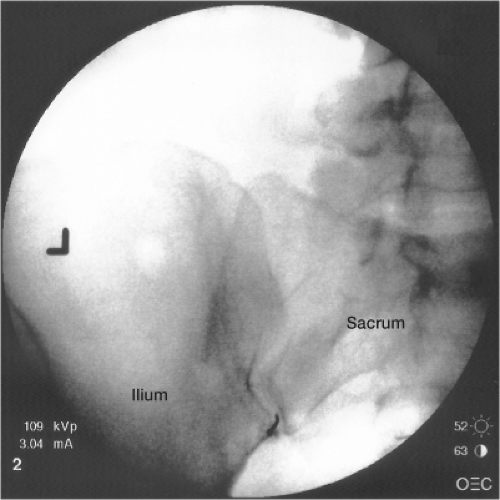
Sacroiliac Joint Injections
The sacroiliac (SI) joint is the weight-bearing joint between the sacrum at the base of the spine and its connection to the ileum of the pelvis (Fig. 21-1). The location of the SI joints is visible at the gluteal dimples (Fig. 21-2). There is both a left and right SI joint. The SI joints are located where the spine connects to the pelvis, and they are subject to a good amount of stress by virtue of their function. The SI joints are a common origin of pain, being the source in 13% to 19% of patients with chronic low back pain.1,2 SI joint degeneration develops more often in patients who have had lumbosacral fusion regardless of the number of fusion segments. On history, patients describe SI joint pain as achy and sharp. Sometimes they report that climbing stairs makes it worse. The pain may radiate into the thigh or groin, mimicking facet or hip joint pain. On physical examination, when the hips are pushed together SI pain might be elicited. However, physical examination is notoriously unreliable for teasing out SI pain. The pain may affect one SI joint (unilateral) or both SI joints (bilateral).
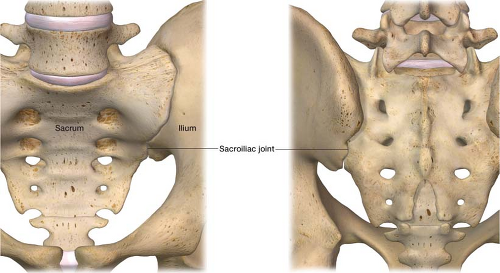 Figure 21-1 Anatomy of the sacroiliac (SI) joint. The weight-bearing joint between the sacrum at the base of the spine and its connection to the ileum of the pelvis. |
When to use
SI joint injections can be both diagnostic and therapeutic. As previously mentioned, it is difficult relying on history and examination to clearly identify if the SI joint or joints are the source of pain. A diagnostic block is a reliable way to determine definitively whether the SI joint or joints in question are the source of pain: If anesthetic relieves the pain, this confirms the diagnosis. Diagnostic blocks help protect the patient from undergoing needless pursuit of competing diagnoses and from undergoing presumptive treatment that is not appropriate for SI joint pain. If the SI joint is indeed the source of pain, the patient should feel relief in this area after the procedure. The patient may not be relieved of 100% of their pain, as there may be several other pain generators.3 However, the percentage of the patient’s back pain that stems from the SI joint can be determined by this method.
Before the procedure, it is predetermined whether to block a single SI joint or both SI joints based on the patient’s pain. If the pain is confirmed to be coming from the SI joint or joints with a diagnostic block, there are interventional therapeutic options. Patients may receive therapeutic injections of cortisone directly into the joint. Another therapeutic option is radiofrequency (RF) ablation of the nerves that transmit painful impulses from the painful SI Joint.
How to Perform the Procedure
Diagnostic Sacroiliac Joint Injections
It is necessary to explain the procedure to the patient completely, answer all questions, and obtain informed consent. For accuracy and safety, SI joint injections are performed under fluoroscopic guidance (live x-ray).
After arrival at the fluoroscopy suite the patient lies on the fluoroscopic table in the prone position (face down). A “time out” is performed prior to the procedure including verbal confirmation of correct patient, procedure and procedural site. Noninvasive hemodynamic monitors and pulse oximetry are placed. The fluoroscope is placed in the anteroposterior (AP) position. Radiographically the SI joint does not have a single silhouette of its articular cavity. To help isolate the posterior margin of the joint the C-arm of the fluoroscope should be rotated usually to the contralateral side until the medial inferior aspect of the joint is maximally crisp. Usually 5–20 degrees of contralateral rotation is necessary to properly improve the picture. The target is, approximately 1–2 cm cephalad of the most inferior aspect of the joint. The skin is prepped with betadine and drapes are placed over the area in standard sterile fashion. Using a metal marker and a felt-tip marking pen, an “X” is placed on the skin overlying the intended target, the inferior aspect of the SI joint (Fig. 21-3). The skin is anesthetized with lidocaine using a 1.5-in, 25-gauge needle. After the skin is anesthetized a 3.5-in, 22-gauge spinal needle with a curve at the end—the physician typically bends the needle to create a curve (Fig. 21-4)—is placed through the “X” in a perpendicular fashion to the skin and parallel to the fluoroscope (Fig. 21-5). The needle is advanced until it enters the SI joint and bone is touched. The stylet of the needle is then removed. A 3-mL syringe with tubing containing contrast is connected to the needle. Tubing
is used so that you can see the contrast being injected under live x-ray without having your hand obscure the image and to protect your hand from radiation exposure. A small amount (1 mL) of contrast is injected to make sure that it spreads in the intra-articular joint space. Once proper contrast spread is seen (Fig. 21-6), the 3-mL syringe is disconnected from the tubing. A local anesthetic is then injected via a 10-mL syringe connected to the tubing. I use 1.5 mL of 0.5% bupivacaine as my diagnostic agent. The needle is removed and a bandage placed. In the recovery room, the preoperative pain score is compared with the postoperative score to see if the SI joint or SI joints are the pain generator.
is used so that you can see the contrast being injected under live x-ray without having your hand obscure the image and to protect your hand from radiation exposure. A small amount (1 mL) of contrast is injected to make sure that it spreads in the intra-articular joint space. Once proper contrast spread is seen (Fig. 21-6), the 3-mL syringe is disconnected from the tubing. A local anesthetic is then injected via a 10-mL syringe connected to the tubing. I use 1.5 mL of 0.5% bupivacaine as my diagnostic agent. The needle is removed and a bandage placed. In the recovery room, the preoperative pain score is compared with the postoperative score to see if the SI joint or SI joints are the pain generator.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree