Psychiatric Complications in the Postpartum Period | 31 |
Women are most likely to develop a mood disorder during the childbearing years, and the postpartum period represents a particularly high-risk time for new onset of psychiatric illness as well as exacerbation or recurrence of preexisting psychiatric conditions (Munk-Olsen, Laursen, Pedersen, Mors, & Mortensen, 2006; Stuart-Parrigon & Stuart, 2014; Yonkers et al., 2009). Because of the frequency and regularity of obstetric visits during pregnancy, the impact of the birth experience, and the unique provider–patient relationship, most women seek consultation from obstetric providers when experiencing psychiatric symptoms throughout childbearing years as well as during pregnancy and postpartum periods. For women with no prior psychiatric history, mood disorder symptoms can be experienced as both unfamiliar and distressing. Recognition of an initial episode of depression may be challenging as women will often attribute psychiatric symptoms such as anxiety, fatigue, decreased energy, low mood, and anhedonia to the labor and birth experience, or simply new motherhood (Beck & Driscoll, 2006).
Since psychiatric symptoms can emerge with relative suddenness in the postpartum period, it is not uncommon for these women to present to obstetric triage or emergency settings. However, due to multiple societal messages that motherhood is synonymous with fulfillment and joy, many women feel a sense of shame and guilt and may be reluctant to disclose mood symptoms or negative thoughts. It is imperative that key personnel in the triage setting be familiar with psychiatric symptoms most likely to emerge during peripartum, prepared to assess the acuity of psychiatric symptoms, and able to identify the need for immediate psychiatric care versus a referral for psychiatric consultation at a subsequent appointment. When severe postpartum psychiatric symptoms go unrecognized and untreated, the consequences for both mother and infant can be dire. Obstetric providers, as primary medical caregivers for perinatal women, are uniquely positioned to intervene when psychiatric complications are detected. Like all medical conditions, early detection and intervention can greatly improve outcomes for both mothers and infants (Vesga-Lopez et al., 2008).
POSTPARTUM DEPRESSION
Postpartum depression (PPD) is the most common psychiatric complication of the prenatal and postpartum periods, affecting approximately 10% to 15% of women 366(Gavin et al., 2005; Robertson, Grace, Wallington, & Stewart, 2004; Sit & Wisner, 2009). Although this prevalence rate is similar for depression among nonpregnant women, the rates of first onset and severity of depression are increased threefold (Stewart, Robertson, Dennis, Grace, & Wallington, 2003). Major depressive disorders regardless of onset during, after, or unassociated with pregnancy have high rates of recurrence. At least 50% of individuals who recover from an initial episode of depression will have one or more additional episodes during their lifetime (5th ed.; DSM–5; American Psychiatric Association [APA], 2013), which usually occurs within 5 years of the initial episode (Burcusa & Iacono, 2007). Approximately 80% of those with a history of two episodes of depression will have another recurrence (APA, 2013) and, on average, individuals with a history of depression have five to nine depressive episodes during their lifetime (Burcusa & Iacono, 2007).
According to the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5; American Psychiatric Association, 2013), PPD is formally classified as a major depression, either recurrent or single episode, with a range from mild to severe. The specifier “peripartum onset” is now used when symptoms occur during pregnancy or in the 4 weeks following childbirth. Although the DSM-5 specifies onset of symptoms within the first 4 weeks of childbirth to be categorized as PPD, many women don’t recognize PPD symptoms until much later in the first year. The DSM-5 notes that 50% of “postpartum” major depressive episodes actually begin prior to delivery. These episodes are now collectively referred to as peripartum episodes and are often associated with severe anxiety and even panic attacks. Postpartum mood episodes with psychotic features occur in 1 in 500 to 1 in 1,000 deliveries and may be more common in primiparous women (APA, 2013). Once a woman has had a postpartum episode with psychotic features, the risk of recurrence with each subsequent delivery is between 30% and 50% (APA, 2013). When unrecognized and untreated, PPD causes profound suffering for the mother and, although rare, can result in suicide. PPD can compromise mother–infant interactions and care practices; the long-term deleterious impact of untreated maternal depression on infant/child development is well-documented (Field, 2010).
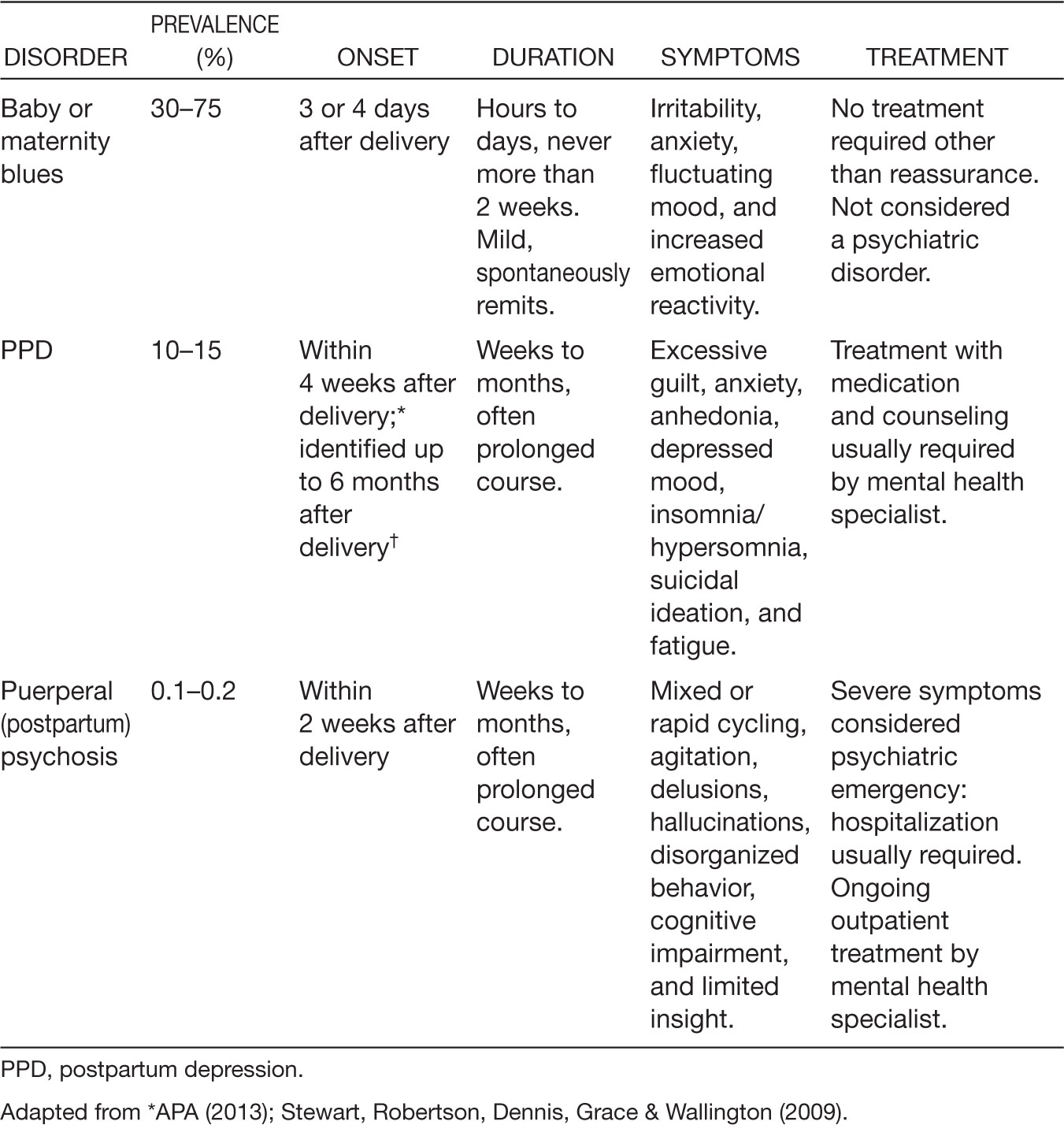
Postpartum mood disorders are typically categorized as: postpartum blues, PPD, and puerperal (postpartum) psychosis. The prevalence, onset, duration, symptom, and treatment of these three types of postpartum mood disorders are summarized in Table 31.1 (APA, 2013; Robertson et al., 2004).
RISK AND PROTECTIVE FACTORS
PPD occurs in women of all socioeconomic, cultural, ethnic, and age groups. Antenatal risk factors that render a woman more vulnerable to PPD in order of effect size include: depression during pregnancy, anxiety during pregnancy, stressful life events during pregnancy or the early puerperal period, poor social support, and previous history of depression (Robertson et al., 2004). Moderate risk factors predictive of PPD include child-care stress, low self-esteem, maternal neuroticism, negative attribution style, and difficult infant temperament (Stewart et al., 2003). Neuroticism is a lifelong tendency or personal trait characterized by anxiety, fear, moodiness, worry, envy, anger, and depressed mood. Women who identified as “being nervous,” “shy, self-conscious,” or a “worrier” through questionnaires and women who had negative cognitive attributional styles of “pessimism,” “anger,” and “ruminations” were more likely to develop PPD (Robertson et al., 2004). Single marital status, poor relationship with partner, and lower socioeconomic status, including income, were weaker predictors of PPD (Beck, 2001; Stewart et al., 2003). Pregnancy-related complications such as preeclampsia, hyperemesis, premature labor, and delivery-related complications such as premature delivery, instrumental delivery, and emergency caesarean section also have a small yet significant effect in the onset of PPD (Stewart et al., 2003; Verreault et al., 2014). No relationship has been found for ethnicity, maternal age, level of education, parity, or gender of child in Western societies in predicting PPD (Stewart et al., 2003). A more recent study identified adolescence, poverty, and recent immigrant status as additional predictors of PPD (Pearlstein, Howard, Salisbury, & Zlotnick, 2009). Far less is known about protective factors associated with PPD beyond the absence of identified risk factors (Robertson et al., 2004; Verreault et al., 2014). One recent notable study reports that women experiencing a supportive couple relationship are less likely to report PPD symptoms even when they have a history of depression or a prior PPD episode (Banker & LaCoursiere, 2014).
TABLE 31.1 Postpartum Affective Disorders: Summary of Onset, Duration, Symptoms, and Treatment
A systematic review of risk factors for depressive symptoms during pregnancy identified maternal anxiety, life stress, history of depression, lack of social support, unintended pregnancy, Medicaid insurance, domestic violence, lower income, lower education, smoking, single status, and poor relationship quality were associated with greater likelihood of antepartum depressive symptoms (Lancaster et al., 2010). These antepartum risk factors need to be considered in conjunction with prenatal depression screening recommended by the American 368College of Obstetricians and Gynecologists (ACOG) at the initial prenatal visit and at each trimester (ACOG, 2015). A similar systematic review of risk factors associated with PPD included anxiety and depression during the pregnancy, experiencing stressful life events during pregnancy or the early postpartum period, traumatic birth experience, preterm birth/infant admission to neonatal intensive care, low levels of social support, previous history of depression, and breastfeeding problems (ACOG, 2015).
PRESENTING SYMPTOMATOLOGY
The diagnosis of PPD is challenging due to inherent changes in sleep, appetite, and energy during the early postpartum weeks. Similarly, fatigue, emotionality, irritability, and worry over the infant’s well-being are common postpartum and typically referred to as the “baby” or “postpartum blues.” While not a true disorder, postpartum blues respond well to support, reassurance, and adequate sleep and resolve by week 3 postpartum.
Postpartum depression, on the other hand, is a serious disabling condition and is characterized by sad, depressed mood and loss of interest or pleasure persistent for at least 2 weeks. Additional symptoms include sleep disturbance, most typically insomnia (e.g., unable to sleep when the infant sleeps); lack of energy; feelings of worthlessness or guilt, often with the belief of being a “bad mother”; difficulty thinking, concentrating, and making decisions; and thoughts of suicide or “everyone would be better off without me.” Other hallmark symptoms of PPD include anxiety, lack of attachment to the infant, and intrusive and unwanted thoughts of harm befalling the infant. Research substantiates clinical observation that there is no correlation between the presence of intrusive harming infant thoughts and acting on them (Barr & Beck, 2008). Rather, these thoughts are experienced as highly distressing to the mother, can result in avoidance of the infant, and signal the severity of the depression.
HISTORY AND DATA COLLECTION
In the triage setting, a brief, easily administered and scored self-report screening measure is an optimal first step in detecting depression (Gjerdingen & Yawn, 2007). The most widely used and well-studied depression screening tool for perinatal women is the 10-item Edinburgh Postnatal Depression Scale (EPDS; Cox, Holden, & Sagovsky, 1987), which has demonstrated validity, sensitivity (80%–90%), and specificity (80%–90%) in screening for the presence of PPD (Agency for Healthcare Research and Quality [AHRQ], 2013). Scores 13 or greater are generally indicative of depression. The EPDS is a 10-item measure with a 0–3 Likert scale response set with a range of 0–30 points (see www.sadag.org/images/brochures/edinburghscale.pdf). A cut-point of 10 is suggestive of depression and scores of 12.5 or greater are considered indicative of depression (Cox et al., 1987).
The nine-item Patient Health Questionnaire-9 (PHQ-9; Kroenke, Spitzer, & Williams, 2001) is a general depression screen commonly used in adult primary care settings and may be more familiar to primary care providers (see Exhibit 31.1). Comparative performance of the EPDS and the PHQ-9 in pregnant and postpartum women seeking mental health services found both measures had comparable sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) for detecting depression (Flynn, Sexton, Ratliff, Porter, & Zivin, 2011). The PHQ-2 (Kroenke, Spitzer, &Williams, 2003) consists of the first two questions of the PHQ-9, has 100% sensitivity and 44.5% to 65.7% specificity in screening for depression, and may be appealing in a busy obstetric triage setting as a brief screening measure (AHRQ, 2013). If the response is “yes” to either question, consider administering the PHQ-9, the EPDS, or asking more questions about possible depression. If the response to both questions is “no,” the screen is negative.
369EXHIBIT 31.1
Patient Health Questionnaire (PHQ-9)
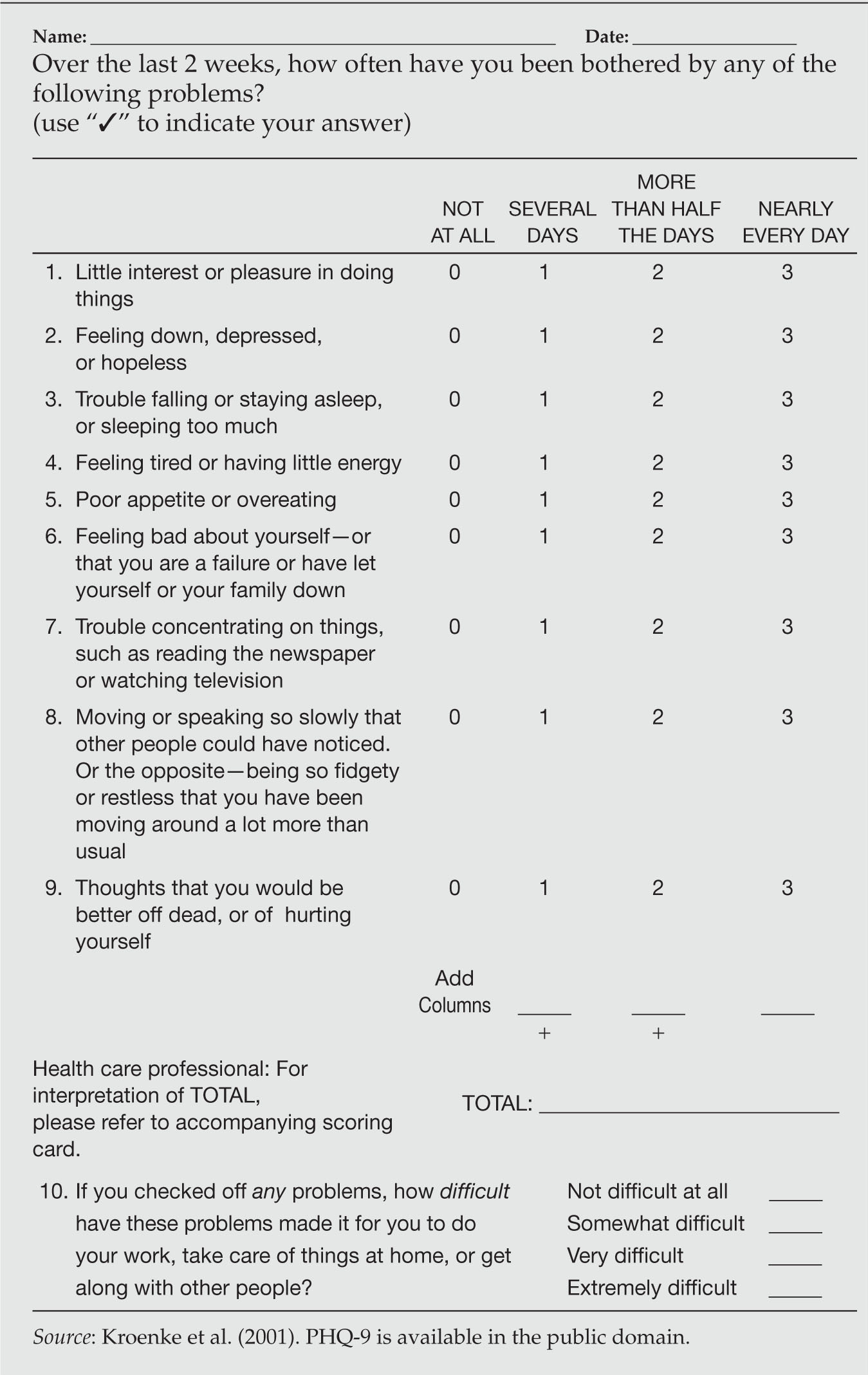
370The EPDS, PHQ-9, and PHQ-2 perform similarly in screening for depression in postpartum women (Flynn et al., 2011; Gjerdingen, Crow, McGovern, Miner, & Center, 2009). Positive screens can be followed by careful additional inquiry about mood state, sleep, appetite, concentration, anxiety, intrusive negative thoughts, hedonic capacity, degree of attachment to infant, and presence of suicidal thoughts. Symptom onset, intensity, and duration are critical as well as information regarding the woman’s degree of functional impairment and whether or not adequate social support is present. History of prior episodes of depression, anxiety or other mood disorders, substance use, and interpersonal or environmental stress must also be obtained to determine comorbidities and inform treatment planning.
A distinct advantage of the PHQ-9 is that the self-report measure includes diagnostic and symptom severity items that can be used for screening, diagnosis, and monitoring treatment response for depression over time (AHRQ, 2013). A PHQ-9 score of 10 or greater has a sensitivity of 88% and a specificity of 88% for major depression (Kroenke et al., 2001). PHQ-9 scores range from 0 to 27 with scores 0 to 4 indicating none to minimal depression, 5 to 9 indicating mild, 10 to 14 indicating moderate, 15 to 19 indicating moderately severe, and 20 to 27 indicating severe depression (Kroenke et al., 2001).
SUICIDE RISK ASSESSMENT
A positive depression screening score indicates the need for suicide risk assessment. Although suicide rates are lower during pregnancy and the postpartum period, perinatal women who complete suicide do so by more violent and lethal means than nonperinatal women (Lindahl, Pearson, & Colpe, 2005). Risk factors for suicide include comorbid psychiatric and substance abuse disorders and having a stillbirth or infant death within the first postpartum year. It is recommended that when assessing suicidality in the pregnant or postpartum woman, specific inquiry must be made about suicide risk factors such as prior suicide attempts, previous trauma, current domestic violence, substance abuse, and access to firearms. Further inquiry about current suicidal thoughts, a suicide plan, access or means to carry out the plan, and intent to act on the plan warrant timely psychiatric consultation and likely hospitalization (Johannsen et al., 2016).
OTHER POSTPARTUM PSYCHIATRIC CONDITIONS
PPD is a term that is universally recognizable among obstetric providers, yet other postpartum psychiatric conditions exist that, while not as common as depression, are equally debilitating and just as likely to be encountered in the triage setting. These include postpartum psychosis and postpartum anxiety disorders and subtypes.
371POSTPARTUM PSYCHOSIS
Postpartum psychosis, although not part of the formal psychiatric diagnostic nomenclature, is a widely used term to describe a severe and relatively uncommon psychiatric condition that occurs in one to two per 1,000 live births (Munk-Olsen et al., 2006). It requires immediate attention, likely inpatient psychiatric hospitalization, and has a rapid onset, with symptoms evident in the first 2 to 4 weeks after delivery. Women with postpartum psychosis may present to the obstetric triage unit exhibiting confusion, disordered thinking, mood lability, and delusions. Disorganized, bizarre behavior may be witnessed as well as flat or inappropriate affect.
Women with psychotic symptoms are frequently accompanied by family members who may additionally report paranoia, suspiciousness, grandiosity, and evidence of auditory or visual hallucinations. There are likely to be reports of poor judgment and impaired functioning. Sleeplessness and other hypomanic symptoms such as agitation and irritability are common prodromal states, emerging within 72 hours of childbirth. Unrecognized postpartum psychosis can have serious consequences including infanticide, suicide, and infant abuse/neglect. Women with postpartum psychosis may have command auditory hallucinations telling them to kill the infant or delusional beliefs that the infant or they are, for instance, possessed by demons and can only be saved through death. Risk factors include a previous episode of postpartum psychosis, previous hospitalization for a manic or psychotic episode, current or past bipolar disorder diagnosis, family history of bipolar disorder, primiparity, and recent discontinuation of mood stabilizers (Doucet, Jones, Letourneau, Dennis, & Blackmore, 2011).
POSTPARTUM ANXIETY DISORDERS
Worry is common in new mothers and is often regarded as an adaptive and protective response in the early postpartum period. When anxious worrying becomes excessive, occurs in multiple settings/situations, does not respond to reassurance, inhibits normal functioning, or interferes with self-care or care of the infant, it has moved along the continuum from “normal” to “disordered.” Subtypes of anxiety disorders include generalized anxiety disorder (GAD), obsessive compulsive disorder (OCD), and panic disorder and posttraumatic stress disorder (PTSD). Because anxiety disorders and major depression are highly comorbid in the postpartum period, it is essential to screen for both (Austin et al., 2010).
Panic Disorder
Panic disorder is characterized by unpredictable, discrete episodes of intense anxiety and includes symptoms of fear, heart palpitations, shortness of breath, chest pain, dizziness, numbness or tingling, nausea, sweating, choking, fear of dying, or losing control. Postpartum women who experience an episode or more of panic will frequently present to the emergency department believing they are having a heart attack or other catastrophic medical crisis. There has been some evidence that weaning may precipitate or exacerbate panic symptoms (Ross & McLean, 2006).
372Posttraumatic Stress Disorder
PTSD develops in response to a traumatic event, which is either witnessed or experienced and involves actual or threatened death, serious injury, or threat to physical integrity. The response to the traumatic event includes intense fear, helplessness, or horror. Women who have undergone traumatic deliveries and/or women with histories of prior trauma are susceptible to PTSD during the postpartum period. Symptoms include hypervigilance, fear, irritability, poor concentration, sleeplessness, heightened anxiety, intrusive recollections of the traumatic event, flashbacks or “re-living” of the experience, and psychologic and physiologic reactivity when exposed to stimuli associated with the traumatic event. Additional symptoms include emotional numbing, avoidance of stimuli reminiscent of the event or evocative of the feelings, or thoughts associated with the traumatic event. Women who have been victims of childhood or adult sexual assault may become “triggered” and experience PTSD symptoms during childbirth procedures, examinations, and delivery (APA, 2013).
BIPOLAR DISORDER
Bipolar disorders are characterized by mood swings with periods of elevated, expansive, or irritable mood and increased energy or activity with major depressive episodes characterized by depressed mood or loss of interest, significant weight loss or gain, insomnia or hypersomnia, psychomotor agitation or retardation, fatigue or loss of energy, feelings of worthlessness or excessive guilt, diminished concentration or indecisiveness, and recurrent thoughts of death or suicidal ideation with or without a specific plan (APA, 2013). Bipolar I disorder must include at least one full manic episode of abnormal and persistently elevated, expansive, or irritable mood and abnormally increased activity or energy lasting at least 1 week and present nearly every day. Symptoms include inflated self-esteem or grandiosity, decreased need for sleep (e.g., feeling rested after only 3 hours of sleep), talkative or pressured speech, distractibility, and excessive involvement in activities that have high potential for painful consequences (APA, 2013). Bipolar II disorder is characterized by hypomanic episodes, never a full manic episode, episodes of depression, and often a history of chronic irritability.
Diagnosis of bipolar disorder is often missed in women with PPD, which has significant clinical implications (Sharma, Khan, Corpse, & Sharma, 2008). Misdiagnosis of symptoms as PPD can result in pharmacologic intervention with antidepressants, typically selective serotonin reuptake inhibitors (SSRIs) or serotonin norepinephrine reuptake inhibitors (SNRIs; Connolly & Thase, 2011). Antidepressants can trigger psychotic symptoms, cause a full manic episode, contribute to rapid-cycling, and result in a more difficult course of clinical treatment (Stahl & Grady, 2011). The woman’s mental health history, family psychiatric history, careful questioning about episodes of high energy with little sleep, mood swings, risky behaviors, and using reliable and valid assessment measures are critical to make an accurate differential diagnosis. The 17-item Mood Disorder Questionnaire (MDQ; Hirschfeld et al., 2000) is a valid, psychometrically sound measure to screen for bipolar disorder (MDQ available at www.dbsalliance.org/pdfs/MDQ.pdf).
OBSESSIVE COMPULSIVE DISORDER
Intrusive, short-lived thoughts of causing accidental harm to the infant are a common and relatively normative experience among new mothers, while 50% 373of new mothers report unwanted, intrusive thoughts of intentionally harming the infant (Fairbrother & Woody, 2008). Compared with intentional harm thoughts, accidental harm thoughts are more frequent and time consuming, yet less distressing to new mothers (Fairbrother & Woody, 2008). Obsessive compulsive disorder (OCD), however, is an extreme form of recurring intrusive thoughts and interferes with a woman’s ability to care for herself and/or the infant. Obsessive compulsive disorder is characterized by intrusive, unwanted images, thoughts, or impulses either with or without accompanying compulsions. The most common obsessions experienced by postpartum women include contamination, intentionally or accidentally harming the infant, need for order/symmetry, and catastrophic images. Compulsions are goal-directed, driven, and repetitive or ritualized behaviors; engagement in them results in temporary reduction of anxiety associated with the obsessive thoughts or beliefs. Compulsions include cleaning, checking (often resulting in sleep deprivation due to incessant checking on infant), washing, praying, counting, repeating certain phrases, or other ritualized behaviors. The postpartum period represents a time of increased vulnerability to the onset of OCD and a time of symptom exacerbation in women with preexisting OCD (Zambaldi et al., 2009).
ASSESSMENT AND MANAGEMENT OF POSTPARTUM MENTAL HEALTH DISORDERS
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








