Chapter 50 Noninvasive Ventilation
Concepts and Practice
Historical Perspective
Dalziel, in 1832, reported the use of a bellows-operated box with a seal around the neck or shoulders to provide artificial respiration to a drowned seaman.1 In 1867, Woillez designed the first workable noninvasive negative-pressure ventilator, which was operated manually.2 Doe, in 1989 described a box used for resuscitating newborns.3 Drinker developed the first tank ventilator in 1928 that was subsequently used with great clinical value in patients with poliomyelitis.4 Negative-pressure ventilation was introduced for use with neonates in the 1960s.5,6 In 1953, Lassen reported that positive-pressure ventilation administered using an endotracheal tube or a tracheostomy was more successful that negative-pressure ventilation in treating patients with poliomyelitis.7 Major technologic advances in the design of positive-pressure ventilators led to the marked decrease in negative-pressure ventilation. Noninvasive positive-pressure ventilation by facemask was first used by Barach et al.8 for the treatment of hypoxemic respiratory failure secondary to acute pulmonary edema. Gregory et al.,9 in 1971, reported that constant positive airway pressure (CPAP) through nasal prongs was effective in improving oxygenation in neonates with hyaline membrane disease. Vidyasagar and Chernick showed that constant negative pressure applied about the chest and abdomen was as effective as CPAP in improving oxygenation in neonates with hyaline membrane disease.10 Despite these early reports, noninvasive ventilation did not become popular until more recently. There is a renewed interest in noninvasive ventilation coinciding with technologic advances in the manufacture and design of noninvasive ventilators. NIV through a mask for neuromuscular disorders was pioneered in the 1980s by Rideau et al.11 and subsequently by Bach et al.12
Short-Term Noninvasive Ventilation
The indications for use of NIV in acute care and critical care situations are given in Box 50-1. The selection guidelines are given in Box 50-2. The first step is to determine whether a patient has a reversible cause of respiratory failure. The second step is to determine whether the patient needs positive pressure support to maintain gas exchange. Before attempting NIV in acute respiratory failure, the clinician must answer the following questions:
Box 50–2 Selection Guidelines for Short-Term NIV
Figure 50-1 shows the algorithm to be followed for initiation of NIV in acute respiratory failure. If NIV is used in acute situations, there should be a determination within 1 to 3 hours whether the patient has improved. Signs of success and failure are given in Box 50-3. A good response to NIV is indicated by: (1) reduction in respiratory rate, (2) reduction in work of breathing, (3) reduction in dyspnea, (4) improvement in pH, (5) improvement in oxygenation, and (6) reduction in PaCO2. Additionally, there may be hemodynamic effects such as a reduction in heart rate, improved blood pressures, and perfusion. Generally, for short-term use, NIV is used continuously until the patient improves or fails NIV. The goals of short-term NIV are given in Box 50-4.
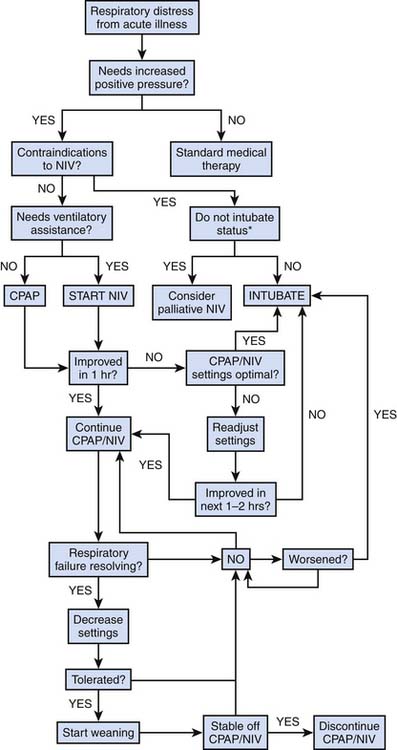
Figure 50–1 Algorithm for initiation and weaning of short-term continuous positive airway pressure and NIV.
Box 50–3 Signs of Success and Failure Within 1–2 Hours of Application of NIV for Short-Term NIV
Adult Studies on the Short-Term Use of Noninvasive Ventilation
Adult studies have shown that NIV can be used in hypoxemic respiratory failure (PaO2/fraction of inspired oxygen [FiO2] ratio <300) with bilateral parenchymal disease to prevent endotracheal intubation. Ferrer et al. showed that NIV reduced the intubation rate from 52% to 25% with a reduction in intensive care unit (ICU) mortality rate from 39% to 18%.13 But, this finding must be tempered by studies that show that NIV may not reduce the need for endotracheal intubation.14,15 CPAP, not strictly a form of ventilatory assistance, was described by Barach et al.8 for the treatment of acute cardiogenic pulmonary edema. Since then, several studies have demonstrated that both CPAP and NIV can decrease the rate of intubation, improve work of breathing and improve gas exchange.16–18 In adults with acute exacerbations of chronic obstructive pulmonary disease, NIV has been shown to improve both short-term and long-term outcomes.19–21 It is reasonable to expect a similar response to acute asthma because many of the pathophysiologic features are similar. Uncontrolled studies and one randomized controlled study showed improvement in patients having an acute asthma attack.22–24 It is desirable to reduce the probability of nosocomial infections in immunocompromised patients. Therefore, it is appealing to apply NIV to avoid endotracheal intubation in these patients. Adult studies have shown that NIV can reduce the rate of intubation and may improve short term mortality.25–27
Adult studies have shown that respiratory insufficiency that develops postoperatively in patients can be successfully treated with NIV. NIV reduces the rate of intubation and is more effective than CPAP or chest physiotherapy.28,29 In patients after lung resection surgery, NIV reduced the rate of intubation and mortality compared with conventional therapy.30 Children with restrictive chest diseases who develop respiratory failure after surgery such as spinal fusion are good candidates for NIV if they develop postoperative respiratory failure provided they do not have any other contraindications.
Endotracheal intubation and invasive mechanical ventilation are associated with complications including ventilator-associated pneumonia, ventilator-induced lung injury, and airway trauma. To minimize these complications, it is desirable to extubate the patient as quickly as possible. Generally, extubation coincides with the end of weaning (i.e., the patient is not placed on any form of positive pressure support postextubation). In some patients, who take a long time to wean, but require fairly low ventilatory assistance, it is possible to extubate them to NIV. Theoretically, it would reduce the incidence of complications associated with endotracheal intubation and invasive mechanical ventilation. Udwadia et al. were among the first to test this paradigm in 22 adult patients who were successfully stabilized on NIV after extubation.31 Three adult studies have demonstrated that the use of NIV resulted in a reduction in the duration of mechanical ventilation, a reduction in the incidence of nosocomial pneumonia, and a reduction in the duration of hospital stay.32–34 Similar pediatric studies are lacking. NIV to facilitate extubation should be carried out only if the patient meets the following criteria: (1) is awake and alert, (2) has intact bulbar function with a preserved cough reflex, (3) has minimal airway secretion, (4) is able to breathe spontaneously, (5) has stable hemodynamic status, (6) does not have gastric distension, and (7) has a requirement for 40% or less supplemental oxygen. Recently, some adult studies have examined the use of NIV for postextubation respiratory failure (i.e., respiratory failure that develops after extubation on complete spontaneous breathing). The rationale for the use of NIV in this circumstance is the avoidance of endotracheal intubation. In at least one study in adults, this approach was shown to increase the time from respiratory failure to intubation with an increase in mortality rate.35 It is difficult to extrapolate from adult studies to pediatrics. It is possible that some children may benefit from the institution of NIV for postextubation respiratory failure.
Pediatric and Neonatal Studies
In 1981, Sullivan et al.36 first demonstrated that nasal CPAP was effective in reversing obstructive sleep apnea in four adults and one teenager. Guilleminault et al.,37 in 1986, reported that nasal CPAP reversed or reduced obstructive sleep apnea in some children. There were problems related to poor cooperation from parents and difficulty in preventing leaks around the nasal mask. Since the first report, several studies have shown that nasal CPAP was effective in obstructive sleep apnea in infants and children.37–42 In 1995, Guilleminault et al.43 reported that nasal CPAP was successful in 70 of 72 infants with sleep-disordered breathing. In many instances, it provided an interim solution while allowing the patient to grow and postponing surgery.
Patients in a fairly wide age range appear to tolerate NIV therapy in the acute setting, provided they are adequately monitored and sedated. In 1993, Akingbola et al.44 published a case report describing effective NPPV therapy in two pediatric patients with acute respiratory distress. Since that time, NIV has been applied to pediatric patients with a variety of respiratory disorders associated with acute hypoxemic respiratory failure, including pneumonia, pulmonary edema, postoperative respiratory decompensation in sleep apnea syndrome, status asthmaticus, spinal muscular atrophy, and end-stage cystic fibrosis.45–51
Padman et al.52 published a preliminary report on 15 patients ages 4 to 21 years who had respiratory failure because of cystic fibrosis (four patients) and neuromuscular disease (11 patients). In 14 patients, the placement of an artificial airway was avoided. They observed significant improvement in hospital days, respiratory rate, heart rate, serum bicarbonate, arterial carbon dioxide, dyspnea, activity tolerance, and quality of sleep. In 1995, Fortenberry et al. reported a retrospective study on the efficacy and complications of biphasic positive airway pressure (Bi-PAP) in 28 children with acute hypoxemic respiratory insufficiency.47 Bi-PAP significantly decreased respiratory rate and improved both oxygenation and ventilation. The use of Bi-PAP decreased hospitalization rate and increased patient comfort. Only three of 28 patients required intubation or reintubation. Padman et al. conducted a prospective study in 34 patients with impending failure all of whom required airway or oxygenation/ventilation support and required admission to the pediatric ICU.50 A decrease in respiratory rate, heart rate, and dyspnea score, and an improvement in oxygenation were noted in more than 90% of patients studied. The frequency of intubation in these patients was only 8%. Birnkrant et al.51 reported their experience with Bi-PAP in six patients with spinal muscular atrophy and three patients with other causes of respiratory failure. This uncontrolled study showed that in these patients noninvasive positive-pressure ventilation facilitated extubation. Teague et al.53 reported that NIV treatment acutely improved oxygenation and reduced cardiorespiratory distress in 19 of 26 patients. This group of “NIV responders” had significantly shorter lengths of stay in both the ICU and hospital. However, the seven nonresponders required endotracheal intubation as respiratory distress progressed despite sedation. Teague et al.53 also showed that NIV improves gas exchange in children with upper airway obstruction In a prospective, randomized, controlled trial of NIV in children with acute respiratory failure, Yan et al.54 showed that NIV improved hypoxemia and the signs and symptoms of acute respiratory failure and reduced the rate of endotracheal intubation. Thill et al.,55 in a randomized, crossover study in children with lower airway obstruction, showed that NIV decreased signs of work of breathing such as respiratory rate, accessory muscle use, and dyspnea as compared with standard therapy with no serious associated morbidity. Pancera et al.56 recently published their experience with NIV in immunocompromised pediatric patients. NIV as the first-line therapy was compared to invasive mechanical ventilation. Seventy-five percent of the patients treated with NIV did not require endotracheal intubation showing that NIV is a viable first-line therapy for respiratory failure in immunocompromised patients for preventing endotracheal intubation.56 More recently, NIV has been suggested as an alternative to endotracheal intubation for the perioperative management of scoliosis correction in patients with muscular dystrophy.57
Interfaces
A properly fitting facial appliance is essential for the optimal application of NIV. There are currently several devices in use: (1) oral-nasal mask, (2) nasal mask, (3) total face mask, (4) Adam’s circuit, (5) head hood, (6) nasal prongs, and (7) mouthpieces. A correctly sized interface minimizes leaks, improves effectiveness of positive pressure support, and improves comfort.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








