Psychological Problems in the Ventilated Patient: Introduction
Psychological and psychiatric disturbances occur frequently in mechanically ventilated patients, and cause patients, their loved ones, and their caregivers considerable distress. This chapter familiarizes the reader with commonly observed psychological and psychiatric symptoms in ventilated critically ill patients; briefly discusses the challenge of making a psychiatric diagnosis in the context of the ventilated patient; and describes what is known of the three disorders most commonly described in this patient population: delirium, depression, and posttraumatic stress disorder.
Traditional psychological and psychiatric assessments in the adult patient rely on the patient’s ability to engage in conversation. Baseline psychological health and personality, a patient’s relationship with his or her acute or chronic illness, a patient’s emotional response to it, and the clinical context in which the patient is placed are typically considered in this evaluation. Assessment of the psychological and psychiatric state of a mechanically ventilated patient is hindered by the presence of an endotracheal tube, which makes verbal communication impossible. A tracheotomy with a talking valve, and a face mask, also limits speech. Beyond problems of verbal communication, the sudden and dramatic onset of a ventilated patient’s illness, the use of pharmacologic sedation, the layout of an intensive care unit (ICU), and a critical care physician’s unfamiliarity with psychological assessments have hampered descriptions of psychiatric and psychological issues.
Psychiatric diagnoses are made on the basis of clinical criteria. These criteria were, for many decades, highly variable depending on a school of thought and geographical provenance. Lobotomies, incremental electroshock therapy to re-create neuropsychiatric normalcy, and insulin-coma treatments exposed psychiatric professionals to scientific and public criticism. Over the last 40 years, psychiatric diagnoses have been structured more rigorously by experienced psychiatrists based on symptom and disease classifications through the use of systems such as the International Classification of Diseases (ICD) from the World Health Organization, and the Diagnostic and Statistical Manual of Mental Disorders (DSM) from the American Psychiatric Association. The tenth revision of the International Statistical Classification of Diseases and Related Health Problems (ICD-10) was published in 1991; the fourth revision of the Diagnostic and Statistical Manual of Mental Disorders, DSM-IV-TR, was published in 2000. The ICD-11 is expected in 2011 and the DSM-V update is anticipated in 2013.
The ICD-10 and the DSM-IV-TR rely on diagnostic criteria compiled by expert psychiatrists and, in the case of the DSM-IV, on the basis of described and published patient symptoms. Two problems become apparent when applying these diagnostic criteria to critically ill patients. The first is the challenge of applying diagnostic criteria to a mechanically ventilated patient if the symptom constellations have been gathered in a different—usually ambulatory—population. Apathy, for instance, a feature of depression, may be expected in a septic ventilated patient receiving propofol, making its value as a diagnostic criterion of depression in this context uncertain. The second is that these DSM or ICD criteria have not been investigated in terms of validity in ventilated patients, whether acutely or chronically ill, nor are the criteria correlated with outcomes in such patients.
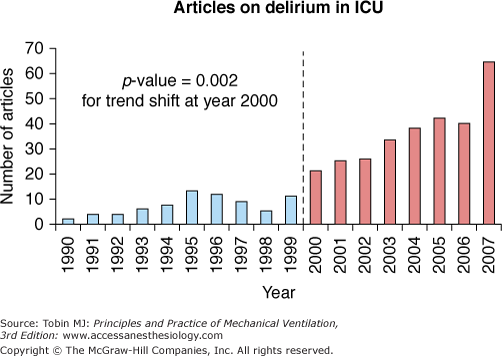
Psychiatric or psychological disturbances in the ventilated critically ill patients have been given many names, such as ICU psychosis, septic encephalopathy, and apathy. Semantic descriptions for disorders such as delirium1 vary by geographic region. Over the last decade, publications on psychiatric topics such as delirium in ventilated patients have increased significantly (Fig. 54-1). Two factors may have influenced this change. Two intensivist-led publications in 20012,3 sensitized clinicians to the notion of screening ventilated patients for delirium through the use of simple screening tool, applicable at the bedside. More delirium-related publications followed, with subsequent interest in other psychiatric and psychological disorders, such as depression and posttraumatic stress disorder. Almost simultaneously, researchers with an interest in ICU outcomes in adult respiratory distress syndrome (ARDS), whose focus was initially on respiratory physiology, realized the main impediments to recovery for these patients were myopathy and psychological distress.4,5 Three psychiatric syndromes—delirium, depression, and posttraumatic stress disorder—have since been identified with increasing frequency 6 in ventilated critically ill patients and ICU survivors.7 The associations between these diagnoses and poor outcomes, including length of stay, quality of life, and cognitive impairment, have led to a cry for pharmacologic intervention for delirium by interventionists, and for further longitudinal studies8,9 by those interested in the sequelae of what had traditionally believed to be rapidly reversible (and almost irrelevant) disorders.
Figure 54-1
The number of publications on delirium in the critical care setting (in mechanically ventilated and nonmechanically ventilated patients) over 17 years. (Modified, with permission, from Morandi A, Pandharipande P, Trabucchi M, et al. Understanding international differences in terminology for delirium and other types of acute brain dysfunction in critically ill patients. Intensive Care Med. 2008;34:1907–1915.)
What is understood of these three psychiatric syndromes is limited by the dearth and relative novelty of literature on the topic.10 Current knowledge should be considered in light of the methodological limitations in establishing a diagnosis as described above.
Most publications reviewed for this chapter are focused exclusively or largely on mechanically ventilated patients, a group that some authors argue is particularly susceptible to psychiatric complications, such as delirium.11 Information from nonventilated patients is discussed if it is consistent with what has been published on ventilated patients, but only if it provides insight not available from the literature on mechanically ventilated patients per se. Reviewed studies are limited to critical care and stepdown units; studies in patients receiving home ventilation or chronic ventilation on a hospital ward or a specialized institution were not considered. The disproportion between the delirium literature in critical care and that describing other syndromes, which is more modest, explains the discrepancy in content herein.
Diagnostic and Contextual Challenges
Unsurprisingly, publications on the subject of psychological and psychiatric disorders in ICU patients have been driven by the medical perspective of the psychiatric diagnosis. Most physicians attempt to classify psychological or psychiatric symptoms as diseases, with attributable biologic alterations and reproducible symptoms. Medical culture12 drives a rigid medical approach, and a rationalization of “disease”; the narrow view of biologic alterations and their diagnostic criteria is the focus of what we publish and read. Dimensions such as illness (the patients’ perception of the self) and sickness (the social dimension and impact of the diagnosis, particularly a psychiatric one) are seldom addressed. In settings outside critical care, caregivers understand that a patient’s well-being depends on psychological integrity. Such well-being, and perhaps even the will to survive, are hindered if the patient is unable to recognize his or her own self during disease, or if that very self is compromised, a common occurrence in the foreign, disturbing, and overwhelmingly technological setting of the ICU. This wretchedness is complicated by a complete dependence on machines and personnel. What little autonomy a patient retains is seldom fostered or encouraged. The relationship with the caregiver, or a significant person in the patient’s life, also contributes to healing, or to a more serene journey toward death. The social impact of a psychological or psychiatric disease may interfere with this patient–caregiver or patient–significant person relationship, and constitute a dimension of “sickness.” Establishing a diagnosis of depression and delirium requires descriptors; the dimensions of illness and sickness, however, may be what cause the greatest distress. Patient recovery and postdischarge outcomes may be related to these dimensions of illness and sickness; however, our limited understanding of these facets as experienced by patients, their caregivers, and loved ones limits a global understanding of the psychological and psychiatric issues and precludes a holistic approach to care.
Furthermore, context is important in establishing whether endogenous or exogenous factors trigger psychiatric or psychological disturbances. Some psychiatric diagnoses can be made with clarity. For instance, mania in an ambulatory outpatient has in many cases a recognizable pattern, associated biochemical abnormalities, and a predictable response to medication. Syndromes such as depression can come from within, or be considered a normal response (in grieving, for example). Other mood states such as anxiety range from normal to pathologic, and have not been defined in the critically ill. Several symptoms (sadness, paranoid delusions, or harrowing flashbacks) could, arguably, be considered contingent, temporary, and normal responses to painful, traumatic, or near-death experiences. Overlapping syndromes of delirium and depression have been described.13,14 The administration of psychotropic drugs in high doses over prolonged periods of time adds an important confounder, as do personality traits and the amount of cognitive reserve. This issue of context makes the attribution of a psychiatric diagnosis to a set of symptoms particularly challenging in the critical care setting. Dialog is a key element in differentiating these factors as potential contributors, in establishing the diagnoses, and in proffering expression as a form of early therapeutic intervention. Verbal dialog is challenging in the context of mechanical ventilation. Weakness, which precludes movement, facial expression, or both, further challenges (or is perceived as challenging) the examiner and contributes to the real or perceived barriers to communication.
Delirium
The patient you spoke to and communicated with yesterday on ICU rounds is a little more difficult to rouse this morning. When you approach him, he initially looks surprised and frightened; as you introduce yourself and remind him of yesterday’s conversation, he appears uncertain of who you are and of his surroundings. As you continue speaking, he looks away and appears to stare at something on the ceiling. The nurse reports that a few hours earlier he was grasping at what appeared to be imaginary objects in front of him. He did not sleep last night.
Delirium, with its traditional symptoms described here, frightens patients. The delusions and hallucinations they experience transiently and usually for the first time in their lives are upsetting; paranoid thoughts are common. When cognitive function normalizes in the fluctuating course that characterizes delirium, patients wonder if they are losing their minds and if they will ever return to the way they were before. Because 40% of patients present symptoms only between midnight and 8 am, careful attention to the nurse’s report of a patient’s behavior is helpful in recognizing the problem.
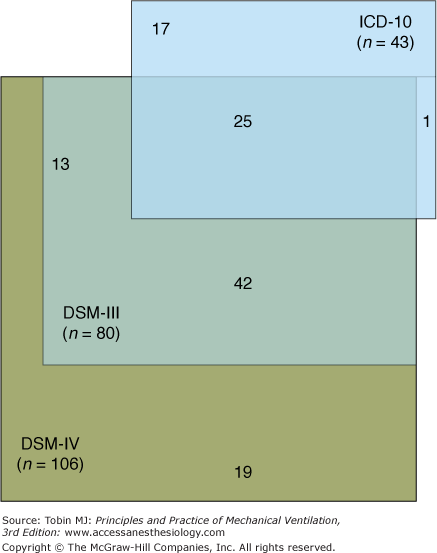
A diagnosis of delirium is based on the reference standard of symptoms described in nonventilated patients deemed clinically delirious, mostly among geriatric patients where the syndrome is prevalent. The DSM-IV criteria require a fluctuating disturbance in cognition and in consciousness in the context of an acute medical illness. Conversely the World Health Organization’s ICD-1015 includes different criteria for clinical and research use, both of which include a broad range of features that capture the phenomenologic complexity of the syndrome. Comparison of these two sets of criteria in a group of 425 nonventilated elderly medical or nursing home patients showed that applying the DSM-IV criteria identified more (n = 106) patients as having delirium than did the ICD-10 criteria, with twenty-five patients considered delirious by both sets of diagnostic criteria (Fig. 54-2).16 Surprisingly, this study reported similar outcomes, in terms of mortality or length of stay, regardless of the criteria applied to diagnose delirium (Table 54-1).
Figure 54-2
Comparison of different screening tools in the same population of 425 nonmechanically ventilated elderly medical or nursing home patients using DSM-IV criteria and earlier DSM criteria (DSM-III) as well as ICD-10 criteria. More (n = 106) patients were identified as having delirium with the DSM-IV than with any other set of diagnostic criteria. (Adapted, with permission, from Laurila JV, Pitkala KH, Strandberg TE, Tilvis RS. Impact of different diagnostic criteria on prognosis of delirium: a prospective study. Dement Geriatr Cogn Disord. 2004;18:240–244.)
| Prognostic Variable | DSM-IV (n = 106) | DSM-III (n = 80) | ICD-10 (n = 43) | p-valuea |
|---|---|---|---|---|
| Mortality/1 year, % | 34.9 | 36.3 | 41.9 | n.s. |
| Mortality/2 year, % | 58.5 | 62.5 | 65.1 | n.s. |
| Mean days in institutions/1 yearb | 220(150) | 230(148) | 211(157) | n.s. |
| New admissions to permanent institutional care/2 year, % | 55.0[33/60] | 60.0[24/40] | 64.3[9/14] | n.s. |
| In permanent institutional care or deceased/2 year, % | 90.6 | 93.8 | 97.7 | n.s. |
Thorough descriptions of the natural history of delirium in ventilated patients are lacking, as is a good understanding of its basic scientific and biologic mechanisms. In 2001, two groups reported independently validated delirium screening scales for use in ventilated critically ill patients.3,4 The first, the Intensive Care Delirium Screening Checklist (ICDSC), is an eight-point item scale, where four points or more correspond to a clinical diagnosis of delirium. The scale was validated against the clinical bedside opinion of a psychiatrist. The advantage of using this eight-item scale with a four-point cutoff is its ability to detect subsyndromal delirium in patients with scores of more than 0 but less than 4 items. Subsyndromal delirium is considered clinically significant by psychiatrists17,18 and, in ventilated and nonventilated ICU patients, predicts an intermediate risk of prolonged length of stay and mortality when compared with asymptomatic patients,19 who did better, or delirious patients, whose prognosis was the worst. The second delirium scale was originally adapted as a simplification of the DSM-IV–based Confusion Assessment Method (CAM) scale, so as to make it applicable to ventilated patients; it was validated against the clinical opinion of a geriatrician. This modified scale, the Confusion Assessment Method in Intensive Care Units (CAM-ICU),2 is binary. Other scales, such as the Delirium Detection Scale (DDS) and the Nursing Delirium Screening Scale (NuDESC), have also been assessed in critically ill patients; only the ICDSC and the CAM-ICU are presented here because of their broad application to and validation in ventilated patients, and because of their psychometric quality.
Clinicians are reported to underrecognize delirium.20,21 This has led some critical care professional societies to promote routine critical care delirium screening.22 Canadian governing bodies mandate it for hospital accreditation. Perusal of the literature on screening tools, however, shows that these validated screening tools yield a broad distribution of incidences of this condition. Studies describing the binary CAM-ICU in similar populations reveal delirium incidences that range from 10%23 to over 80%. Sedation may confound the scale measurements.24 In contrast, the range in reported delirium rates using the ICDSC is somewhat narrower: 32%25 to 45%.21 In addition to grading cognitive normalcy, subsyndromal delirium and delirium the ICDSC describes specific symptoms,26 and with them, the prognosis conferred by each one. Whether these two tools screen for the same constellation of symptoms is unclear, given the conflicting results in the publications on the subject.27,28 Because of the numerous methodological issues described above, comparisons of sensitivity and specificity of delirium screening scales to mechanically ventilated patients in and outside the ICU are difficult to address.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree