CHAPTER 18 Right Ventricular Infarction
INFARCTION OF the right ventricle, previously considered rare and clinically unimportant,1,2 is now recognized as a common clinical event, occurring in one third of patients with inferior myocardial infarction (MI).3–5 Right ventricular (RV) infarction confers a worse prognosis in patients with inferior wall MI.4 Prompt recognition and appropriate treatment of RV infarction require a thorough understanding of the unique anatomy and pathophysiology of the right ventricle.
Historical Perspective
In 1930, Sanders6 reported the first clinical description of RV infarction. During the following 4 decades, RV infarction received attention mainly in autopsy series.7 At that time, any shock syndrome was considered the result of left ventricular (LV) infarction.1,2 This view was buttressed by evidence from open pericardium dog models in which destruction of the right ventricle was not associated with shock.8,9 The development of surgical procedures that bypassed the right ventricle, such as the Glenn and Fontan procedures, furthered the belief that the right ventricle is mainly a volume conduit contributing little to cardiac output.10,11
In 1974, Cohn and coworkers12 first called attention to RV infarction as a unique clinical and hemodynamic syndrome, characterized in its extreme form by shock, distended neck veins, and clear lung fields. During the ensuing 2 decades of intense investigation into the syndrome, the crucial role of ventricular interdependence through the pericardium and the septum was recognized.13–16 Today, a rational approach to therapy of RV infarction based on an understanding of its pathophysiology is possible.
Coronary Circulation and the Right Ventricle
In patients with right dominant coronary circulation (85% of the population), the right ventricle receives its blood supply almost exclusively from the right coronary artery (RCA), with the septum and part of the posterior wall supplied by the posterior descending artery, and the anterior and lateral RV walls supplied by acute marginal branches of the RCA.17,18 The left anterior descending (LAD) artery supplies a small portion of the anterior wall of the right ventricle. In a left dominant circulation, the left circumflex coronary artery supplies the posterior descending artery, and a nondominant RCA supplies the acute marginal branches. Isolated RV infarct without LV involvement can occur with a nondominant RCA.
The angiographic hallmark of RV infarction is thrombotic occlusion of the RCA proximal to the origin of the acute marginal branches. Angiographic flow studies suggest the status of RV branch perfusion is the critical determinant of RV ischemic dysfunction.19 Proximal RCA occlusions would typically limit RV branch perfusion, in contrast to distal RCA occlusions. Mid and distal RCA occlusions less commonly cause severe RV ischemic dysfunction by flow impairment in at least one major RV branch attributable to the culprit stenosis, prior severe RV branch stenosis, or presence of RV branch thrombus.19
Not every case of proximal RCA occlusion results in RV infarction.18 This relative protection of the right ventricle from infarction is thought to be a consequence of its lower oxygen demand, its continued perfusion during systole, and the existence of collaterals from the LAD artery, which, because of the lower systolic pressure on the right side, are more capable of supplying blood in the direction of the right ventricle than in the reverse direction. The LAD collaterals to the right ventricle are mainly through the moderator band artery, a branch of the first septal perforator.20 Prior severe stenosis or occlusions of the LAD artery can limit the development of collaterals to the right ventricle with the occurrence of an acute RCA occlusion increasing the extent of acute ischemic RV dysfunction.21
Conflicting data, particularly in autopsy series, exist concerning RV infarction in the setting of LAD obstruction producing anteroseptal infarction.18,22–24 With LAD occlusion, the clinician would expect the septal portion of the right ventricle and a small portion of the anterior RV wall to be affected. Andersen and colleagues,22 in an autopsy study of 107 patients, were able to detect evidence of RV infarction in more than half of the patients with anterior infarcts, but the amount of RV tissue affected was small (1% in anterior infarction versus 15% in posterior infarction). Hemodynamically significant RV infarction with LAD occlusion is probably rare.22 In the case of a left dominant circulation, the circumflex artery supplies the posterior septum and posterior wall of the right ventricle through the posterior descending artery. Although obstruction of the circumflex artery may lead to RV involvement, hemodynamically significant RV infarctions are uncommon because the nondominant RCA continues to supply the lateral RV wall and most of the anterior RV wall through the acute marginal branches.
Ventricular Interdependence
The concept of ventricular interdependence in RV infarction is central to understanding the pathogenesis of the resultant low cardiac output state. Ventricular interdependence is mediated through the common pericardium and shared septum. In RV infarction, acute RV dilation occurs.15,16,24 Because the right ventricle shares a relatively fixed space with the left ventricle, the pericardial pressure abruptly increases, leading to impaired LV filling. In animal models with the pericardium removed, it is difficult to induce hypotension with RV infarction.8 When the pericardium is left intact,16,25 however, RV infarction is associated with the full syndrome, as originally described by Cohn and coworkers.12 Incision of the pericardium leads to improvement in cardiac output, pressure equalization, and an increase in RV systolic pressure.16
The increase in right-sided diastolic pressure that occurs in RV infarction leads to a reversal of the normal left-to-right transseptal diastolic gradient.26 On echocardiography, the septum can be seen to flatten and encroach on the LV diastolic dimension. During systole, the septum can be seen to move paradoxically toward the right ventricle, at times in a piston-like manner.16
Except in rare cases of isolated RV infarction,27,28 LV infarction accompanies RV infarction. The pericardial constraint and alterations in septal geometry lead to reduced LV filling, and cardiac output is diminished further by the decrease in LV systolic function. Development of the shock syndrome with isolated RV infarction27 proves, however, that LV systolic dysfunction is not a necessary component. Echocardiographic assessment in cases of hemodynamically severe RV infarction has confirmed that shock may be present with preserved LV systolic function.16
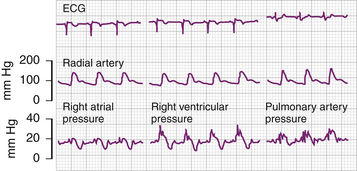
The hemodynamic hallmarks of RV infarction (Table 18-1) are a decrease in cardiac output, elevation of right atrial pressure (>10 mm Hg), elevation of RV diastolic pressure, and decrease in RV systolic pressure.29–31 There is diastolic equalization of RV and LV pressures, as in cardiac tamponade, and the ratio between right atrial and pulmonary capillary wedge pressure increases. This ratio, which normally is less than 0.65, is usually greater than 0.8 in RV infarction.29 The RV tracing reveals a delayed, depressed, and often bifid peak, indicating systolic RV failure.16 RV diastolic failure is also manifested by a dip and plateau pattern on the RV pressure tracing.
Table 18–1 Hemodynamic Findings in Cases of Right Ventricular Infarction
| Elevated right atrial pressure (>10 mm Hg) |
| Right atrial pressure/pulmonary wedge pressure ratio >0.8 |
| Noncompliant jugular venous pattern (prominent y descent) |
| Dip and plateau right ventricular diastolic pressure pattern |
| Depressed and delayed (often bifid) right ventricular systolic pressure |
| Decreased cardiac output |
| Hypotension |
In most studies, hemodynamic tracings showed a blunted x descent with a prominent y descent, suggesting decreased compliance of the right ventricle, as seen in pericardial constriction (Fig. 18-1).18,29–33 In contrast, Goldstein and coworkers,16 when using RV pressure tracings to time hemodynamic events, described a prominent x descent with blunting of the y descent, as seen in tamponade. They also showed that atrial function was of pivotal importance. In some patients, there was an increase in atrial function, as evidenced by augmented a waves. These patients had a better response to therapy and had a better prognosis than patients with depressed atrial function. The latter group was shown to have more proximal RCA occlusion, affecting the atrial branches of the RCA and causing superimposed atrial infarction. Although the hemodynamic criteria for RV infarction are usually present on admission, volume loading may increase the identification of these abnormalities in a few patients.30
Clinical Presentation
Clinically significant RV infarction occurs mainly in patients with concomitant inferoposterior infarction of the left ventricle, and many of the symptoms overlap. Necropsy studies suggest that RV infarction occurs almost exclusively in patients with transmural posteroseptal MI.34 The size of the LV infarct does not correlate with RV infarct size. The size of the RV infarct influences the severity of RV dysfunction and presentation, however.21 What is unique to RV infarction is the occurrence of a syndrome of RV diastolic and systolic failure that, in its extreme form, is characterized by a triad of signs: hypotension that can progress to cardiogenic shock, elevated neck veins, and clear lung fields.6,12,18,35
When RV infarction is hemodynamically significant, the physical examination is a sensitive method of detection. Dell’Italia and colleagues35 found elevated jugular venous pressure to be 88% sensitive, with a specificity of 69% for inferior wall MI with RV involvement. Kussmaul sign, an inspiratory increase in the jugular venous pressure, was found to be 100% sensitive and specific in the same series, and Bellamy and coworkers36 found it to have a sensitivity of 59% and a specificity of 89%. Other associated findings include a high frequency of bradycardia and atrioventricular (AV) block and atrial arrhythmias, including supraventricular tachycardias and atrial fibrillation or flutter. A right-sided fourth heart sign was described in 11 of 16 patients in one series, with 4 of 16 having a right-sided third heart sound.37 Tricuspid regurgitation may be audible. Pericardial friction rubs may be heard because infarction in the thin right ventricle is usually transmural.33
The differential diagnosis includes tension pneumothorax, cardiac tamponade, constrictive pericarditis, and pulmonary embolism. When the full triad is present, and ST segment elevations are observed in inferior leads, the diagnosis is straightforward. A potential pitfall is the occurrence of isolated RV infarction, which may manifest with the full clinical picture, but without electrocardiogram (ECG) evidence of MI on the standard 12-lead ECG.27 Pulmonary embolism occasionally mimics RV infarction and may be a predisposing factor,38 leading to occult RV infarction. Conversely, RV infarction with thrombus formation in the right ventricle can lead to pulmonary embolism. Dyspnea is usually more severe in pulmonary embolism, and RV and pulmonary artery pressures and pulmonary vascular resistance are higher than in RV infarction. Cardiac tamponade may be acute and may manifest with a similar triad of elevated neck veins, hypotension, and clear lungs, but it can be distinguished easily at the bedside with echocardiography. Pulsus paradoxus, a hallmark of tamponade, is unusual in RV infarction, which tends to resemble pericardial constriction.33
Diagnosis
Electrocardiographic Diagnosis
ST Segment
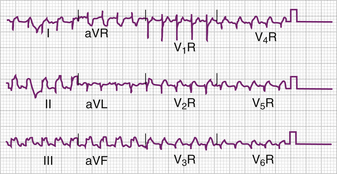
The ECG remains the most useful tool for the diagnosis of RV infarction.39 The hallmark of acute RV ischemia is ST segment elevation in the right precordial leads, a finding first reported in 1976 by Ehrhard and coworkers,40 who used lead CR41 located in the fifth intercostal space at the right mid-clavicular line. The importance of obtaining right-sided chest leads on presentation in patients with suspected MI, particularly with evidence of inferior wall involvement, cannot be overemphasized (Fig. 18-2).
Several studies have documented that ST segment elevation of 0.05 mV or greater (0.5 mm when using standard settings of 10 mm/mV) in lead V4R in the setting of inferior MI is sensitive and specific for RV involvement, as documented by postmortem examination41 or by radionuclide,39,42,43 echocardiographic,42 hemodynamic,39 or angiographic studies.33,43 Braat and colleagues42 found that ST segment elevation of 1 mm or greater in lead V4R had a sensitivity of 93% and a specificity of 95% in a series of 67 patients with inferior MI. ST segment elevation in lead V3R was also specific (97%), but less sensitive (69%). In a series of 110 patients with acute inferior MI, Klein and coworkers,44 using the 0.5-mV criteria, reported a sensitivity of 83% and a specificity of 77%, with a positive predictive value of 70% and a negative predictive value of 88%. Infrequently, ST segment elevation in V5R or V6R occurs in the absence of elevation in V4R.39,42 Zehender and colleagues4,39 confirmed the utility of 0.1-mV ST segment elevation in any of the right precordial leads (V4R-V6R) in a series of 200 patients, showing a sensitivity of 89% and a specificity of 83%.
The ECG findings in RV infarction of right precordial ST segment elevations are the result of a rightward and anteriorly directed vector. Using Grant’s method of spatial vector analysis, Hurst45 emphasized that the clinician can diagnose RV infarction from the standard 12-lead ECG because the ST segment vector is shifted rightward (>90 degrees) toward the site of infarct. A larger RV infarct would be expected to result in greater rightward ST segment vector deviation (>150 degrees). Andersen and coworkers46 showed that ST segment elevation in lead III exceeding that in lead II (i.e., ST segment vector directed rightward) is sensitive (68%) in diagnosing RV infarction. This criterion had a specificity of only 11% and a positive predictive value of 58% in Zehender’s series of 200 patients with inferior MI. Andersen’s criteria were confirmed as being highly sensitive, however (95% in Zehender’s series).
Certain special situations with variant ECG findings that may cause confusion warrant mention. Geft and colleagues47 described five patients with ST segment elevations in leads V1-V5 who on catheterization were shown to have RCA occlusion and acute RV infarction. All five patients had minimal or absent ST segment elevations in the inferior leads. The authors speculate that in the usual cases of RV infarction, ST segment elevations in leads V1-V5 are blocked by the dominant electrical forces of inferoposterior MI, resulting in isoelectric or even depressed ST segments in the left precordium. When these forces are absent, because of isolated RV infarction48 or because of minimal posterior involvement, as may be seen in a patient with a codominant circulation,47 ST segment elevation in the left precordial leads mimicking anterior wall infarction may be seen. A distinguishing characteristic in RV infarction may be that the ST segment elevations are highest in leads V1 or V2 and decrease toward lead V5, a pattern opposite that seen in anterior MI.47
If septal involvement can mimic RV infarction, a left lateral wall infarction or a large true posterior infarction can be expected to cancel right precordial ST segment elevations. Such cases of false-negative findings have been described.44,49
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree