192 Rash in the Severely Ill Patient
• Identification of rash morphology is paramount for elucidating the differential diagnoses of potentially lethal rashes.
• History taking must include occupation, travel, medications, comorbid conditions, and immune status.
• Complete and serial physical examinations are needed for proper evaluation of any patient with a potentially lethal rash.
• Blood cultures and early antibiotic administration are crucial because most potentially lethal rashes have an infectious cause.
• The clinical manifestations of Rocky Mountain spotted fever and meningococcemia are very similar. With any diagnostic uncertainty, treat for both.
• Petechial and purpuric rashes are marked by high morbidity and mortality.
• Petechiae and fever are very concerning. These patients may decompensate rapidly and require aggressive care.
• Palpable petechiae are due to vasculitides and may have an infectious cause.
• Nonpalpable petechiae are most often associated with thrombocytopenia.
• Hemorrhagic bullae are ominous.
• Patients with toxic epidermal necrolysis and other skin-sloughing diseases desquamate extensively and may require admission to a burn unit.
Presenting Signs and Symptoms
History Taking
The history is of paramount importance in the diagnosis of a patient with a rash. Of particular concern is an accounting of any recent travel, the patient’s own geographic location, medical and occupational history, animal exposure, and medication regimens. Table 192.1 classifies rashes in severely ill patients by exposure to geographic regions and animals.
Table 192.1 Rashes in Severely Ill Patients by Geographic and Animal Exposure
| DISEASE | DISEASE HIGHLIGHTS | |
|---|---|---|
| By Geographic Exposure | ||
Northeastern  of United States of United States | Lyme disease | |
| Caribbean | Dengue fever | |
| Continental U.S. except Vermont and Maine | Rocky Mountain spotted fever | |
| Colombia | “Tobia fever” | |
| Brazil | “Sao Paulo fever” | |
| Mexico | “Fiebre Manchada” | |
| By Animal Exposure | ||
| DISEASE | DISEASE HIGHLIGHTS | |
| Farm animals, especially pregnant ones: cattle, goats, sheep | Q fever | Maculopapular truncal rash (20%); usually present with culture-negative endocarditis |
| Rats | Rat-bite fever | Constitutional symptoms, endocarditis, hepatitis, enteritis, and a rash around an open sore that may spread and appear red or purple; ulcerations of the hands and feet; wounds are slow to heal and may recur |
| Herbivores (plant eaters): buffalo, cattle, horse, deer, goat, rabbit, sheep, birds | Anthrax | Boil-like lesion that forms an ulcer with a painless black eschar Exposure to infected or dead animals or their products |
| Bioterrorism | ||
Physical Examination
At the start it is very important to evaluate the vital signs of toxic-appearing patients with rashes. Fever and hypotension are of particular concern and mandate expedited and intensive care. A complete examination should include evaluation for any new-onset heart murmur, changes in mental status, and nuchal rigidity. Of particular importance are the onset and progression of the rash; involvement of the palms, soles, and mucous membranes; and the age of the patient. An algorithmic approach can aid greatly in the identification of systemically ill patients with a rash. Table 192.2 categorizes rash characteristics in severely ill patients.
Table 192.2 Rash Characteristics in Severely Ill Patients
| Centripetal progression | RMSF, EM major |
| Centrifugal progression | Viral exanthems, smallpox |
| Rash with palm and sole involvement | EM, RMSF, bacteremic endocarditis, syphilis, erythroderma |
| Rash with mucous membrane involvement | EM major, TEN, SJS, pemphigus vulgaris, syphilis |
| Rash with rapid spread | Urticaria, anaphylaxis, meningococcemia, erythroderma |
| Rash with hypotension | Meningococcemia, TSS, RMSF, TEN, SJS |
| 0-5 yr | Meningococcemia, Kawasaki disease, viral exanthems |
| >65 yr | Bullous pemphigus, sepsis, meningococcemia, TEN, SJS, TSS |
EM, Erythema multiforme; RMFS, Rocky Mountain spotted fever; SJS, Stevens-Johnson syndrome; TEN, toxic epidermal necrolysis; TSS, toxic shock syndrome
Physical Signs
Two signs are important in the evaluation of these rashes, the Nikolsky sign and the Asboe-Hansen sign. A positive Nikolsky sign (Fig. 191.1) is noted when slight rubbing of the skin results in exfoliation of the outermost layer with lateral extension of the erosion into intact skin. The area of denuded skin is pink and tender. The Asboe-Hansen sign (indirect Nikolsky sign or Nikolsky II sign) is extension of a blister into normal skin with the application of light pressure on top of the blister. All patients with tender, blistering, or sloughing skin should be evaluated serially for these important signs.
Differential Diagnois and Medical Decision Making
Algorithmic Approach to Classification
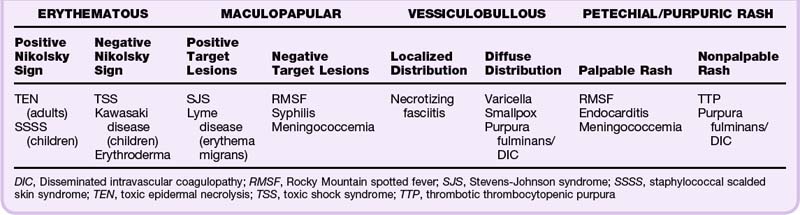
It is helpful to first define the rash into one of four types: erythematous, maculopapular, vesiculobullous, or petechial/purpuric (see Chapter 191 for more detailed review). Erythematous rashes can then be further classified into those with or without a positive Nikolsky sign. Maculopapular rashes may be subdivided into those with or without target lesions. Vesiculobullous rashes should be differentiated into those with a localized or a diffuse distribution. Petechial/purpuric rashes should be classified into those with palpable or nonpalpable rash morphology (Table 192.3).
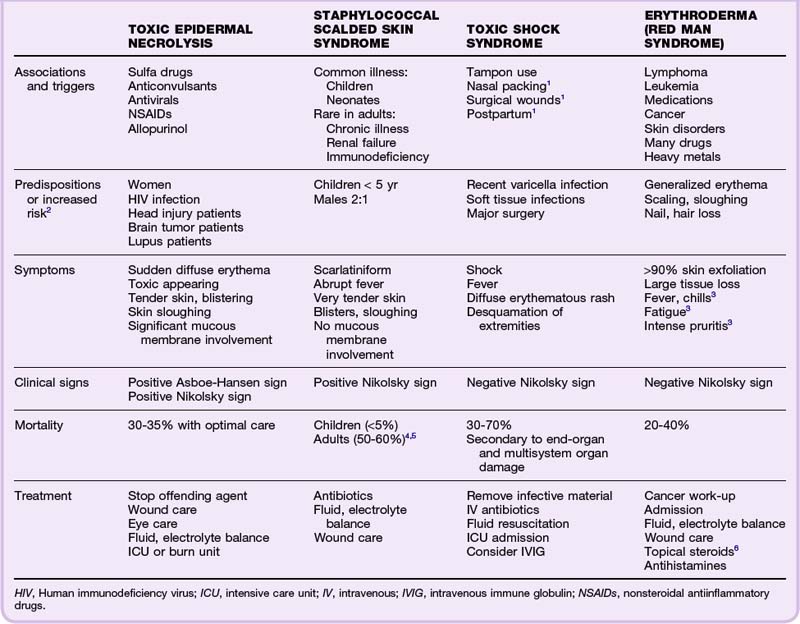
Erythematous Rashes
Toxic patients with an erythematous rash may have specific signs that narrow the differential diagnosis. The combination of an erythematous rash in a toxic patient with a positive Nikolsky sign reduces the differential diagnosis substantially, usually to toxic epidermal necrolysis (TEN) in adults and staphylococcal scalded skin syndrome (SSSS) in infants and young children. Alternatively, the differential diagnosis for toxic and febrile patients with an erythematous rash as well as a negative Nikolsky sign includes toxic shock syndrome (TSS), Kawasaki disease, and erythroderma (see Table 192.3). Table 192.4 details the symptoms, signs, mortality, and treatment of the aforementioned erythematous rashes. SSSS, TSS, and Kawasaki disease are also covered in Chapter 18.
Toxic Epidermal Necrolysis
TEN (Lyell disease) is the most serious cutaneous drug reaction. It is most commonly associated with sulfa drugs; however, it has other important triggers as well. TEN is manifested as the sudden onset of diffuse erythema with tender skin and blistering. The skin cleavage is full thickness with positive Nikolsky and Asboe-Hansen signs and significant skin sloughing (Fig. 192.1). These patients are toxic and exhibit significant mucous membrane involvement. Symptoms occur first around the eyes, spread caudally (shoulders and upper extremities), and then progress to involve the entire body. Several populations are predisposed to TEN and others are at high risk (see Table 192.4). However, one group deserves expanded mention. It is important to consider that patients infected with human immunodeficiency virus (HIV) who are on a chronic regimen of trimethoprim-sulfamethoxazole prophylaxis and other polypharmacy have a 1000 times greater risk for TEN than do those without HIV.2,7
Staphylococcal Scalded Skin Syndrome
Also known as Ritter disease or dermatitis exfoliativa neonatorum,4 SSSS is manifested as a scarlatiniform, erythematous rash caused by a staphylococcal infection that blisters and sloughs (positive Nikolsky sign). Children younger than 5 years are at highest risk.
Kawasaki Disease
This childhood illness is also known as mucocutaneous lymph node syndrome or infantile polyarteritis. It is a vasculitis of unknown cause, although infective and autoimmune theories abound. It affects many organ systems, including the skin, mucous membranes, lymph nodes, and blood vessels. Diagnostic criteria include high fever for at least 5 days, diffuse erythroderma of the skin, strawberry tongue, significant cervical lymphadenopathy, conjunctival injection, peeling of the fingers and toes, and edema of the extremities.8 Thrombocytosis may also be present. By far the most serious complication is vasculitis of the coronary arteries, which leads to coronary vessel aneurysms, myocarditis, and myocardial infarction (even in the very young). Treatment consists of high-dose aspirin (given immediately), hospitalization with supportive care, and very importantly, intravenous immune globulin (IVIG) because Kawasaki disease does not respond to antibiotics.8,9
Erythroderma
Erythroderma, also known as exfoliative dermatitis, is an erythematous, scaling rash that involves more than 90% of the skin.10 Erythroderma is also termed red man syndrome when a primary cause cannot be identified.10 The rash begins as a very generalized erythema. The skin begins to scale and slough, along with nails and hair.11 The skin is inflamed and may lose pigmentation in dark-skinned individuals. This is an overwhelming disease process in which large tissue burdens of exfoliated scales are lost en masse daily; these patients are, in essence, “burn victims.” They have marked increases in skin perfusion and profound temperature dysregulation that result in significant heat loss, increased basal metabolic rate, fluid loss, edema, and hypoalbuminemia.10 Although this disease primarily affects adults, it does occur in younger populations who have other skin or connective tissue disorders (lupus, sarcoid, psoriasis, SSSS, atopic dermatitis, or seborrheic dermatitis). Patients with rapid disease progression usually have a history of cancer or SSSS or an inciting medication reaction. Those with gradual symptomatology generally have a skin disorder history. The work-up for these patients should be conducted in close consultation with a dermatologist, who can aid in identification of the primary lesions, which can be a difficult task. All patients warrant cancer evaluation and treatment of the underlying cause. Laboratory studies include a sedimentation rate, complete blood count, comprehensive metabolic panel, HIV testing, skin scrapings, skin biopsies, and wound cultures.6 All patients warrant admission. In pediatric patients, erythroderma and fever are predictors of hypotension and may reflect TSS.12 Systemic steroids are controversial and may worsen psoriasis and SSSS. Recovery is long and recurrences common in the case of red man syndrome. Mortality ranges from 20% to 40% and in many instances is due to factors unrelated to the disease process itself.3,13
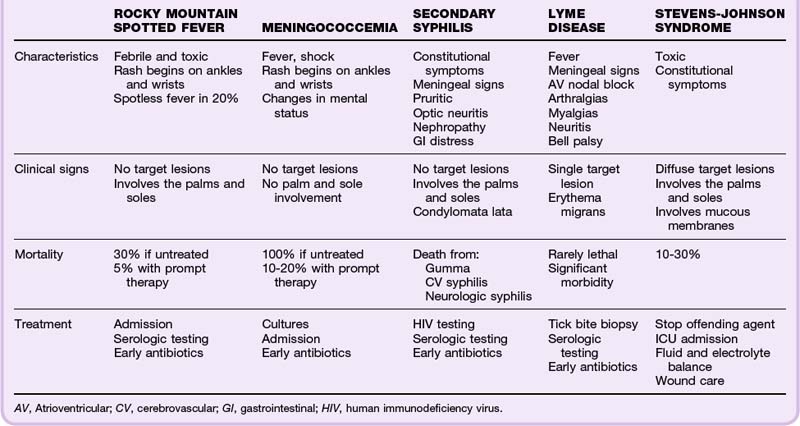
Maculopapular Rashes
The term maculopapule is a portmanteau of macule and papule. Maculopapular rashes are differentiated according to the distribution of the rash and systemic toxicity (Table 192.5). Patients who appear toxic and febrile have a wide differential diagnosis; however, it is paramount that patients living in endemic areas be assessed for Lyme disease. Target lesions (see Fig. 191.4) are pathognomonic for Stevens-Johnson Syndrome (SJS) and erythema multiforme (EM). Refer to Chapter 191 for review of EM. A full discussion of TEN was presented in the previous section (erythematous rashes); however, TEN and Lyme disease may also be associated with target lesions. Toxic patients with a maculopapular rash but no target lesions require emergency evaluation for Rocky Mountain spotted fever (RMSF), syphilis, and meningococcemia (see Table 192.3).
Stevens-Johnson Syndrome
SJS is often a drug reaction, although infections and malignancies have been implicated. Previously, SJS was thought to be linked with EM, but it has recently been reclassified on the spectrum with TEN.2 These patients have diffusely distributed target lesions that include the palms and soles. Significant mucous membrane involvement is present as well (Fig. 192.2
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree