandible fractures located between the mid-ramus and canine region. Greater bony displacement increases the risk for inferior alveolar nerve injury or even transection.
Radiographs. Plain radiographs usually suffice for evaluation of mandibular fractures. At least two views at 90 degrees should be used to evaluate most injuries. This is especially important in the subcondylar region, where superimposition of other structures can mimic or obscure a fracture.
The best initial radiograph is the panorex, accompanied by an open mouth Towne’s view. Other radiographs that can be used to evaluate mandibular fractures are the posteroanterior (PA) and lateral oblique views.
Computed tomography (CT) aids the evaluation of patients with condylar or subcondylar fractures. This is particularly true in children because their condyles are developing and incompletely ossified, making plain radiology detection difficult. Patients (especially children) with a chin laceration and preauricular pain or swelling should be evaluated for a condylar or subcondylar fracture. Coronoid fracture accounts are uncommon and are generally associated with an overlying zygomatic complex fracture that was displaced medially, creating the injury.
Management
Cervical immobilization
Cervical immobilization should be maintained until C-spine injury is excluded unless a trivial mechanism exists.
Management of emergent problems
Initial management should be control of the airway and bleeding. Control of the airway is performed with distraction of flail bony segments, if possible. In the event of a compromised airway, perform endotracheal intubation or surgical airway before stabilization and repair of the mandibular fracture.
Temporary immobilization
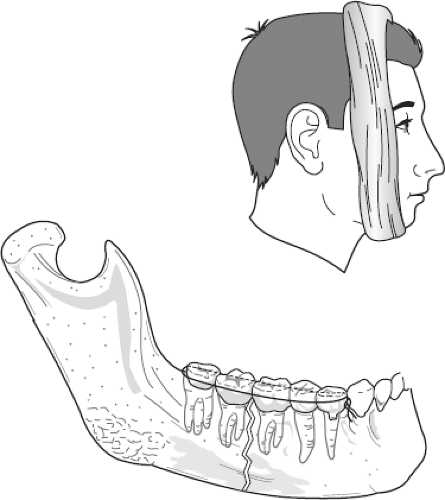
Temporary partial reduction and stabilization of the fracture segments can provide symptomatic relief, help control bleeding, and minimize damage to the inferior alveolar neurovascular bundle. This can be performed with a modified Barton’s bandage (circumferential wrap from chin to skull vertex) or by placing a stainless steel bridal wire (24 to 26 gauge) around the necks of two teeth on either side of the line of fracture (Fig. 24-5).
Definitive treatment
Fractures should be reduced adequately, fixated, and immobilized for adequate healing to occur. This is typically accomplished by open reduction and internal screw fixation. Without immobilization, fracture segments usually become
displaced by the pull of muscles of mastication, leading to a malunion or nonunion. Isolated minimally displaced fractures, particularly those of the condylar region, can be treated by wiring the teeth, or maxillomandibular fixation (MMF). The period of MMF for subcondylar fractures is 2 to 3 weeks to avoid the risk of ankylosis; 6 weeks for all other mandibular fractures.
Prophylactic antibiotics. Mandibular fractures that include tooth-bearing segments are considered compound fractures because of the egress of saliva, bacteria, and other contaminants through the periodontal ligament or fracture site. Prophylactic antibiotics that cover most oral microorganisms (e.g., penicillin, amoxicillin with clavulanate) or a first-generation cephalosporin are recommended, along with oral saline or antimicrobial (Peridex) rinses. In the penicillin-allergic patient, clindamycin is an alternative.
IV. Midface Fractures
Are any fracture of the orbital–zygomatic–maxillary complex. The mechanism of injury is usually blunt trauma from either an assault or motor vehicle crash.
General midfacial fracture management
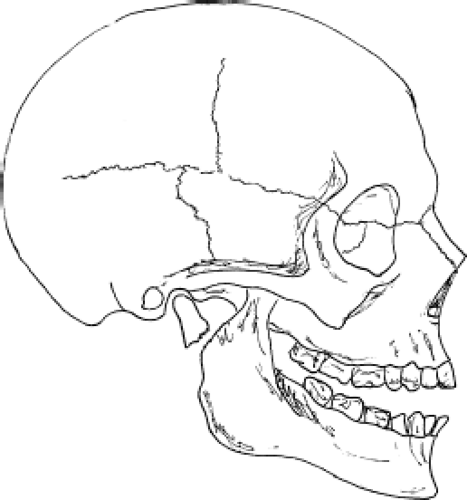
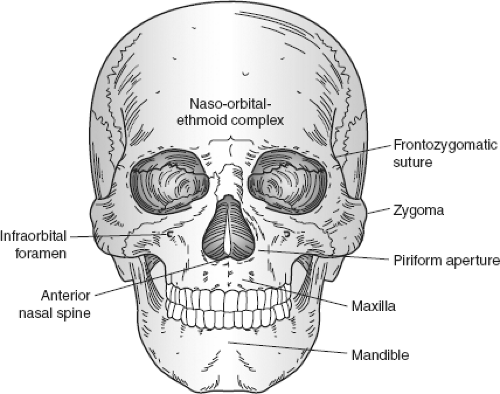
Anatomy and location of injury. The midface is divided into the maxilla, the zygomatic complexes, and the nasal–orbital–ethmoid (NOE) complex (Fig. 24-6). Fractures tend to occur at the site of impact and inherently weak regions of the midfacial complex, including bony sutures, foramina, and apertures.
The infraorbital neurovascular bundle enters the midfacial complex via the orbital region through the inferior orbital fissure and then traversing
partially through a bony canal along the floor of the orbit to exit through the infraorbital foramen on the anterior surface of the maxilla. The infraorbital nerve (V2) supplies general sensation to the ipsilateral lower eyelid, lateral nose, upper lip, and anterior maxilla.
Evaluation
Clinical
Emergent situations
Airway obstruction. In most clinical situations, airway obstruction occurs in patients with panfacial trauma, including significant mandibular fractures.
Hemorrhage. Significant hemorrhage is more common with midfacial fractures than mandibular fractures. The descending palatine arteries, which travel in a bony canal along the posterior surface of the nasal cavity within the palatine bone, can cause profuse posterior nasal bleeding. Other vessels that may be injured include the nasal septal, sphenopalatine, and pterygoid plexus.
Occlusion. Occlusal discrepancies are one of the first clinical signs detected in patients with certain midfacial fractures. Mobility of the maxillary teeth relative to other midfacial structures is pathognomonic of a maxillary fracture. A posteriorly directed force of significant magnitude can cause a posteriorly impacted maxilla. Either an anterior or posterior open bite is indicative of a maxillary or midfacial fracture.
Soft-tissue signs include ecchymosis, edema, pain, and mucosal lacerations.
Palpation. Palpate all bones of the midface, including maxilla, orbital rims, zygomas, and nose; often, the patient is too sensitive to allow a complete examination. However, grasping the anterior maxillary teeth with the thumb and forefinger and attempting upward or side-to-side movement while stabilizing the entire forehead with the opposite hand is crucial in detection of a midfacial fracture.
Sensation. Upper lateral lip, nose, and cheek paresthesia or anesthesia is common in patients with a fracture extending through the infraorbital foramen. Complete transection of the infraorbital nerve is uncommon in blunt trauma.
Ophthalmologic examination. Any fracture involving the bony orbit or zygomatic complex can cause injury to the globe or other orbital contents. Complete examination includes pupils, visual acuity, range of motion of the globe, globe position, and the globe itself, including a funduscopic examination. Extraocular movements in multiple fields of gaze are often diminished in patients with significant orbital edema, but tend to be mild without a firm fixed sudden stop. Blowout fracture of one of the orbital walls (most commonly the medial orbital floor) can cause entrapment of the extraocular muscles (inferior rectus muscles or inferior oblique). A firm, fixed and reproducible point of limitation in upward gaze or, more likely, downward gaze should alert the practitioner to this possibility. An urgent specialist consultation is appropriate because prolonged muscle ischemia and resultant fibrosis can lead to long-term impairment of movement.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree