Chapter 14 Pediatric Transport
Shifting the Paradigm to Improve Patient Outcome
Along with the regionalization of pediatric emergency and critical care centers has come the growth of interfacility transport programs, allowing geographic expansion of tertiary medical care. Eighty-nine percent of pediatric emergency department (ED) visits occur in nonpediatric EDs, where the extent of illness or injury is assessed and initial stabilization is provided.1 Most community hospitals do not have the personnel, space, or facilities to provide critical care to infants or children beyond the period of initial stabilization, necessitating transfer to a tertiary facility. In transport, children are subjected to a high-risk environment with limited resources and monitoring capabilities. The goal during transport should be to provide care commensurate with the degree of illness severity in a safe and effective manner, minimizing the risk of deterioration and unplanned events before transport and en route. Little research exists to support the choices about mode of travel or makeup of the transferring team that are made every time a child is transferred to a tertiary facility.
Improvements in critical care are incremental: There are no miracle drugs or technologies. The major improvements in care in the last decade involve early, aggressive administration of simple therapies: timely initiation of resuscitation fluids, inotropes via peripheral intravenous line, and antibiotic therapy can improve outcomes.2,3 If appropriate resuscitation waits until the child arrives in the pediatric intensive care unit (PICU), the benefits of early, aggressive action are likely to be lost. Goal-directed therapy must begin before and continue during transport for the benefits noted in these studies to occur. Significant barriers to realizing this ideal exist.
In this chapter we will briefly discuss the barriers that have stifled progress. Information about appropriate vehicles, medication, and equipment for transport is summarized elsewhere, in the American Academy of Pediatrics (AAP) Guidelines for Air and Ground Transport of Neonatal and Pediatric Patients.4 This chapter is designed to challenge the pediatric intensivist, whose patient population is largely derived from transport, with the important concept that a well designed and staffed pediatric critical care transport system can have a dramatic impact on patient outcomes, and deserves great attention from pediatric intensivists.
The Problem: An Adult-Oriented Retrieval System Focused on Rapid Movement
Emergency medical services (EMS) and regional flight teams are focused on the major causes of mortality in the adult population, such as myocardial infarction and trauma, for which rapid transfer to a center that can provide definitive care is an important determinant of outcome.5 Adult-oriented ED and EMS services do not provide ideal care for children. Still, multidisciplinary teams transport the majority of critically ill children. Many argue that pediatric specialized transport systems are not necessary, for the reasons given in Box 14-1.
Box 14–1 Arguments Against and for Use of Specialized Pediatric Transport Teams
With the support of other interested bodies, the American Academy of Pediatrics recently issued a policy statement detailing the recommended pediatric equipment for ambulances.2 It is not known what percentage of ambulances are adequately equipped, but two independent studies reported that as recently as 2003, only 6% of emergency rooms were appropriately equipped to care for children. Items frequently not available included laryngeal mask airways and infant and neonatal equipment.6
Limited pediatric training coupled with limited exposure to pediatric patients may hamper the ability of EMS providers to respond appropriately to pediatric emergencies. In 2000, nationally registered paramedics received a median 358 total hours of instruction, less than 5% of which were dedicated to pediatrics. Moreover, most paramedics in this study were not required to take pediatric continuing medical education (CME) training.7 Without repeated reinforcement, cognitive and interventional skills deteriorate over time. Fewer than 10% of all EMS runs nationwide are for infants and children, and a small percentage of these involve advanced life support (ALS) or critical care.8,9 Babl et al.10 demonstrated that in a program with 50 active ALS providers, each provider is expected to have one pediatric bag-valve-mask (BVM) case every 1.7 years, one pediatric intubation every 3.3 years, and one intraosseus cannulation every 6.7 years. Su et al.11 demonstrated that the knowledge acquired in didactic sessions deteriorates rapidly over a 6-month period. Henderson12 also demonstrated that the ability of a provider to intubate or provide BVM ventilation for a child deteriorates significantly over the course of 6 months.
Underutilization of an acquired skill can lead to a decrement in skill level and a fear-related aversion to performing the procedure. With any given scenario in the EMS setting, adult patients are more likely to receive an appropriate intervention compared with a child having the same problem.13,14 Prehospital care providers are reluctant to attempt intubation, even when it is clearly indicated. Aijian et al. examined a population of pediatric patients who had suffered a prehospital cardiopulmonary arrest and determined that endotracheal intubation was attempted only 68% of the time, with a success rate of only 64%.15 In patients younger than 1 year, endotracheal intubation was attempted only 38% of the time, with a success rate of only 50%.15 Multiple investigators have documented a decrease in the percent of successful intubations in children compared with adult patients, both in ground EMS systems and air ambulance systems.16–19
Studies of pediatric trauma victims make it clear that prehospital providers could do a better job with children. Children were twice as likely to die of trauma in the field compared with adults, which was attributed to the lack of pediatric training.5,8,20 Ramenofsky et al. determined that 53 of 100 deceased pediatric trauma victims in their study could have been salvaged given an optimally functioning emergency medical system and that in 79% of the potentially salvageable cases, mortality was associated with prehospital iatrogenic or secondary insults.9
Referring hospitals that lack pediatric expertise may create suboptimal situations prior to transport. Esposito et al. found that frequent errors occur in ED management of pediatric trauma, leading to preventable mortality of approximately 9%.21 In addition, they reported a 64% error rate in the management of children, including gross violations of basic trauma care.21 Han et al.22 found that resuscitation practice in a community ED was consistent with American College of Critical Care Medicine-Pediatric Advanced Life Support (ACCM-PALS) guidelines in only 30% of children who presented with septic shock. Athey et al.23 found that nearly 10% of all U.S. hospitals without pediatric intensive care facilities admit critically ill and injured children, and that 7% of these hospitals routinely admit these children to adult intensive care units rather than transferring the children to a more appropriate facility. Of the facilities that keep children, few have protocols for obtaining pediatric consultation for emergencies, and most did not have appropriate-sized equipment to care for children.23 Those referring hospitals that do transport children to pediatric facilities are often inadequately equipped to care for children or unfamiliar with established guidelines and protocols and, as a result, may be in a rush to send children, sacrificing stabilization and eschewing transport by a more experienced team in the interests of saving time. When facilities and physicians lack insight about their ability to care for children, requests for transfer may come too late, after irreparable organ damage has already occurred.
Critical Pediatric Physiology Relevant to Transport Medicine
Peripheral airway resistance in children younger than 5 years is approximately four times higher than in adults or older children, in whom the upper airway is the major contributor to airflow resistance.24 Because of this, young children are more likely to have lower airway obstructive disease and less likely to respond to airway positioning, an intervention which is commonly used by paramedics to defer intubation in adults.
Infants and small children have more compliant chest walls with low elastic recoil compared with older children and adults, increasing the risk of lung collapse.25 In infants and small children, muscular effort is required to stabilize the chest wall, and a portion of the force of contraction of the diaphragm is wasted in distorting the rib cage.26 This mechanical disadvantage leads to increased energy expenditure, and increases the likelihood that infants with lung disease may fatigue and stop breathing.27 Gastric distension can further decrease the efficiency of the diaphragm in children and should be prevented or treated with a nasogastric tube. Positive pressure breathing applied early in the disease process can stop the progression of atelectasis and respiratory failure.
Functional residual capacity is only slightly higher than critical closing volume in infants and small children, leading to alveolar collapse much earlier in the course of respiratory failure. Lung growth appears to involve both an increase in the number of alveoli and an increase in the size of alveolar spaces,28 which may also predispose the infant lung, with its smaller alveoli, to collapse. In addition, the adult lung contains anatomic channels that allow ventilation distal to an obstructed airway, also known as collateral ventilation; the absence of these pathways in young children further increases the risk for atelectasis.29 The diffusing capacity across the alveolar-capillary membrane in a child is only about one third that of an adult, making gas exchange less efficient.30
The delivery of goal-directed therapy may be hampered by the inability of practitioners to recognize shock. Infants and children have a greater capacity to increase systemic vascular resistance in shock states and tend to preserve blood pressure until very late in the evolution of shock.31 Pediatric shock resuscitation protocols developed by the consensus of experts in the field call for treatment of shock using clinical signs, including age-specific targets for heart rate and blood pressure, and relatively subtle indicators of perfusion as therapeutic endpoints.32
Rapid Transfer, Goal-Directed Therapy, and the Golden Hour
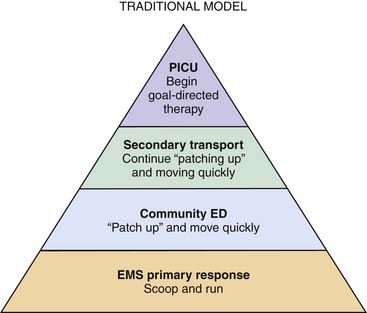
EMS and regional flight teams focused on adult experience work under the assumption that the time between the moment of injury and arrival at a center capable of delivering definitive care is among the most important determinants of survival. This “golden hour” is the driving force for clinical decision-making and usually translates into providing minimal care and moving quickly (Figure 14-1). The concept of the “golden hour” often is described as having its origin in a surgical commentary by Cowley et al.33 on the success of implementing a helicopter-based program for trauma, during an era when prehospital care consisted of providing supplemental oxygen and a fast-moving vehicle. “Scoop and run” and the “golden hour” remain the prevailing philosophies in the transport of infants and children, few of whom benefit from the speed of transport alone.
There are a few disease processes, such as aneurysms requiring neurosurgical intervention or complete transposition of the great arteries requiring urgent atrial septostomy, in which rapid transport to a center that can provide definitive care is the most pressing issue. These are rarities. Respiratory insufficiency and shock are common reasons for referral of pediatric patients. A recent study identified shock in 37% of children transferred to tertiary centers regardless of the reason for referral.34 It is increasingly recognized that rapid resuscitation is critical to the management of pediatric shock.32 In adults and children, protocolized, aggressive, early therapy of septic shock has proven vastly more effective than any pharmacological intervention.2,22,34,35 Aggressive fluid resuscitation and initiation of inotropes and antibiotics should be accomplished within the first hour after presentation. In adults with septic shock, a delay in antibiotic therapy is associated with worse survival, with mortality increasing by 7% for every 30 minutes that passes without delivery of appropriate antibiotic therapy.3
The American College of Critical Care Medicine (ACCM) clinical practice parameters for hemodynamic support of pediatric and neonatal septic shock are divided into specific tasks to be accomplished in the first 5 minutes, the first 15 minutes, and the first hour. The recommended treatments are simple interventions that can be initiated in community EDs and continued and refined in transport, provided that the treating physician and transferring team appreciate the urgent need and are sensitive to the subtle signs of shock in children. Han et al. reported that when community physicians aggressively resuscitated and successfully reversed shock before a transport team arrived, patients had a ninefold increase in their odds of survival.22 These studies defy the popular notion that out-of-hospital stabilization “wastes time” and “delays” definitive therapy that should be rendered at the receiving facility. Initiating treatment in the referring facility to the best of the institution’s ability and bringing skilled transport personnel to the child rather than transporting the child with inadequately skilled personnel may markedly decrease the time to effective treatment.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree