Chapter 7 Safety and Quality Assessment in the Pediatric Intensive Care Unit
A Brief Consideration of the Relationship Between Safety and Quality
Many similarities exist between safety and QI. As a result, there is potential confusion between the two domains. Are they the same? Is safety really applied QI? The Institute of Medicine weighed in on this discussion by identifying safety as a component of quality in the report Crossing the Quality Chasm.1 Based on this report, safety is a prerequisite to achieving quality. That is, it is impossible to achieve true quality without improving safety. Others who argue that attention to other aspects of quality beyond safety is critical have confirmed this observation.2 For the pediatric critical care provider, the important point is that safety is a necessary prerequisite for quality, but improving safety is insufficient to achieve quality.
State of Safety and Quality in Pediatric Intensive Care Units
The Institute of Medicine’s report, To Err is Human, was the first widely recognized publication to identify the scope of preventable medical harm.3 In response, patient safety and quality was placed on the radar screen of consumers, policy makers, and providers. Perhaps the most visible response from these groups is the focus on measurement as an attempt to drive improvement. Inherent to this is the recognition that adoption and public reporting of performance measures is a necessary (though not sufficient) step to achieving a high-quality health care system.
In PICUs, the increased focus on safety and improvement is evident in three major developments. First, the National Quality Forum endorsed the adoption of and public reporting of six PICU-specific performance measures in May 2008 (Table 7-1).4 These measures were created based on the recognition that performance measures designed for adult populations may not be appropriate for application to the pediatric populations and settings.5,6 For many PICUs, measurement and reporting of these endorsed measures is voluntary. However, formal endorsement by the National Quality Forum makes these measures “fair game” for evaluation by payers and accrediting bodies such as The Joint Commission.
Table 7–1 Endorsed Pediatric Intensive Care Unit Measures
| Measure | Description |
|---|---|
| PICU standardized mortality ratio | The ratio of actual deaths over predicted deaths for PICU patients, adjusted using an accepted risk of mortality tool. |
| PICU severity-adjusted length of stay | The number of days between PICU admission and PICU discharge for PICU patients, adjusted using an accepted risk of mortality tool. |
| PICU rate of unplanned readmissions within 24 hours of PICU discharge | The total number of patients requiring unscheduled readmission to the ICU within 24 hours of discharge or transfer, over the number of discharges and transfers. |
| Review of PICU unplanned readmissions within 24 hours of PICU discharge | Periodic clinical review of unplanned readmissions to the PICU that occurred within 24 hours of discharge or transfer from the PICU. |
| PICU pain assessment on admission | Percentage of PICU patients receiving pain assessment on admission. |
| PICU periodic pain assessment | Percentage of PICU patients receiving periodic pain assessment while in the PICU. |
A second development illustrating the importance of QI and patient safety to PICUs is the national catheter-associated bloodstream infection (CA-BSI) team collaborative.7 This national initiative is focused on applying bundle tools to reduce cather-associated bloodstream infections. Based on data from 29 teams, applying the bundle recommended by the collaborative prevents 22 CA-BSI infections and saves two lives and $750,000 each month.
A third manifestation of the increased importance of QI and patient safety in PICUs is the American Board of Pediatric’s requirements for Maintenance of Certification. Intensivists interested in maintaining their credentialing must now demonstrate that they meet four conditions: professional standing, lifelong learning, cognitive expertise, and performance in practice.8 A component of meeting these conditions is the active participation in an improvement project. Of note, active participation in the previously mentioned CA-BSI project will meet this condition.
Consistent with each of these three developments, multiple authors have concluded that physician leadership and participation are crucial to the success of QI and patient safety efforts.9,10 Unfortunately, a 2003 survey among U.S. physicians showed that they infrequently participate in improvement efforts, they don’t routinely use data for assessment of their performance, and are reluctant to share those data.11 Specific to the PICU environment, a more recent survey of pediatric critical care providers demonstrated that responders had poor knowledge of national quality and safety initiatives and similarly poor compliance with these national initiatives.12 These data suggest that significant gaps in knowledge and practice of safety and quality activities by physicians caring for critically ill children persist.
Fundamentals of Quality Improvement and Patient Safety: Systems Thinking
To understand patient safety and quality in health care, one first must recognize the importance of systems to the way care is delivered. The Institute of Medicine, drawing from James Reason’s studies of errors, defines a system as “a set of interdependent elements interacting to achieve a common aim.” One model of systems in health care consists of five interaction components: people (1) use tools and technologies (2) to perform tasks (3) within an enviroment (4) in the context of an organization (5).13 Each of these five components interacts with the others to yield the emergent properties (greater than the sum of the parts) of safety and quality.
Several essential implications follow from this model. First, no matter how safe any component is (ie, an intensivist who never makes mistakes), it is the five components and their interactions that determine if care is safe and of high quality. Second, if you change any of these components, it will have impact on the other components and their interactions. This is illustrated through the routine practice of cannulation for extracorporeal membrane oxygenation (ECMO) in the PICU. Merely changing the environment from the PICU to the hospital parking lot would have dramatic implications for the people, their tasks, the tools, and the organization’s culture and liability. A third implication of this model is that changes to one or more of the five components will inevitably impact their emergent properties of safety and quality. This is illustrated by the growing literature that suggests that “safety technologies” may actually cause errors and harm.14–19 Thus for critical care providers, understanding the role of systems in the work done in an intensive care unit (ICU) is crucial to improving quality or reducing harm.
Additional characteristics of systems that are important to intensivists are their complex adaptive nature20 and the concept of tight coupling.21 A complex adaptive system is one with several characteristics. First, complex adaptive systems have multiple similar agents that are autonomous entities that observe and act on their environment (such as PICU providers). More important, these multiple agents are adaptive, allowing for a high degree of resilience to system changes. The complex adaptive nature of the PICU is illustrated by sudden, unpredicted events such as codes, an unplanned extubation, or even multiple simultaneous admissions. In each of these scenarios, the future was unpredictable, the response was adaptive, and order is emergent rather than predetermined.
Quality Improvement and Value
Quality has been defined as “the degree to which health services for individuals and populations increase the likelihood of desired health outcomes and are consistent with current professional knowledge.”22 This definition, which comes from the Institute of Medicine, draws from the work of Donabedian.23 In his work, quality was defined in the context of structure, process, and outcomes. In other words, to measure quality, you should consider the structure or capacities of health care, the process or interactions between patients and care providers, and the outcomes or evidence of changes in a patient’s health condition. Ideally, considerations of quality should consider all three components.
The Institute of Medicine has identified six essential domains for achieving health care quality.1 These areas include safety, effectiveness, patient-centeredness, timeliness, efficiency, and equity. Based on these and Donabedian’s components of quality, efforts to improve quality should consider improvement of process, structure, and/or outcome focused on one of the six areas identified by the Institute of Medicine. The first of these domains, safety, is discussed in depth later in this chapter. These initiatives are intended to identify, analyze, and reduce risks that contribute to medical errors and injuries.24 The CA-BSI bundle project discussed previously is an example of QI leading to improved safety.25
The second domain, effectiveness, implies providing services based on the best available scientific knowledge in order to achieve the best outcome. Publication and implementation of clinical practice guidelines seek to decrease unwarranted variability in care resulting in improved outcomes. A practical example of the latter is the 2002 American College of Critical Care Medicine guidelines for hemodynamic support of pediatric and neonatal patients in septic shock. Studies have provided evidence that these guidelines are useful and effective, though evidence that clinical guidelines are often violated 26,27 indicates that promoting their use will remain an additional challenge.
Patient-centeredness describes the provision of care in a manner that is respectful of and responsive to individual patient preferences, needs, and values. In the PICU, many children may be unable to express their desires. Therefore, the experience of their parents is recognized as being fundamental to defining this aspect of quality. Applying this perspective, the principle of family-centered care mandates incorporation of parents in daily aspects of care. Measuring patient and family satisfaction may be invaluable to improving this aspect of PICU quality. One strategy shown to have a positive impact on satisfaction is the presence and involvement of parents on rounds.28
Efficiency in the PICU could be measured by the ability to achieve adequate outcomes while keeping resource utilization appropriate, thus minimizing cost. Length of stay (LOS) is a common meaure of resource utilization in the PICU, and reduction is one potential method of reducing cost and improving efficiency. In adult ICUs, consistent identification of daily rounding goals during multidisciplinary patient care rounds leads to reduced LOS with improved staff understanding of what is needed to perform care.29 It is important to note that improvement efforts targeted solely at efficiency may have unintended but foreseeable adverse effects on safety and satisfaction. This could be seen if efforts to reduce LOS lead to premature discharge with subsequent readmission. Thus, improvement efforts may need to view how they influence all six of the domains.
The final domain of quality is equity. Essentially, the quality of care provided in the PICU should be independent of characteristics such as gender, ethnicity, geographic location, and socioeconomic status.30 Studies have documented disparities in the allocation of resources to critically ill adults related to race and insurance status.31 In one multicenter study of three PICUs, the authors concluded that risk-adjusted mortality and resource utilization for critically ill children did not differ according to race, gender, or insurance status. However, uninsured children had significantly greater physiologic derangement at time of PICU admission.32 More research into the issue of equity in pediatric critical care may be necessary before the community concludes there is no room for improvement. Even if admission criteria are free of inequity, are there comparable resources available for effective long-term care?
A discussion of the definition of quality should include potential shifts in thinking. Of note, there is literature suggesting that beyond quality, the issue of value is important to health care. In this context, value is defined as a measure of quality per unit cost.33 This can be illustrated by considering what automobile the reader drives. Whether an entry-level compact car or a “loaded” luxury vehicle, for each consumer there is some determination of both the quality of the vehicle and whether that quality is worth the cost. Although robust measures of quality and true costs remain elusive in health care, critical care providers could improve value to patients by improving quality, reducing cost, or both.
Quality Improvement Methods
QI seeks to improve the quality of care. To improve care, you must first define the process of care that needs improvement. Ideally, a goal is set to define what is desired in terms of the outputs of the process. Then data are obtained to understand the process, and finally interventions are made with follow-up measurement to assess the change, positive or negative.34
Ideally, these changes and reevaluations are done in an iterative manner. This method has been labeled as the “PDSA (Plan, Do, Study, Act) Cycle.”34 The Institute for Healthcare Improvement (www.IHI.org) has advocated use of a PDSA method over a short period to create what it calls “rapid cycle improvement.” With either model, changes often are introduced quickly and sometimes multiple changes are introduced simultaneously. This method has evoked pushback from some physicians because of an apparent lack of scientific and statistical rigor. From a QI standpoint, many improvements are achieved without the need for meeting a given P value. Ironically, the resistance to QI methodology because of lack of statistical rigor is inconsistent with much clinical practice in the PICU. There does not exist a standard of care that every intervention performed in resuscitating a patient be accompanied by evaluation for statistical significance. In fact, resuscitations may involve multiple interventions (endotracheal intubation, chest compressions, administration of medications) in a rapidly sequential or simultaneous manner. With a successful resuscitation, an intensivist may be unable to identify which of numerous interventions was responsible for the improvement. Arguably, if improvement occurred, neither the patient nor the family necessarily cares which intervention resulted in the positive change. Such is the QI mindset. If a given intervention can be identified and causation established for a specific improvement, this information may be applied to different settings. However, the goal is improvement, and improvement without clear identification of the causative factor remains an improvement.
Variation and Display of Data over Time
If an intensivist watches a physiologic monitor for any length of time, it is normal to view variability in heart rate and other vital signs. This reflects the dynamic nature of physiologic systems and processes. Similarly, health care processes vary within certain ranges under normal circumstances. Reacting to changes within normal variation may lead to interventions that increase variation rather than reducing it.35 However, the range within which the variation is occurring may be outside the desired goal. Thus improvement may address the amount of variation associated with an existing system and/or fundamental redesign of the system.
Again, understanding the normal variation in a process is critical. The PICU provides physiologic illustrations of this concept. A patient who is doing reasonably well in the PICU has a normal range of heart rate variability, and loss of heart rate variability has been associated with increased risk of death in certain populations.36 Similarly, a relatively well patient in the PICU who acutely develops either tachycardia or bradycardia merits evaluation for new or worsened pathology. In this case, the heart rate variation that normally occurs does so within certain parameters. This variation is called common cause variation in the QI literature. When the variation crosses either the upper parameter (tachycardia) or lower parameter (bradycardia), then something is amiss. The same holds true for processes and systems within health care. Variation that crosses certain thresholds or is an abnormal outlier is called special cause variation.
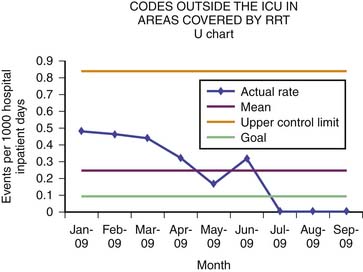
Plotting data over time allows for an understanding of this variation, normal or abnormal, in data. When data points (eg, LOS) are placed on a chart with time (eg, in days) plotted on the ordinate, this is called a run chart. Control charts, or statistical process control charts, also plot data over time. However, control limits are added that help define the limits of normal variation. Control limits, first described by Walter Shewart in the 1920s, are calculated in a variety of statistical manners, in part depending on the type of control chart. The type and distribution of data determine the choice of control charts37; methods for choosing a control chart are beyond the scope of this chapter. At the most basic limit, control levels are set at three times the standard deviation of the data, around the line of central tendency.
In general, when data exist within the control limits, a process is said to be in control. Data that either extend beyond the control limits or demonstrate one of several patterns suggest either an unstable process or a process that is responding to a change. This change may be an intentional effort to alter a process or may represent the effect of an unknown cause. Returning to the heart rate analogy, a patient who becomes bradycardic from hypoxia would demonstrate deviation of the normal heart rate variation in response to the special cause (hypoxia). Correction of the hypoxia ideally returns the heart rate (process) to its normal range of variation. An example of a control chart is displayed in Figure 7-1. Another example of process variation over time in the PICU is rates of CA-BSIs. For years, CA-BSIs were viewed as an unpreventable cost of PICU and adult ICU care. However, the systematic introduction of central line insertion bundles has resulted in transformative improvement in rates of CA-BSIs. With the addition of central line maintenance bundles, ICUs have reached sustained CA-BSI rates of zero. Analagous to the rate of codes outside an ICU with the introduction of a rapid respose team (see Figure 7-1), plots of CA-BSI rates over time in control charts similarly allow intensivists to understand the relationship between improvement efforts and infection rates.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree