The patient may grip the throat with one hand and the wrist with the other (‘the universal choking sign’). Sudden collapse with cyanosis while eating may mimic myocardial infarction (the ‘café coronary’).
TX
Get help. Encourage coughing in the responsive patient.
Figure 13.1 Treatment of a choking adult. 2010 Resuscitation Guidelines.
Reproduced with the kind permission of the Resuscitation Council (UK).
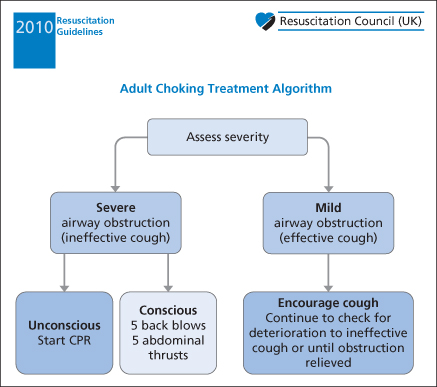
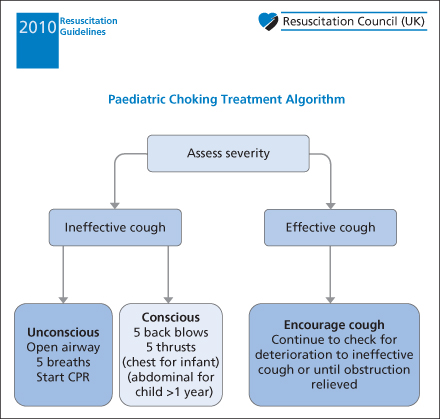
Figure 13.2 Treatment of a choking child.
Reproduced with the kind permission of the Resuscitation Council (UK).
Advanced life support entails careful judgement and an ascending hierarchy of treatment:
Complete airway obstruction that does not result from foreign material (e.g. obstruction due to oedema or tumour) will always require an artificial airway – either an endotracheal tube or a surgical airway.
Notes on 1–5 above:
 Box 13.1 The Heimlich Manoeuvre
Box 13.1 The Heimlich ManoeuvrePostasphyxial Care
All patients who have had an episode of choking should be admitted, often to the ICU. Those who remain dyspnoeic or have a depressed level of consciousness should be ventilated. Cerebral oedema is common after severe asphyxia; treatment with dexamethasone remains controversial.
Stridor and Partial Upper Airway Obstruction
Partial obstruction of the extrathoracic airways – at or above the cricoid ring – causes stridor, which is a harsh, high-pitched noise during inspiration. Intrathoracic obstruction causes wheezing. Characteristically, the patient is sat perched forward with the arms extended backward (the ‘tripod position’). Other signs of partial obstruction of the upper airway are:
- drooling of saliva
- hoarseness
- rattling noises in the upper airway
- snoring (in the unresponsive patient).
Pulmonary oedema may complicate prolonged obstruction. Also → Chapter 1, pp. 1–3.
The causes of partial obstruction of the upper airway are:
- inhaled foreign body
- allergic swelling of the airway (including insect stings)
- burns to the airway
- other direct trauma to the airway (rare) (note that dislocation of the cricoid cartilage may occur in children)
- infection of the larynx (including the epiglottis) or of the trachea
- infection of the mouth, tonsils or pharynx
- infection superimposed on congenital abnormality in a small infant. Congenital abnormalities of the airway usually present in the first few weeks of life but should be considered up to the age of 6 months.
XR
Radiographs should be obtained only in a stable, calm, well-oxygenated patient with an uncertain underlying diagnosis. The only appropriate films are anteroposterior (AP) chest and lateral soft-tissue view of the neck, performed in the ED.
A widened soft-tissue shadow on the lateral view of the neck may represent a retropharyngeal abscess or a swollen epiglottis. A coin in the trachea will have passed through the vocal folds in the sagittal plane and will thus appear end-on as a linear shadow on an AP CXR. In contrast, a coin in the oesophagus usually lies in the coronal plane.
Special problems in Children
TX
If there is marked stridor and cyanosis:
- Call for expert help immediately (anaesthetic and ENT specialists)
- Notify the operating theatre
- Reassure the patient and allow any position of comfort
- Give 100% oxygen or, better still, Heliox (70% helium with 30% oxygen) (helium has better flow characteristics than nitrogen or oxygen and may carry the oxygen through a small remaining passage)
- Try nebulised adrenaline (5 mg) as a temporary measure
- Consider parenteral adrenaline for allergic swelling.
If no help is available and the patient is about to die:
- Attempt laryngoscopy and endotracheal intubation – this is dangerous. Foreign material can be removed with suction and Magill’s forceps. If the anatomy of the pharynx is distorted by oedema, ask a colleague to squeeze the chest; escaping air bubbles will help to identify the position of the upper larynx.
- Be prepared to perform cricothyroidotomy or needle cricothyroid puncture (→ pp. 22–23).
In less urgent cases:
- Reassure the patient and allow a position of comfort
- Give 100% oxygen
- Obtain radiographs of the chest and lateral cervical spine in the resuscitation area
- Ask for ENT or paediatric advice. Be content not to make an immediate diagnosis in every case – looking for one may precipitate complete airway obstruction.
Management of Specific Upper Airway Conditions
Epiglottitis occurs in both children and adults but is often misdiagnosed in the latter. The Haemophilus influenzae type b (Hib) immunisation programme has led to a marked fall in the incidence in children but will have no effect on the adult disease, which is caused by different pathogens, such as staphylococci and streptococci. The clinical course can be dramatic and fatal.
THE LOWER AIRWAYS AND LUNGS
The restoration of adequate breathing is a priority, which is second only to the maintenance of a clear airway.
Respiratory Arrest
Isolated respiratory arrest or failure of ventilation in the presence of a clear airway and a central pulse occurs in four main circumstances:
It may also herald cardiac arrest in conditions such as a pulmonary embolism. The treatment is artificial ventilation with 100% oxygen until the underlying cause can be remedied.
Initial Assessment and Management of Acute Breathlessness
- Ensure that airway obstruction is not the cause of the dyspnoea.
- Give oxygen by mask (→ Box 13.2).
- Consider the need to support the ventilation:
- Check that the circulation is adequate, otherwise the situation is that of cardiorespiratory arrest.
- Sit the patient up, loosen clothing and briefly examine the chest.
- Obtain IV access.
- Monitor SaO2, ECG and BP.
- Score the level of consciousness (AVPU or GCS).
- Get a brief history.
- Obtain a CXR and ECG; check the blood gases (→ below).
- Consider immediate therapy for wheezing or pulmonary oedema.
 Box 13.2 Initial Oxygen Therapy in a Patient with Respiratory Distress
Box 13.2 Initial Oxygen Therapy in a Patient with Respiratory Distress| No to both | Give 100% oxygen |
| Yes to either | Give 24–35% oxygen until blood gas results (and more information) are available, keeping the patient’s SaO2 around 88–92% |
Like pain, shortness of breath must be relieved as soon as possible after initial assessment.
Investigations in Respiratory Distress
CXR (PA if Possible)
An anteroposterior CXR taken on the trolley in the resuscitation room may be necessary in a critically ill patient but is a poor substitute for a posteroanterior erect film because:
- the mediastinum and heart size are magnified
- fluid levels are not identified
- the penetration is often inappropriate
- the film is often rotated or incomplete
- there is a potential radiation hazard to staff.
 Box 13.3 Changes in the Lung Fields on a CXR
Box 13.3 Changes in the Lung Fields on a CXR- Metastases
- Lung abscesses
- Carcinoma of the lung
- Pulmonary infarcts
- Tuberculosis
- Rheumatoid nodules
- Hydatid cysts
- Blood: lung contusion
- Fluid: pulmonary oedema
- Consolidated pus: pneumonia
- Nodular: small in pneumoconiosis, larger in silicosis and sometimes miliary in TB
- Linear: fibrosis (usually lower zone), asbestosis, connective tissue disease and cryptogenic
- Cystic: seen in the lower zone in bronchiectasis and cystic fibrosis and in the upper zone in histiocytosis X
Twelve-Lead ECG
A rhythm strip from a three-lead ECG is insufficient for diagnostic purposes in a patient who may have subtle changes of myocardial ischaemia or pulmonary embolism.
Pulse Oximetry
Measurement of SaO2 is extremely valuable but has some drawbacks.
- It does not assess pH and PaCO2 which may both be abnormal in the presence of normal oxygen saturation.
- The steep fall of the oxyhaemoglobin curve means that SaO2 <95% is abnormal (cf. PaO2).
- SaO2 is inaccurate in the presence of carboxyhaemoglobin (COHb), which is not uncommon in respiratory distress (house fires, faulty gas heaters, heavy smokers).
Arterial Blood Gases
Estimation of the expected partial pressure of oxygen in an arterial blood gas sample → Box 13.4.
 Box 13.4 Estimation of the Expected Partial Pressure of Oxygen in an Arterial Blood Gas Sample
Box 13.4 Estimation of the Expected Partial Pressure of Oxygen in an Arterial Blood Gas Sample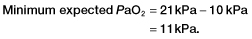
Foreign Bodies in the Lower Airways
Sudden onset of coughing and wheezing may accompany aspiration of a foreign body into the lower airways. Young children are especially vulnerable to this problem; a history of aspiration may be lacking. The right main, intermediate or lower bronchi are the most likely sites for obstruction to occur. Peanuts and toy fragments are the most commonly inhaled objects in children; bony food particles, broken teeth and small dental instruments predominate in adults. The presence of a unilateral wheeze, recurrent infection or other atypical symptoms and signs should always suggest the possibility of an intrathoracic foreign body.
XR
The foreign body is invariably radiolucent but the obstructive emphysema or absorption collapse that it causes may often be seen. Inspiratory and expiratory CXRs should be requested to demonstrate the ball–valve effect of a partial obstruction on the lung volume.
TX
All patients with a possibility of a foreign body in the airways should be referred for bronchoscopy. This would include those with suspicious histories, signs or radiological changes.
Asthma in Adults
Asthma continues to be a major health problem in the UK, affecting an estimated 1.4 million children and 3.7 million adults. It is responsible for the deaths of over 1500 people each year. Throughout western Europe, there is an average prevalence of asthma of 13% in children and 8.4% in adults, with a 2–4% annual increase in prevalence over the last 15–20 years. The reasons for this increase are uncertain but possible explanations include:
- a rise in the house-dust mite population
- increased diesel particulate emissions
- a decrease in exposure to bacterial pathogens in childhood
- changes in diet (more polyunsaturated fats and fewer antioxidants).
Patients with severe asthma and one or more adverse behavioural or psychosocial factors have a higher risk of death. For risk factors for developing near fatal or fatal asthma → Box 13.5. However, around 90% of asthma attacks that are severe enough to require admission to hospital develop relatively slowly over a period of 6 hours or more. Therefore, there is usually enough time for effective action.
 Box 13.5 Patients at Risk of Developing Fatal or Near Fatal Asthma
Box 13.5 Patients at Risk of Developing Fatal or Near Fatal Asthma- Previous near fatal asthma (e.g. required ventilation or had respiratory acidosis)
- Previous admission for asthma (especially if in the last year)
- Repeated attendances at ED for asthma (especially if in the last year)
- Asthma treatment requiring three or more classes of medication
- Heavy use of β2 agonists
- Brittle asthma
- Non-compliance with treatment, failure to attend appointments or self-discharge from hospital
- Psychiatric illness including depression and self-harm
- Current or recent major tranquilliser usage
- Alcohol or drug abuse
- Learning difficulties
- History of abuse in childhood
- Employment and income problems
- Severe domestic, marital or legal stress
- Social isolation
- Denial of illness
- Obesity
The clinical features of asthma result from a reversible inflammatory obstruction of the lower airways, which has three main components:
Asthma is caused by an allergic response to a wide variety of substances but there is usually an underlying sensitivity to house-dust mite. A viral infection is a common trigger for an acute exacerbation; exercise is responsible for around 40% of attacks.
Dyspnoea and wheezing are the predominant features. Bronchodilators may control these symptoms, but it is steroids that modify the underlying inflammatory processes.
Ask About
- When this attack started
- Improvement or deterioration in symptoms
- The patient’s assessment of severity
- What triggers an attack and how often
- Recent hospital admissions
- Any ICU admission
- Why this time was chosen to come to hospital; this is an important discriminator when considering discharge
- Previous and current drug use, especially steroids and theophyllines
- Other conditions, including upper respiratory tract infections and pregnancy.
