Respiratory Physiology in ECC: Principles of Oxygenation and Ventilation
Elizabeth H. Sinz
Kane High
The arrested circulation requires both ventilation and gas transport to sustain vital organ function while attempts are made to establish a perfusing rhythm. Thus, both ventilations and compressions are important for patients in prolonged cardiac arrest, when the oxygen stores are depleted, and for patients in asphyxial arrest, such as children and drowning patients who were hypoxemic at the time of cardiac arrest.
Optimizing ventilation during cardiopulmonary resuscitation (CPR)
Controversy regarding optimal compression-to-ventilation ratios—the science
Airway anatomy and lung–thorax relationships affecting ventilation
Overview
Health care providers learn to use a systematic approach to adult resuscitation based on the Basic Life Support (BLS) Primary Survey and the Advanced Cardiac Life Support (ACLS) Secondary Survey. Many of the topics in this initial assessment are organized around the A (airway) and B (breathing) components of these surveys. An organized approach to airway management is critical and monitoring of ventilation and oxygenation is mandatory.
Respiratory Physiology
Although respiration is commonly perceived as the act of breathing, respiration is more precisely defined as the provision of gas exchange at the tissue and cellular level. There are three other functional components of respiration. Pulmonary ventilation is the exchange of gas between the atmosphere and alveoli. The end result of pulmonary ventilation is diffusion of oxygen and carbon dioxide between the alveoli and blood. Circulation or transport of gases to and from the tissues is dependent on normal cardiovascular function. Four structural components provide the skeleton for respiration and can modify the functional components: the central nervous system, chest bellows component, airway component, and an alveolar component.
Acute respiratory failure results from diverse causes affecting these functional or structural components. However, the final end result is an impairment of gas exchange resulting in either low blood oxygen content (hypoxemic respiratory failure), high carbon dioxide content (hypercapnic respiratory failure), or both. Clinical management involves identification of the failure or impending failure of respiration and emergency measures to support ventilation. The cause may be obvious or can require an extensive differential diagnosis if the patient can be resuscitated or stabilized.
Oxygenation and Ventilation During CPR
The arrested circulation requires both ventilation and gas transport to sustain vital organ function while attempts are made to establish a perfusing rhythm. Thus, both ventilations and compressions are important for patients in prolonged cardiac arrest, when the oxygen stores are depleted, and for patients in asphyxial arrest, such as children and drowning patients who were hypoxemic at the time of cardiac arrest.
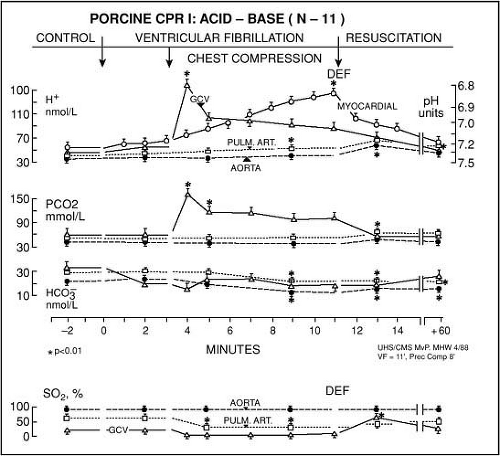
If the primary event is cardiac arrest, oxygen levels in the blood are normal and remain adequate for the first several minutes after cardiac arrest (Fig. 15.1). During the phase of early cardiac arrest, myocardial and cerebral oxygen
delivery is limited more by the diminished blood flow (cardiac output) than a lack of oxygen in the lungs and blood. For these reasons, during the first minutes of ventricular fibrillation (VF) sudden cardiac arrest (SCA), rescue breaths are probably not as important as chest compressions.1 In either situation the overall goal is return of oxygen to tissues and organs.
delivery is limited more by the diminished blood flow (cardiac output) than a lack of oxygen in the lungs and blood. For these reasons, during the first minutes of ventricular fibrillation (VF) sudden cardiac arrest (SCA), rescue breaths are probably not as important as chest compressions.1 In either situation the overall goal is return of oxygen to tissues and organs.
Important Lung–Thorax Relationships
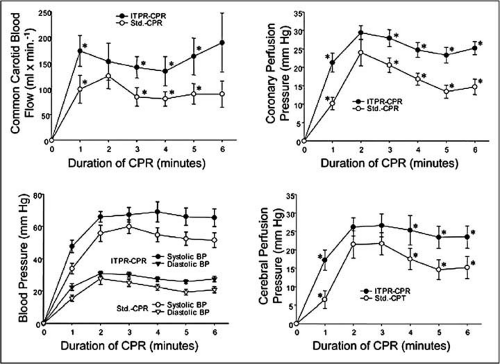
During normal ventilation, the mechanics of ventilation are very important. Elastic forces exist in the lung and chest wall that must be overcome by the respiratory muscles. During CPR, this elasticity returns the chest wall and lungs to their resting state and must be overcome by positive-pressure ventilation to deliver oxygen and remove carbon dioxide during mechanical ventilation and CPR. The resulting airway and transpulmonary pressures have a complex relationship, but the resulting net intrathoracic pressure can significantly affect blood flow during low-flow states such as shock and CPR. In one study, incomplete chest recoil preventing return to baseline intrathoracic pressures increased intrathoracic pressure, decreased coronary perfusion pressure, and decreased cerebral perfusion pressure.3 Increased intrathoracic pressure decreases both venous return and cardiac output. In a clinical study, about 50% of patients had incomplete chest relaxation at some point during CPR.4 In contrast, in an experimental situation, negative intrathoracic pressure significantly improved hemodynamics, vital organ perfusion pressure, and common carotid organ flow5 (Fig. 15-2). Whether these beneficial effects can be translated into patient survival is under current investigation.
Basic Principles of Ventilation in CPR
During CPR, blood flow to the lungs is substantially reduced, so an adequate ventilation–perfusion ratio can be maintained with lower tidal volumes and respiratory rates than normal.6 Excessive ventilation is unnecessary and is harmful because it increases intrathoracic pressure, decreases venous return to the heart, and diminishes cardiac output and survival.7
Tidal Volumes
Studies in anesthetized adults (with normal perfusion) suggest that a tidal volume of 8 to 10 mL/kg maintains normal oxygenation and elimination of CO2. During CPR, cardiac output is approximately 25% to 33% of normal,8 so oxygen uptake from the lungs and CO2 delivery to the lungs are also reduced.9 As a result, low minute ventilation (lower than normal tidal volume and respiratory rate) can maintain effective oxygenation and ventilation during CPR.10,11,12,13 During adult CPR, tidal volumes of approximately 500 to 600 mL (6–7 mL/kg) should be sufficient. Although a provider cannot estimate tidal volume, this guide may be useful for setting automatic transport ventilators and as a reference for manikin manufacturers. If providers generate a tidal volume sufficient to cause visible chest rise in adults, this will approximate the necessary tidal volume.
Optimizing Ventilation During CPR
Current controversy has emerged regarding the need for ventilation early in CPR and the optimal ventilation–perfusion ratio matching tidal volume and rate and cardiac output generated by chest compressions. Importantly, interruption of chest compressions decreased optimal hemodynamic parameters determining cerebral and myocardial blood flow.1
Ventilation Rate and Compression–Ventilation Ratio
The ideal compression–ventilation ratio to achieve an optimal ventilation–perfusion ratio during CPR has not been defined. Babbs and Kern evaluated the optimum ratio of compressions to ventilations in CPR using a mathematical model14 (Fig. 15-3




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree