221 Pursuit of Performance Excellence
Organizations consist of numerous parts, systems, and functions all operating and, ideally, collaborating to produce an end result, one that is not always desired. Unlike the organs of the human body, in healthcare delivery, different components often struggle to operate in a coordinated and symbiotic fashion. Systems such as pharmacy, lab billing, ICU, operating room, emergency department, internal medicine, surgery, and graduate medical education programs frequently operate independently without the coordination necessary to produce reliably integrated operations. The parts seem more independent than interdependent, more competitive than cooperative, and more focused on their own efforts than on the results of the whole. Whereas each part has to remain viable and effective in order to contribute to the overall goals and purpose of the organization, all parts must operate in harmony for superior performance to be achieved and maintained. Using the Baldrige Performance Excellence Program (BPEP or Baldrige) as a framework (Figure 221-1), this chapter provides guidance on how to design and manage the ICU to improve patient outcomes and be a great part of the larger hospital system. The Baldrige framework is elaborate, and a full presentation is beyond the scope of this chapter. A complete guide to the framework can be found at www.baldrige.org.
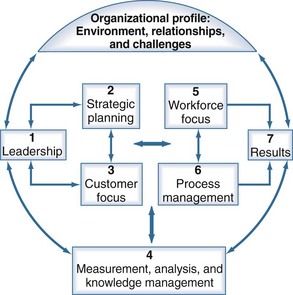
Figure 221-1 Baldrige healthcare criteria for performance excellence framework: a systems perspective.
(Adapted from www.baldrige.org.)
 Background and Overview
Background and Overview
Differentiation of High Performance Versus Average Performance or Scoring Guidelines
 The Baldrige Intensive Care Unit
The Baldrige Intensive Care Unit
Category 1: Leadership
The criteria for leadership are instructive as they relate to ICUs and are likely very different from the current approach. Within the ICU, opportunities exist for the leadership team to become a more instructive leadership system (Figure 221-2) and promote a unit that demonstrates repeatable and fully deployed process across all areas of delivering ICU care. The leadership team ensures consistency of care across boundaries, incorporates and supports continuous cycles of improvement and/or innovation, and strategically aligns with the overall goals and objectives of the hospital.
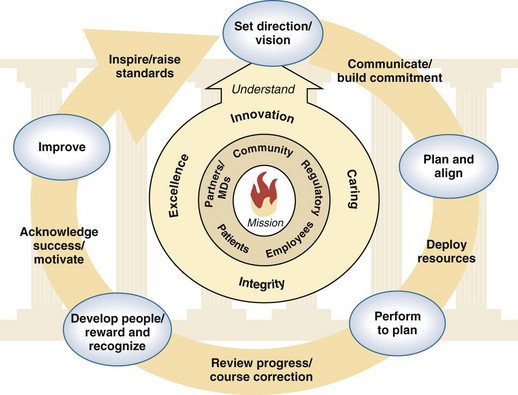
Figure 221-2 Example of a leadership system (Sharp Healthcare, San Diego, California).
(Adapted from 2007 National Baldrige Application.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




