Spinal Cord and Spinal Column
Matthew Sanborn
Lachlan J. Smith
Neil R. Malhotra
Introduction
Each year, nearly 250,000 individuals will suffer an injury involving the spine. In the United States, approximately 10,000 new patients with spinal cord injury (SCI) are seen yearly. The impact of SCI is disproportionately large relative to its incidence given the frequency of disability and occurrence in a relatively young population in the prime of productivity. Since 2005, the mean age of a patient with a SCI is 40 years with 80% of injuries occurring in men. The estimated cost of SCI in the United State is $9.7 billion.
Of patients with spinal cord injuries, 44% also suffer from other significant injury, with 14% having head and facial injury. Half of all spinal cord injuries involve the cervical spine, most occurring between C4 and C7, with a 3-month mortality of 20%. One-half of spinal cord injuries involve complete quadriplegia.
The median age of patients with SCI has increased in recent years, reflecting an increase in the median age of the US population. This increase in median age is reflected in falls (27.9%) superseding violence (15.0%) as the second most common cause of SCI. The most common cause remains motor vehicle crashes (40.4%).
Anatomy
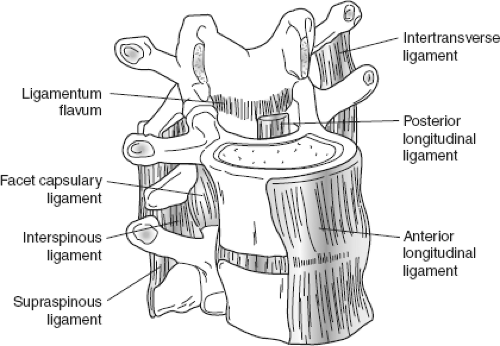
The human spinal cord has 31 segments including 8 cervical, 12 thoracic, 5 lumbar, and 6 sacro-coccygeal segments. The spinal canal is surrounded by bony structures: The vertebral body anteriorly, the pedicles laterally, and the lamina posteriorly. With the exception of the sacral vertebra, the vertebral bodies articulate with each other across the intervertebral disc anteriorly and facet joints posteriorly, forming a functional spinal unit. The facet joints, associated ligamentous structures, and other bone articulations (e.g., the rib cage) determine the motion across two vertebral bodies (Fig. 25-1). Motions can be in the sagittal plane (flexion and extension), coronal plane (lateral flexion), and in the transverse plane (rotation).
The adult spinal cord begins at the level of the cervicomedullary junction as the spinal cord passes through the foramen magnum of the skull to join the medulla of the brainstem. The spinal cord is surrounded by the three layers of the meninges which are contiguous with the cranial compartment. The dura mater is the outermost, tough layer, followed by the arachnoid that loosely invests the spinal cord and contains space for the cerebrospinal fluid (CSF). The pia mater is tightly adherent to the spinal cord itself. The spinal cord tapers to an end at the conus medullaris posterior to the L1–L2 vertebral body.
The spinal cord contains white matter tracts consisting of axons originating from upper motor neurons (UMNs) within the brain. These axons synapse with lower motor neurons (LMNs) within the gray matter of the spinal cord that send axons out in the form of nerve roots and the cauda equina. Lesions of the UMNs or their axons result in spasticity, while lesions of the LMNs or their axons result in flaccid paralysis. Generally speaking, UMN lesions carry a worse prognosis than LMN lesions, as nerve roots have better capacity for repair than the spinal cord. Further, because LMN have overlapping motor and sensory distributions, minor injuries may have limited sequela. After exiting the spinal canal, the nerve roots in the cervical and lumbar regions fuse as the cervical and lumbar plexuses before separating again as specific nerves.
In the cervical spine nerve roots exit above the like-numbered pedicle, with C1 exiting between the cranium and the pedicle of C1, and C8 exiting beneath the pedicle of C7. The spinal canal in the cervical region is generally more capacious than in the thoracic or lumbar
regions. Facets are oriented in a coronal plane and overlap one another like roof-tiles, thus coupling ipsilateral bending with contralateral axial rotation. In the cervical spine, about 50% of flexion and extension occurs between the occiput and C1, whereas 50% of rotation occurs between C1 and C2. The remainder of cervical movement takes place in the subaxial (below C2) region.
regions. Facets are oriented in a coronal plane and overlap one another like roof-tiles, thus coupling ipsilateral bending with contralateral axial rotation. In the cervical spine, about 50% of flexion and extension occurs between the occiput and C1, whereas 50% of rotation occurs between C1 and C2. The remainder of cervical movement takes place in the subaxial (below C2) region.
In the thoracic spine, nerve roots exit beneath like-numbered pedicles with the T1 nerve root exiting beneath the pedicle associated with the T1 vertebral body. The thoracic spine has little motion because of the facet joint orientation and added stabilization of the rib cage.
Lumbar nerve roots exit beneath like-numbered pedicles, as in the thoracic spine. The facet joints of the lumbar spine have a more sagittal orientation and allow moderate motion in the sagittal plane while resisting rotation. The transition from the stiff thoracic spine to a mobile lumbar area accounts for the high number of injuries at the thoracolumbar junction.
Mechanics of Vertebral Column Injury
Injuries to the spinal column occur as a result of excessive forces applied to the spine. These forces can cause axial loading, hyperflexion, hyperextension, distraction, rotation, or a combination of forces. Injury to the spinal column can cause spinal instability, which can be defined on either radiographic or clinical grounds. In the acute setting, radiographic features are most commonly used to determine spinal stability (see later).
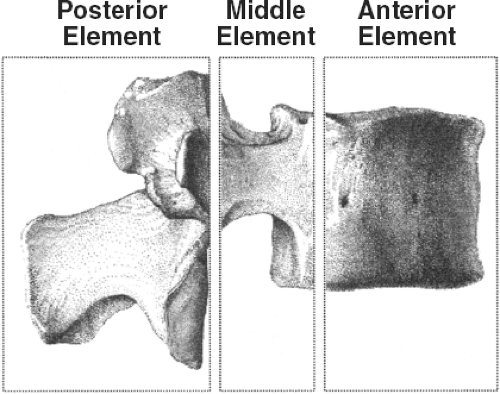
The conceptualization of the spine as a series of support columns provides a framework for our understanding of biomechanical stability. Denis first described the three column model of the spine for thoracolumbar fractures. The anterior column (anterior longitudinal ligament and the anterior two-thirds of the vertebral body and disc), the middle column (posterior third of the vertebral body and disc and the posterior longitudinal ligament), and the posterior column (the facet joints, capsule, ligamentum flavum, and posterior ligaments) describe the main columns of overall biomechanical support (Fig. 25-2). Injuries to two of three columns suggest biomechanical instability.
Spinal cord injuries can be distinct from spinal column injuries. Spinal column injuries are bone or ligamentous disruptions that result in bone fractures or ligamentous instability. The loss of these stabilizing and supporting elements can result in compression and injury of neural elements. The diagnosis of spinal column injury is based on both clinical (pain,
tenderness, or ecchymosis) and radiographic criteria on plain films or tomography. Spinal column injuries can occur without SCI, just as SCI can occur without spinal column fracture.
tenderness, or ecchymosis) and radiographic criteria on plain films or tomography. Spinal column injuries can occur without SCI, just as SCI can occur without spinal column fracture.
The diagnosis of a SCI is made on clinical grounds and supplemented with imaging studies. The level of SCI frequently correlates with the level of spinal column injury. However, SCI can occur without spinal column injury. Spinal cord injury without radiographic abnormality (SCIWORA) tends to happen in the very young or the elderly in whom ligamentous laxity or canal stenosis, respectively, are predisposing factors. This term developed before the era of magnetic resonance imaging (MRI) and retrospectively these cases may have shown imaging abnormality today.
Certain comorbidities can alter the usual biomechanics of the spine and predispose the trauma patient to unusual fracture patterns. Ankylosing spondylitis can lead to fusion across multiple spinal levels, known as “bamboo spine.” This increased rigidity causes the spine to act like a tubular long-bone, with fractures resulting from relatively minor trauma and frequently leading to significant instability. Osteoporosis is found in 38% of women over 75 and is characterized by a decrease in density of normal bone. This decreased density increases risk for fractures from even minor trauma, particularly of the vertebral body. These vertebral compression fractures are rarely associated with neurologic deficit but can lead to progressive kyphosis, ongoing pain, and loss of height.
Prehospital Measures
Initial treatment of patients directed to establish an adequate airway, ventilate the lungs and maintain circulatory support to prevent secondary hypoxic neurologic injury. All patients with a suspected SCI should be immobilized. An estimated 3% to 25% of spinal cord injuries occur after the initial trauma, either in transport or during early resuscitation. A rigid cervical collar alone does not adequately prevent translation in the upper cervical spine, where instability has dire consequences. Use of bilateral sandbags and tape immobilization is more effective in achieving cervical immobilization than any device, especially in conjunction with a rigid collar. When turning is necessary (e.g., active emesis), three members of the treatment team should logroll the patient.
Flat, firm backboards are typically used to facilitate immobilization of the spine but are not optimal in all situations. These boards can lead to skin breakdown over bony prominences. In the rare case of a patient with ankylosing spondylitis, the patient should be transported in the most comfortable position rather than exacerbating spine injury by forcing the spine into a “normal” position.
A scoop stretcher or similar backboard with supportive blocks and straps should be used rather than logrolling to prevent uncontrolled motion. Transport to a definitive treatment center should be the goal, as delays can incur worse outcomes, longer hospitalization, and higher costs. The patient should remain on a backboard until evaluated in the emergency department.
Trauma patients with a mechanism of injury severe enough to cause spinal injury frequently require airway protection. This is discussed in Chapter 3.
Hypovolemic and neurogenic shock can occur in the setting of SCI. Hypotension should be considered first to be from abdominal bleeding, aortic or cardiac injury, or external blood loss before considering neurogenic shock. Neurogenic shock is a diagnosis of exclusion; it is caused by interruption of sympathetic outflow tracts with resultant unopposed vagal tone. Bradycardia is a classic but not always present, as is true for warm, dry skin.
Regardless of cause, shock should be appropriately treated to prevent further ischemic injury to the spinal cord. Treatment consists of crystalloid fluid administration first with vasopressors to maintain adequate blood pressure only once certain that euvolemia is achieved. This is covered in Chapter 5.
Neurologic Evaluation and Physical Examination
At the conclusion of the primary survey, a focused neurologic examination should be performed examining level of consciousness with Glasgow Coma Score (GCS), pupillary size and reaction, lateralizing signs and SCI level.
During the secondary examination, a more detailed neurologic examination, external assessment for spinal tenderness or deformity (e.g., spinous process step-off) and radiologic evaluation guided by the results of the neurologic and physical examinations is performed. Evaluate the mental status, cranial nerves, motor testing, sensory testing, and reflexes to assess global functioning, and repeat this to detect any changes over time.
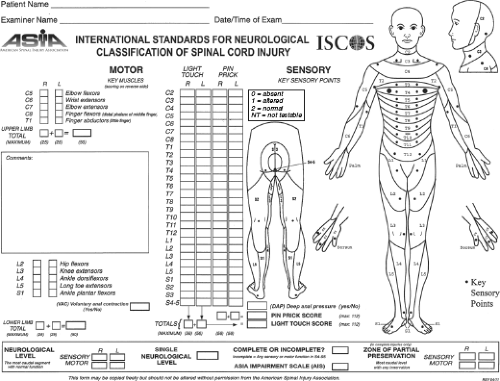
Motor evaluation is performed by asking the patient to move all extremities individually and assessing strength using the American Spinal Injury Association/International Medical Society of Paraplegia (ASIA/IMSOP) protocol. Normal strength is graded 5/5, with mild weakness graded as 4/5. Grades 4 and 5 are determined based on amount resistance overcome and grade 4 is the only grade that is sometimes subdivided into three divisions to further clarify amount of power (−4, 4, 4+). The ability to fully overcome gravity through a full range of motion, but not overcome any applied resistance by the examiner, is graded 3/5. Movement throughout a range of motion but unable to overcome gravity is graded 2/5. Flicker motion of muscles is 1/5 and no movement is 0/5. Patients with C5 levels of spinal cord function will be able to flex only their arms and should not be confused with pathologic flexor posturing.
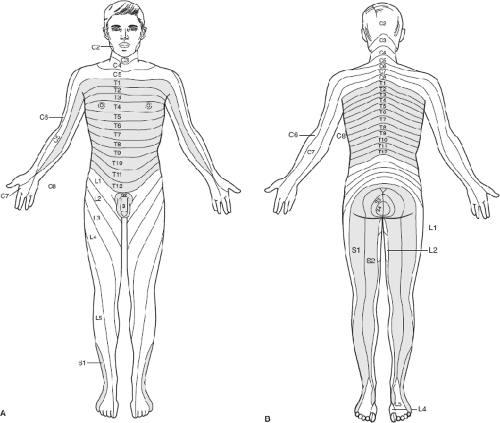
Sensory testing of light touch and pain perception can aid determining radiographic target for imaging (Fig. 25-3). Useful examination tools include a cotton swab broken in half or safety pins. Pay close attention to the level of sensation and asymmetry.
Reflex testing is performed at the biceps (C5), triceps (C7), brachioradialis, knee (L4), and ankle areas (S1). Special reflex testing includes jaw jerk, deltoid (C5), pectoral, superficial abdominal (T9–T12), bulbo- or cliterocavernositis (S3–S4), anal wink (S5), and Babinski. The extremity reflexes are graded on a scale of 0 to 4, where 0 represents absent reflex activity, 1 is decreased reflex activity, 2 is normal reflex activity, 3 represents increased reflex activity, and 4 is grossly exaggerated reflex activity with sustained clonus. An exaggerated jaw jerk indicates injury at or above the pons. Deltoid and pectoral reflexes are usually associated with significant hyperreflexia. Bulbo- or cliterocavernosis reflexes may be retained in complete injury, but lost during spinal shock. Their reappearance may indicate that a period of spinal shock has ended. Babinski responses are recorded as present or absent. The presence of UMN findings (hyperreflexia, loss of superficial abdominal reflexes, Babinski responses) indicates spinal cord or conus medullaris injury. Decreased reflexes imply LMN (cauda equina and
nerve root) injury. Weakness, sensory loss, and bladder, bowel, and sexual dysfunction can be seen with either UMN or LMN injuries. Of note, acute UMN injuries often present with reflex stunning or areflexia, mimicking a LMN injury, and may last for 24 to 48 hours.
nerve root) injury. Weakness, sensory loss, and bladder, bowel, and sexual dysfunction can be seen with either UMN or LMN injuries. Of note, acute UMN injuries often present with reflex stunning or areflexia, mimicking a LMN injury, and may last for 24 to 48 hours.
The most sensitive predictor of prognosis is the severity of neurologic injury as characterized by level and completeness of deficit. The neurologic sensory levels are determined and recorded based on the lowest segment with normal sensory and full motor function bilaterally. Complete injury is seen in the patient without sensory or motor function below the level of neurologic injury, including loss of perianal sensation and sphincter function. The patient with incomplete injury has partial preservation of sensory or motor function below the level of neurologic injury, with preservation of perianal sensation and motor function called “sacral sparing”; the latter does not include an intact bulbo/clitorocavernosus reflex which can be present in complete injuries.
In the acute setting, the use of specific terms denoting neurologic level is preferable to more general terms (e.g., paraparesis, quadriplegia). The ASIA impairment scale, consisting of a five-point grading scale demarcated A–E (Fig. 25-4), is as follows:
Complete loss of sensory and motor function (including the sacral area) below the neurologic level. Even patients with ASIA A scores can improve neurologically, although few of these patients will achieve functional motor recovery.
Incomplete injury, whereby sensory function is preserved below the level of neurologic injury including the sacral area.
Incomplete injury with motor function preserved below the neurologic level and most preserved groups exhibiting strength of <3 (gravity).
Incomplete injury with motor function preserved below the neurologic level and most preserved groups exhibiting >3 strength.
Normal sensory and motor examination.
Spinal cord injuries can often present with characteristic constellations of findings indicating the region of the spinal cord affected and reflecting the mechanism of injury.
Posterior cord injury with loss of position sense resulting from injury to the posterior columns is rarely traumatic. This injury is usually related to vitamin deficiencies and infections (e.g., syphilis). The patients develop a loss of position and vibratory sense.
Central cord injury is common in the cervical spine of patients who experience excessive motion in the sagittal plane, particularly in those with pre-existing stenosis of the spinal canal. These injuries are thought to result from vascular compromise to the central areas of the spinal cord. The hallmark features are hand weakness that is more pronounced than lower extremity weakness, bladder dysfunction, and variable degrees of sensory loss below the lesion.
Anterior cord injury often occurs in the setting of vascular compromise and suggests anterior spinal artery occlusion. Infarction of the spinal cord results in loss of all motor and sensory function other than proprioception.
Brown-Sequard syndrome is rarely seen in its pure form and is a result of injury to one-half of the spinal cord. It is characterized by loss of ipsilateral motor function, ipsilateral position sense, and contralateral loss of pain and temperature sensation two to three segments below the level of injury.
Conus medullaris and cauda equina syndromes occur at the thoracolumbar levels and result in varying degrees of weakness, sensory loss, bladder, bowel, and sexual dysfunction. Conus injuries affect UMNs, which may precipitate hyperreflexia. Conus injuries may also cause reflex stunning with the loss of the bulbocavernosus reflex. The cauda equina syndrome typically results from a compressive lesion below the level of the spinal cord with resultant bowel/bladder dysfunction, saddle paresthesias, and lower extremity weakness. This represents one of the few operative emergencies in spinal trauma; compression should be alleviated as soon as safely possible to attain maximal recovery and prevent further deterioration.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree