Fig. 37.1
Ligaments of the Sacroiliac Joint
There are several myofascial structures that influence movement and stability, the most notable of which includes the latissimus dorsi via the thoracolumbar fascia, the gluteus maximus, and the piriformis. Multiple studies suggest that SIJ stiffness increases with muscle activity, supporting the notion that effective load transfer from the spine to the legs is possible when muscle forces actively compress the SIJ, therefore preventing shear. Altered motor control of deeper muscles, like the transversus abdominus, internal oblique, multifidus, diaphragm, and pelvic floor muscles, plays an important role in both lumbo-pelvic support and pain generation [22].
The SIJ allows movement of the pelvis about the axis of the sacrum, which serves the important functional role of transferring forces in a bidirectional manner. These forces occur during standing and ambulation, between the upper body and the lower extremities, and in the sitting position, between the trunk, ilia, and ischial tuberosities. Although little joint motion exists, it appears to be sufficient enough to decrease the cost of ambulation by storing and releasing energy, which thereby diminishes stress on the pelvic ring by absorbing shock [23]. Nutation denotes sacral base movement in an antero-inferior direction in relation to the ileum that occurs during lumbosacral extension. During lumbosacral flexion, the sacral base moves postero-superior. This opposite movement is termed counter-nutation. There are conflicting reports regarding the position of the instantaneous axes of rotation, the extent of movement, and the existence of motion in other dimensional planes [16].
Under the special physiologic conditions of pregnancy, hormone-induced laxity of the sacroiliac and pelvic ligaments allows for the mobility necessary for gestation and parturition. The hormone-induced ligamentous laxity, pregnancy-associated weight gain, exaggerated lordotic posture, and the mechanical stress associated with parturition, all predispose women to SIJ pain [24].
The variable distribution of referred pain from the SIJ can be attributed in part to its size and heterogeneity, but also to the variable nature of its sensory innervation, which remains controversial. The literature suggests that the posterior SIJ is supplied by lateral branches of the S1 to the S3 dorsal rami, with some evidence of contributions by the dorsal rami from L3 to S4 (Fig. 37.2) [21]. The anterior joint might receive contributions from different combinations of the ventral rami of L2 through S2, and even from the obturator and superior gluteal nerves ; however, it is also believed that the SIJ might be devoid of innervation [16, 25].


Fig. 37.2
Innervation of the posterior SIJ. Original figure by Attias et al.
Pathophysiology
Injury and pain generation from the SIJ generally results from a failure of its stabilizing ligaments, as well as dysfunction of the joint’s anatomical relationships. Destabilizing compressive and torsional shearing forces, which result from excessive axial loads and rotation, can injure the SIJ and associated myofascial structures. Acute, high velocity, repetitive, and asymmetrical forces will have significant impact, but whether acute or insidious, the injury may trigger capsular or synovial disruption, capsular or ligamentous tension, ankylosis or hypermobility, micro or macrofractures, chondromalacia, soft-tissue injury, and inflammation. All these factors are usually followed by abnormal joint mechanics and altered or maladaptive regional biomechanics that can further exacerbate SIJ pathology, dysfunction, and pain [21, 26].
Common Diagnoses/Symptoms Treated
LBP is defined as such pain occurring within a region limited by the outer borders of the erector spinae laterally, the imaginary line through the T12 spinous process superiorly, and a line through the S1 spinous process inferiorly. Sacral pain is defined as that being confined within a region overlying the sacrum and contained between the imaginary vertical lines drawn through the posterior-superior and posterior-inferior iliac spines, and within the transverse lines passing through the S1 spinous process superiorly, and by the posterior sacro-coccygeal joints inferiorly [27].
Pain originating from structures in these regions typically crosses these boundaries. Thus, SIJ pain is often perceived in the lower back, groin, buttocks, lower extremities, and abdomen. Pain caused by SIJ dysfunction can be similar to pain from a discogenic or radicular source. More commonly, it presents unilaterally, below the belt line, in the groin, and over the postero-lateral thigh (Fig. 37.3). It might present with associated crepitus or popping. A study reported that in 22.5% of the involved population with SIJ pain, the radiation pattern was toward the calf and foot [12]. This frequent observation generates confusion given the similarity in referral patterns between SIJ pain and discogenic or radicular pain. It has been noted that any pathology in the SIJ, which causes spasm of the piriformis muscle, may also lead to sciatic nerve irritation as well as a broad spectrum of symptoms, in addition to a variety of radiation patterns [27]. Very frequently, symptoms are perceived and described by the patient as “sciatica”.
Fig. 37.3
Common pain referral patterns from the SIJ. Original figure by Zhukova-Attias
Common mechanisms causing traumatic disruption of the SIJ include motor vehicle accidents, falls, athletic injuries, as well as childbirth. Pain is exacerbated with SIJ loading, which can occur after prolonged sitting, standing, walking and climbing stairs, or by transition from these positions [28, 29].
Multiple etiologies are associated with SIJD and pain (Table 37.1). The HLA-B27 gene is strongly associated with ankylosing spondylitis (AS) and other inflammatory diseases like psoriasis, inflammatory bowel disease, and reactive arthritis. Seronegative and HLA-B27-associated spondylo-arthropathies are notable for producing inflammation at one or both SIJs. Unlike other forms of arthritis and rheumatic diseases, onset of AS commonly occurs in younger people, between the ages of 17–45. However, it can affect children, as well as an older population. AS is more common in men, but occurs in women as well. Infection can be a source of SIJ pain and etiologies include reactive arthritis in HLA-B27 carriers, reactive arthritis associated with HIV-positive individuals, and other rare local infections [26]. Tumors infiltrating the SIJ with resulting pain have been reported, and regional malignancies can certainly trigger or mimic SIJ pain [30]. Regardless of the etiology, both pain and proprioception are transmitted from the SIJ. This is supported by anatomical studies demonstrating the articular presence of both myelinated and unmyelinated nerve fibers, as well as mechanoreceptors [31–34].
Table 37.1
Differential diagnostic categories of SIJ pain generators
Intra-articular sources | Extra-articular sources (more common) |
|---|---|
Spondyloarthropathy | Fractures |
Metabolic and endocrine disorders (crystal-induced joint disorders, hyperparathyroidism) | Trauma |
Arthritis (osteoarthritis and inflammatory) | Ligamentous injuries |
Infection | Myofascial components |
Malignancy | Pregnancy (hypermobility) |
Joint trauma | Malignancy |
True and functional leg length discrepancy | |
Spinal surgery | |
Transitional anatomy |
The differential diagnostic categories for SIJ pain are summarized in Table 37.1. The most common presenting clinical features and pain patterns of SIJD are outlined in Table 37.2. Fig. 37.3 shows common pain patterns . The International Association for the Study of Pain diagnostic criteria for SIJ pain [35] are outlined in Table 37.3.
Table 37.2
Clinical features of SIJ pain
Lower back pain (below L5) |
Pelvic/buttock pain |
Hip, groin, postero-lateral thigh pain |
Lower extremity pain, numbness, tingling, weakness |
Unilateral (4:1 vs. bilateral) |
Subjective leg instability (buckling, giving way) |
Decreased tolerance to sitting positions and side-sleeping |
Exacerbation with transitional activities (i.e. rising from a seated position and climbing stairs) |
Table 37.3
IASP criteria for SIJ pain
Positive Fortin finger test, i.e. pain located within 1 cm inferior-medial to the PSIS |
Pain that is relieved by injection of the SIJ |
At least three positive provocative pain tests (0.82 for sensitivity, 0.88 for specificity, 0.86 for positive predictive value of a test, and 0.84 for negative predictive value) (2015-04-16) |
Treatment Options
This chapter section will focus on technical aspects of the therapeutic modalities used for SIJ pain. Additionally, it will provide suggestions regarding their position in the treatment algorithm, once the correct diagnosis is made. The available supporting evidence will be discussed further in section “Potential Treatment Complications”. Medical management of individual etiologies will not be discussed, but we encourage the reader to refer to the recommended reading list, as well as to the pathology section of this chapter.
Conservative Management/Physical Therapy
Once SIJD has been appropriately diagnosed, the initial treatment often begins with conservative management, similar to other types of joint-associated pain. Conservative management of SIJD may include medication, physical therapy, manual therapy, and durable medical equipment.
The basic principles of medical pain management apply to the treatment of SIJD, including the use of oral steroids, non-steroidal anti-inflammatory drugs, non-opiate analgesics, antidepressants, anti-spasmodics, and other adjuvant medications [36]. Often the combination of these medications, along with other conservative treatment options, provides better outcomes. Physical therapy can provide a structured exercise program with a specific focus on SIJD, to help ease stress on the SIJ, reduce inflammation, remedy associated muscular dysfunction, and to improve functional status. This is accomplished by exercises focused on strengthening and stretching of the musculature surrounding the SIJ (i.e. gluteal muscles, hamstrings, hip flexors/extensors), pelvic floor muscles, and core muscles in the lower back, which help to offload tension on the SIJ [37]. Combining both passive (i.e. application of stretch by therapist) and active (i.e. resistance exercise) physical therapy treatment provides the best outcomes.