If nebulised drugs were given before hospital arrival by the paramedics, precise details and initial peak flow rate should be noted.
Examination begins while taking the history and setting up the nebuliser.
Look For
- Difficulty with speech – spontaneous sentences or single words?
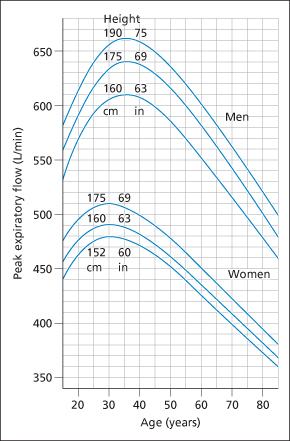
- Reduced peak expiratory flow rate (PEFR). For predicted values of PEFR for adults → Figure 13.3 and Box 13.6
- Tachycardia and tachypnoea
- Indrawing of ribs, flaring of nostrils and use of accessory muscles
- Wheezing and signs of pneumothorax
- Agitation, confusion or drowsiness
- Exhaustion
- Pyrexia
- Cyanosis.
 Box 13.6 Predicted Peak Expiratory Flow Rates for Adults of Average Height (in L/min)
Box 13.6 Predicted Peak Expiratory Flow Rates for Adults of Average Height (in L/min)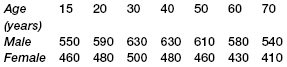
Investigations in Asthma
CXR is not indicated routinely in acute asthma. It should be requested only in cases of suspected pneumothorax, pneumomediastinum, pneumonic consolidation or inhaled foreign body. Patients with life-threatening asthma or failure to respond to treatment will also require a CXR as will those who have been intubated and ventilated.
Arterial blood gas analysis is required only in patients with features of life-threatening asthma and in those with an SaO2 (on pulse oximetry) <92%. There is usually a low PaCO2 as a result of hyperventilation and a low PaO2 caused by ventilation–perfusion mismatch. A normal PaCO2 is worrying and a high PaCO2 (>40–45 mmHg or 5.3–6.0 kPa) indicates respiratory muscle fatigue and impending respiratory failure. Measurement of blood gas tensions should be repeated after 2 h in all patients in whom the initial PaO2 was <60 mmHg (8 kPa) unless the SaO2 has risen to >92% in the meantime. Electrolyte estimation is important – hypokalaemia can occur – but haematological investigation is often unnecessary. A raised white cell count is to be expected with catecholamine and steroid therapy. Theophylline levels should be measured in patients who are taking regular methylxanthines at home.
The PEFR should be measured in all patients and used as a guide to treatment. PEFR expressed as a percentage of the patient’s previous best value is the most useful clinical parameter. In its absence, PEFR expressed as a percentage of the patient’s predicted value is a reasonable guide. For predicted values of PEFR for adults → Figure 13.3 and Box 13.6.
Life-Threatening asthma (PEFR 33% Best or Predicted)
Features include:
- unable to talk
- silent chest, cyanosis, feeble respiratory effort
- bradycardia, dysrhythmia or hypotension
- exhaustion, confusion or coma.
Pulse oximetry and arterial blood gas analysis show:
- SaO2 <92%
- PaCO2 within the normal range of 35–45 mmHg (4.6–6.0 kPa) or higher in near fatal asthma
- PaO2 >60 mmHg (8 kPa) irrespective of oxygen therapy
- Low pH.
TX
- Obtain anaesthetic/intensive care help immediately in life-threatening asthma.
- Give a high concentration of oxygen (at least 60%) via a well-fitting facemask. The aim is to keep the SaO2 >92%.
- Monitor SaO2, ECG and BP.
- Give salbutamol 5 mg (or terbutaline 10 mg) made up to 5 mL with 0.9% saline and nebulised by oxygen with a flow rate of at least 6 L/min. Add ipratropium 500 mcg to the same nebuliser. (This anticholinergic drug has been shown to produce additional bronchodilatation to that produced by β2 agonists alone, leading to faster recovery times and shorter durations of admission.)
- Give prednisolone 40–50 mg by mouth. If the patient cannot swallow oral medication or is vomiting, give IV hydrocortisone 100–200 mg 6-hourly. (Prednisolone 10 mg is roughly equivalent to hydrocortisone 40 mg.) Steroids should be continued for at least 5 days or until full recovery.
- Repeat the salbutamol/terbutaline and ipratropium nebulisers after 15 min. (The β2 agonists can be administered almost continuously; the ipratropium may be repeated at 4- to 6-h intervals.)
- Commence IV fluids.
- Give a single dose of magnesium sulphate 1.2–2.0 g by IV infusion over 20 min. For further information on magnesium → p. 250.
- Consider continuous administration of nebulised β2 agonists (i.e. repeated doses at 15- to 30-min intervals).
- Consider the use of IV salbutamol 200 mcg or IV terbutaline 250 mcg (given slowly over 10 min) for those patients in whom inhaled therapy cannot be used reliably.
- Consider (after consultation with senior staff) the use of IV aminophylline. This may benefit occasional patients with life-threatening asthma who are resistant to standard therapies. A loading dose of 5 mg/kg is given over 20 min under ECG control. This is followed by an infusion of aminophylline of 0.5–0.7 mg/kg per h. The loading dose (and possibly the idea of using aminophylline at all) should be abandoned in patients who are already taking oral methylxanthines. Caution is needed when giving aminophylline to patients who are hypoxic.
Intubation and ventilation may be required. All patients who are failing to respond to treatment should be referred to ICU specialists. This includes patients with worsening PEFR, deteriorating blood gases or acidosis, exhaustion, confusion or drowsiness.
IV adrenaline is sometimes used in a critical situation. Despite theoretical reasons for its efficacy, Heliox (helium and oxygen mixture in a 70 : 30 ratio) has not been shown to be of conclusive benefit in asthma. Similarly, non-invasive ventilation (NIV) is not recommended for the unstable situation of acute asthma.
Severe Asthma (PEFR Between 33% and 50% Best or Predicted)
Features include:
- inability to complete a sentence in one breath
- respiratory rate >25 breaths/min
- pulse rate >110/min.
TX
The patient should be treated as described for life-threatening asthma above, although IV magnesium should be given only if there is a poor response to inhaled bronchodilators. Aminophylline is unlikely to be considered. Admission is always required; the patient must be accompanied by a doctor or a nurse at all times.
Moderate Asthma (PEF Between 50% and 75% Best or Predicted)
The patient can finish a sentence and has no features of severe asthma.
TX
- Give salbutamol 5 mg (or terbutaline 10 mg) made up to 5 mL with 0.9% saline and nebulised by oxygen with a flow rate of at least 6 L/min.
- Monitor SaO2, ECG and BP.
- Wait 15–30 min after the initial nebuliser and then repeat the PEFR.
- If the patient is worse and PEFR <50% treat as severe asthma. If better and PEFR >75% consider discharge (→ below). If PEFR is still between 50% and 75% repeat the salbutamol or terbutaline nebuliser and give prednisolone 40–50 mg orally. Then wait a further 30 min.
- If the patient is worse and PEFR <50% treat as severe asthma. If better and PEF >75% consider discharge (→ later). If the same (i.e. PEFR 50–75%) wait a further 60 min while monitoring the SaO2, heart rate and respiratory rate.
- If, at this point, the PEFR <50% treat as severe asthma. If PEFR >50% and the patient is stable or improving, consider discharge (→ later).
Mild Asthma (PEFR >75% Best or Predicted)
- The patient can talk normally.
TX
The patient should be given his or her usual bronchodilator and then kept under observation for at least 30–60 min. If the PEFR remains >75% consider discharge (→ later). If the PEFR falls, treat as described in the appropriate section above.
Discharge of a Patient with Asthma
Most patients who are sufficiently ill to request emergency help with their chronic condition will require oral steroids (as well as inhaled steroids and bronchodilators as part of a long-term management plan). Prednisolone 40–50 mg given orally for 5 days is usually adequate. (If used within an hour of ED arrival, steroid tablets are effective at preventing admission and reducing the risk of relapse in the ensuing 21 days. Despite this, they are not always prescribed by ED staff.) There are several alternatives for high-dose inhaled steroids:
- Beclometasone 400–500 mcg twice daily
- Budesonide 400–500 mcg twice daily
- Fluticasone 250 mcg twice daily.
These doses are halved for children.