Fig. 17.1
Anatomical illustration depicting the inguinal ligament, adductor longus and rectus abdominis with their respective “forces” on the pubic tubercle
Clinical examination therefore relies on testing all the possible differentials [13]: femoroacetabular impingement (FAI), labral tears, adductor tendinopathy, osteitis pubis and a symphyseal injury
A thorough assessment of the hip and adductor strengths is essential as well as testing a patient’s balance, spinal curvature and of course groin tenderness, especially along the inguinal canal and pubic tubercle. PIPS can then be diagnosed if the three out of five clinical signs exist as per the Manchester consensus statement [3].
17.2.2 17.2.2 Hip-related Pain
Pathology of the hip joint is a well-recognized cause of groin pain. The most common cause in the athletic population is femoroacetabular impingement (FAI). This is a condition where there is an abnormality in the shape of either the femoral head or the shape or position of the acetabulum.
In males, the most common pathology is a prominence at the head-neck junction called a cam deformity. As the hip flexes up, this prominence impacts against the bony rim of the acetabulum and the soft cartilaginous rim (labrum) that is attached to it. Repeated flexion can cause labral tears and shear stresses at the chondrolabral junction, which in turn can lead to cartilage delamination and joint degeneration. The etiology of both pathologies is not though fully understood. The presence of a symptomatic cam deformity does seem to be more common in the athletic population [14] and probably begins to form in early adolescence. It is more commonly seen on the right hand side as that tends to be the dominant side [15]. Pincer abnormalities also start to develop in adolescence and may be associated with a gradual change in acetabular orientation as the person matures [16].
It is clear that the development of symptomatic impingement requires a combination of factors: combining an anatomical abnormality with both the type and level of activity.
Symptomatic hip impingement is most common in certain sports such as distance running, football, rugby, squash and martial arts [17,18]. All of these involve repetitive loading and unloading of the hip. It is less common in nonimpact sports such as swimming and cycling as noted above. Interestingly, it is also common in sports such as gymnastics and ballet, but this may be due to impingement occurring secondary to an abnormal hip range of movement, rather than the presence of significant cam or pincer deformities [15].
Patients usually present with deep-seated antero-lateral groin pain. It tends to be in the middle or just lateral to the mid-inguinal point and exacerbated by exercise. It is not affected by coughing or raised intra-abdominal pressure, which does differentiate it from PIPS. When present for some time, it can be associated with soft-tissue pain and tendinopathy in the surrounding musculature. Patients can often present with an associated anterior clicking as the leg moves from flexion to extension and this is usually due to a psoas tendinopathy. As well as this, it is relatively common for patients to have associated pain in their lower back, sacro-iliac joint and tendinopathy in the gluteal, sartorius and adductors regions.
Clinical examination can confirm the presence of soft-tissue tenderness, and deep hip flexion, particularly with internal rotation and adduction, will often trigger the presenting pain.
Finally, because it is well recognized that it is possible to have FAI features but be asymptomatic, the use of intra-articular local anaesthetic injections (plus or minus steroids/hyaluronic acid) can be a very useful diagnostic tool in differentiating hip and inguinal pain [19].
There have been increasing numbers of published papers looking at patient outcome following hip arthroscopy for FAI. Initially, these tended to be single surgeon series with an emphasis on athletes and showed improved outcomes with good return to sport. Recently there have been a number of reviews looking at both athletic and non-athletic patients. These have shown significant improvement across both groups with regard to return to activity, as well as improvement in patient-reported outcome measures (PROMs).
17.2.3 17.2.3 Adductor-related Pain
On clinical evaluation, pain elicited over the inguinal ligament is more indicative of inguinal-related pain (PIPS) with more inferior pain suggestive of an adductor-related pathology [20], although it is accepted that an adductor tendinopathy can coexist with PIPS in as many as 50% of the patients [21]. As already mentioned, sports that require the strong eccentric contraction are more likely to promote a groin injury and this is especially true for adductor injuries [22]. The main action of the adductor muscle group is to adduct the thigh in the open kinetic chain and stabilize the lower extremity to any changes in all planes of motion in the closed kinetic chain. The adductor longus is the most likely muscle in this group to be injured [23]. It may be that the adductor longus’s lack of mechanical advantage (due to its anatomical origin and insertion) possibly renders it more susceptible to a strain. As discussed later, the need to strengthen and improve the stability of the adductor muscle group becomes essential in reducing the time an athlete spends away from their sport as well avoiding the need for any operative intervention [24].
17.3 17.3 Imaging Investigations
The diagnosis and correct management of the sports-related groin pain, PIPS, is extremely challenging for the practising clinician who is reliant on both clinical skills and imaging findings. It is therefore vital that all relevant clinical information is known when performing and interpreting any radiological investigations. The referring clinician should be aware that not all positive imaging findings present on ultrasound or magnetic resonance imaging (MRI) are clinically important and that they can be found in an asymptomatic individual [11].
This section provides an overview of current radiological terminology with description and imaging findings and our diagnostic approach in processing the information from the history, clinical examination and imaging findings to formulate an optimal management plan.
The pubic symphysis represents the important cross-link between the strong adductor muscle complex and the anterior abdominal wall muscles and tendons. It is thus not unsurprising that the pubic bone often shows changes in sporting individuals and is often mislabeled as a diagnosis of osteitis pubis which is better reserved for females per partum where a more correct term of non-athletic osteitis pubis should be used (Fig. 17.2).


Fig. 17.2
MRI showing a footballer with a right pubic body stress response (arrow)
In the sporting athlete it is best practice to describe the bone marrow signal pattern observed on MRI with a common parasymphyseal bony oedema pattern, which is seen as an incidental finding with young footballers, but more diffuse bony oedema through a pubic body is a more positive finding.
The pubic symphysis is a secondary cartilaginous joint and with time it can develop a central cleft within its central fibrocartilage which is termed the primary cleft. This primary cleft may communicate with a secondary cleft which is an acquired cleft formed by separation of the short adductors (adductor brevis and gracilis) from their bony attachments to the pubis. The secondary cleft is a description of partial tendon avulsion; it is a common finding in sporting athletes and it can be difficult to determine whether this represents an important finding that is responsible for the individual’s current symptoms or an incidental finding from a previous injury (Fig. 17.3).
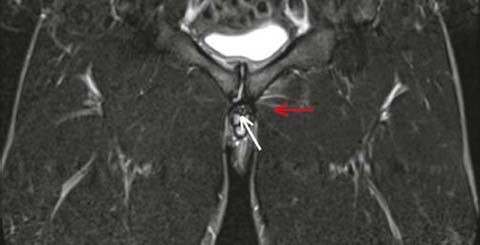
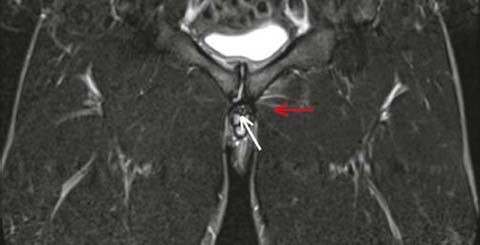
Fig. 17.3
MRI image showing a footballer with a right secondary cleft (white arrow) and a left adductor brevis grade 1 muscle strain (red arrow)
A further sign — the superior cleft sign — described where there is a cleft of high signal arising from the superior most tendinous attachment of the adductor longus to the pubic bone represents partial separation of the adductor longus and its aponeurosis from the superior pubic tubercle (Fig. 17.4).


Fig. 17.4
MRI showing a right superior cleft sign (arrow)
These acute tears or adductor tendinous avulsions can be associated with bony oedema within the underlying bone.
Plain radiographs are useful to demonstrate gross degeneration or abnormalities of hip shape. More advanced imaging such as MR arthrography can reliably detect the presence of labral tears as well as early articular cartilage damage [25].
Ultrasound and MRI can be used to assess weakness of the posterior inguinal wall.
On MRI a hernial sac may also be visualized and strain scans can be performed but ultrasound is better suited in the assessment of the inguinal region for posterior inguinal wall weakness or disruption.
An ultrasound examination with graduated valsalva technique and forced valsalva are helpful in assessment for weakness of the posterior inguinal wall just medial to the deep inguinal ring; femoral hernia, although less common, can be also easily identified.
17.4 17.4 Management
17.4.1 17.4.1 Physiotherapy
Returning the athlete with groin pain back to sport is the aim of any physiotherapy programme.
To treat a sportsperson’s injury the physiotherapist must recognize and be aware of the demands of the individual sport concerned especially once a more chronic PIPS condition is diagnosed.
Unfortunately, often the culture in sport is for the player not to report the pain until it is affecting their function and even then it does not limit their ability to train or play so they may well continue until the pain is too much; therefore, the actual true incidence of groin pain is unknown and it varies from sport to sport [26, 27].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