Manual methods for correcting SIJD fall into three broad categories, which include the following: direct mobilization, direct manipulation, and indirect techniques. No single discipline (osteopathic, chiropractic, or manual physical therapy) has been shown to be superior to another [36]. The overall goal of these techniques is to restore physiologic motion of the SIJ.
Direct mobilization includes both soft tissue mobilization (SMT) and joint mobilization (JMT). SMT addresses muscle tension and attempts to break up inelastic or fibrous muscle tissue (myofascial adhesions) and to relax muscle tension. This procedure is applied to the musculature surrounding the SIJ by placing traction force on the tight area in an attempt to restore normal texture to tissue and to reduce associated pain. JMT involves loosening up the restricted joint, increasing its range of motion by providing slow velocity, and increasing amplitude movement directly into the barrier of a joint, which moves the actual bone surfaces over each other in ways patients cannot otherwise move the joint themselves.
Direct manipulation introduces high velocity, low amplitude thrusting, which aims to restore the gliding motion of joints, enabling them to open and close more effectively. It is a more aggressive technique than joint mobilization and muscle energy techniques, which thrust a joint to its restrictive barrier, but not past it. If utilized properly, increased mobility and decreased muscle tone about the joint should be noticed [38].
Indirect techniques include muscle energy techniques (METs) and are designed to mobilize restricted joints and to lengthen shortened muscles. The mechanism of action utilizes a voluntary contraction of the patient’s muscles against a distinctly controlled counterforce, which is applied by the therapist, from a precise position and in a specific direction. Following a 3–5 s contraction, the therapist takes the joint to its new barrier, where the patient again performs a muscle contraction. According to a study done by Visser and associates, out of 51 patients identified with SIJD-associated leg pain, manual therapy had a significantly better success rate with improved pain scores and increased function when compared to physical therapy and intra-articular SIJ injections [39].
Durable medical equipment such as SIJ (Pelvic) belts can help to stabilize the SIJ, provide biofeedback, and give pain relief for patients with SIJD. Proper positioning of the belt is important, which should be placed directly superior to the greater trochanter [40]. Pelvic belts can help to decrease sacroiliac joint motion by approximately 30% [41].
Interventional Management
SIJ Injections
As mentioned previously, SIJ anesthetic injections are considered a reference standard to diagnose SIJ-related pain. As a therapeutic intervention, most studies agree that analgesic effects from the addition of corticosteroids are significant in the short term, but decline over time, generally 3–6 months. Injections may be directed inside the joint (intra-articular injections), may be directed to the supporting ligaments and muscles that comprise the articulation (extra-articular injections), or may combine both targets. In younger, more active patients, extra-articular pathology with unilateral pain is more common. In the elderly, intra-articular pathology and bilateral pain is more frequent [18, 19]. Depending on the patient, either technique might be of benefit. In our opinion, most patients will benefit from a combination approach.
It is now common practice to utilize either fluoroscopy or CT-guidance to perform SIJ injections , the latter of which is restricted by higher radiation exposure and availability in the pain clinic setting. Ultrasound-guided techniques are becoming increasingly incorporated into pain clinic practices, but are highly dependent on operator experience [42]. For fluoroscopy-guided sacroiliac joint injections, a common technique involves advancing a 22-gauge spinal needle into the infero-posterior aspect of the joint, an area 1–2 cm cephalad to the joint’s most caudal end. The needle is advanced, while rotating the C-arm approximately 30° caudal to the axial plane, to better visualize the area inferior to the posterior superior iliac spine and the iliac crest. Contralateral oblique angulation may be added to further demarcate the joint space. Penetration of the posterior capsule is usually felt as a change in resistance. This may not be felt in all patients, in particular those with significant osteoarthritic changes and ankylosis. In such cases, an extra-articular injection might be necessary. Contrast media can be used to verify placement and to rule out intravascular injection. The total amount of steroid and/or local anesthetic injectate volume should not surpass 3 mL to avoid painful joint distention (Fig. 37.4-1).
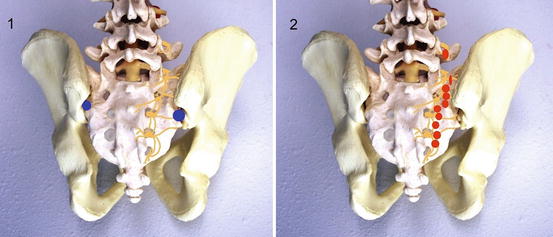
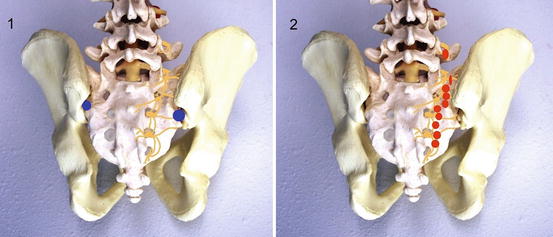
Fig. 37.4
Target locations for SIJ injections (1) and RFA ablations (2). Original figure by Attias et al.
Instillation of neurolytic agents like phenol has been tested, in an attempt to prolong the relief obtained with corticosteroids. However, phenol is rarely used in clinical practice due to the high risk of extra-articular spread to susceptible structures [43]. Although visco-supplementation with hyaluronic acid may also represent a reasonable alternative, given the demonstrated benefit in osteoarthritis of the knee and hip, only small series exist studying subgroups of patients with degenerative SIJ arthritis [44].
Radiofrequency Denervation
For patients who obtain good, yet short lived, response from SIJ steroid injections, radiofrequency (RF ) lesioning of the lateral branch nerves that innervate the SIJ should then be considered. In conclusions derived from a randomized trial by Dreyfuss et al., Cohen et al. [7] support the notion that lateral branch denervation should be more effective in alleviating extra-articular SIJ pain; additionally, either lateral branch or extra-articular blocks are thought to serve as better predictors of RF denervation response than intra-articular injections.
As previously noted, the posterior aspect of the SIJ is innervated by the L5 dorsal ramus and the lateral branches of S1, S2, and S3, with possible contributions from the L4 dorsal ramus. Anesthetic blockade of these structures can predict response to RF ablation of the same nerves. This can be achieved by guiding a needle to a point 5 mm lateral to each foramen, between the 2 and 5 o’clock positions on the right side, and the 7 and 10 o’clock positions on the left side. These targets will correspond to the path of the lateral branch, as it travels laterally toward the joint. The L4 and L5 dorsal ramus can also be included by using the same technique required for medial branch blockade.
Standard monopolar RF ablation of the sacral lateral branches will result in a restricted lesion. Given the size and variable location of these nerves, multiple techniques have been described to increase the chance of achieving denervation. For example, utilizing multiple probes and creating bipolar RF “strip lesions” can be considered, and targets may be expanded to include the terminal fibers innervating the joint. This requires the placement of multiple successive probes, with a separation of less than 1 cm, in a trajectory parallel to the path of the nerves, which are targeted as described for the diagnostic blocks. Therefore, this creates multiple lesions in a “leapfrog” manner (Fig. 37.4-2). Addition of normal or hypertonic saline solutions before lesioning and proper lesion time may increase the size of the lesions, while diminishing the spread of tissue destruction beyond the electrodes [45]. Prior to lesioning, sensory and motor nerve stimulation should be performed to verify concordance and absence of muscle contraction in a radicular distribution. Finally, the addition of anesthetic and steroid mixtures after the lesioning will provide post-procedural analgesia and may prevent neuritis.
There is higher level evidence that cooled RF neurotomy is beneficial to treat SIJ pain, presumably due to the larger lesion size attainable with this technique, with a higher analgesic response at 3 months when compared to traditional radiofrequency, but no significant difference between both modalities at 6 months [19]. Other tools capable of creating multiple lesions with a single device have entered the market (Fig. 37.5) with the goal of decreasing procedural complexity, as well as improving outcomes [46, 47].
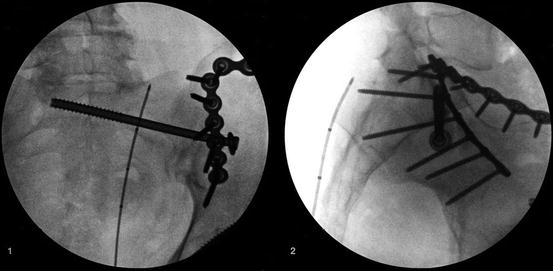
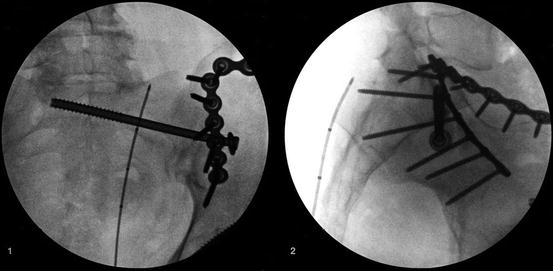
Fig. 37.5
Sacroiliac joint radiofrequency ablation with a multi-lesion probe. Images courtesy of Dr. Stanley Golovac
Neuromodulation
Non-neurolyitic pain modulation therapies like spinal cord, peripheral nerve, and peripheral field stimulation are, in general, considered effective for neuropathic pain syndromes. Predominantly nociceptive pain syndromes, like SIJ pain, are widely considered less responsive to neurostimulation. Despite this assumption, several reports utilizing this therapy targeting different neural targets can be found in the literature, with the goal of treating intractable SIJ pain. [47–49]. Intrathecal opiate and non-opiate infusion pumps are traditionally considered better options to control chronic intractable nociceptive pain arising from these structures, but still typically require ongoing interventional strategies and physical therapy to maintain function, and to keep medication infusions within the recommended dosages.
SIJ Fusion
SIJ arthrodesis, or fusion, is a surgical technique used to treat back or leg pain caused by SIJD that remains controversial. Arthrodesis should be considered only in patients with joint pain proven by controlled diagnostic anesthetic blocks and without any source of pain from the lumbar spine. It also should be reserved for those patients who continue to have disabling symptoms that have not responded to aggressive conservative care [36]. Numerous techniques exist for the surgical fusion of sacroiliac joint. The main goal is to stabilize the joint by using implants and/or instrumentation that can be accomplished by an open surgical procedure (OS) or by a minimally invasive surgery (MIS).
Smith-Petersen first reported SIJ arthrodesis in 1921 [50]. Studies that followed included non-instrumented approaches to achieve arthrodesis and most required either long periods of immobilization, or casting and bracing for a substantial period of time [51]. In the mid-1980s, there were reports of internal fixation using metal plates and screws [52–55]. Reports of minimally invasive surgical (MIS) techniques to address the SIJ began appearing in 2008. However, instrumentation remained limited to threaded screws and cages that rely on autologous bone grafts [56–58]. Recently, new MIS techniques have been introduced with promising outcomes [59–64]. According to a multi-center comparative study done by Smith et al., in which 263 patients underwent either open surgical (OS) or MIS SI joint fusion, patients showed postoperative improvements in pain score. Compared to OS patients, MIS patients had significantly greater pain relief and more favorable peri-operative surgical measures [65]. According to a literature review performed by Zaidi et al., surgical intervention for SIJ pain is beneficial in only a subset of patients. However, with the difficulty in making an accurate diagnosis and with the lack of evidence for the efficacy of SIJ fusion itself, serious consideration as to the cause of pain and alternative treatments should be given before performing the operation [66].
Complementary and Alternative Techniques
Regenerative medicine is considered a paradigm shift in the treatment of degenerative and overuse injuries. Historically, pain symptoms due to these types of injuries were often treated with corticosteroid injections to alleviate the inflammatory component. The goal of regenerative medicine is to directly or indirectly draw upon growth factors and mesenchymal stem cells to regenerate injured tissue. Regenerative medicine includes novel therapies such as prolotherapy and platelet rich plasma injections (PRP).
Over the past several decades, prolotherapy or proliferative therapy has been mostly performed outside of mainstream medicine by independent physicians. More recently, multi-specialty groups, which include family or sports medicine physicians, physiatrists, orthopedic surgeons, neurologists, and anesthesiologists, have been incorporating prolotherapy as the result of both positive clinical experience and reports in the literature. Dorman et al. observed in vitro that injecting chemical irritants into ligamentous tissue incites collagenous proliferation [67].
Prolotherapy treatment has been advocated for a variety of soft tissue conditions, including non-specific low back pain, chronic musculoskeletal pain, and hyper-mobility of joints [68]. In the treatment of a hyper-mobile sacroiliac joint, a combination of concentrated dextrose and a local anesthetic is injected into the affected joint. Prolotherapy has been defined as “the rehabilitation of an incompetent structure, which included ligaments or tendons, by the induced proliferation of new cells” [69]. In 1937, Earl Gedney injected a hyper-mobile sacroiliac joint with sclerosing agents, resulting in satisfactory results in pain improvement [67]. According to a study done by Cusi et al., in which 25 patients underwent CT-guided SIJ prolotherapy, 76% of patients had a positive clinical outcome at both 3 and 12 months post-therapy [70]. Kim et al. compared intra-articular prolotherapy to intra-articular corticosteroid for SIJD and found that dextrose injections provided improved analgesia compared to corticosteroid [71]. Drawbacks to this method of treatment include the need for multiple injections, the potential for considerable post-injection pain, and the general lack of research supporting efficacy [72].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






