Chapter 21 Principles of Invasive Monitoring
Role of Invasive Hemodynamic Monitoring
In his 1733 report “Statical essays: containing haemastaticks; or, an account of some hydraulick and hydrostatical experiments made on the blood and blood-vessels of animals,” Hales1 described early experiments in horses in which he was the first to measure central venous pressure (CVP). Figure 21-1 depicts Hales and an assistant in the process of these early experiments.

Figure 21–1 Clinician and an assistant measuring the blood pressure of a horse.
(From Pickering G: Systemic arterial hypertension. In Fishman AP, Dickinson WR, editors: Circulation of the blood: men and ideas, New York, 1964, Oxford University Press.)
This chapter aims to be a practical guide to the use of hemodynamic monitoring in the pediatric ICU. The chapter reviews general principles of measurement and then discusses the three main types of invasive hemodynamic monitoring: central venous catheter, arterial catheter, and pulmonary artery catheter. It addresses the indications and controversies, sites of insertion, interpretation of waveforms, and potential complications. It also reviews CO monitoring and calculation of oxygen consumption and delivery. Chapter 15 discusses the specific techniques for gaining access in order to make these measurements.
Indications for Invasive Hemodynamic Measurements
The three main indications for invasive hemodynamic monitoring are diagnosis, surveillance, and titration of therapy. Diagnosis may include the differentiation of septic shock (through assessment of factors such as diminished right heart filling pressures or preload and decreased systemic vascular resistance) from cardiogenic shock (which is characterized by elevated left heart pressures and afterload). Surveillance implies observation over time. The purpose of surveillance may be to assess the stability of a patient at risk for adverse changes or to determine the response to therapy. Invasive measurements performed for diagnostic purposes often are continued for surveillance purposes. Titration of therapy often is based on information gleaned from invasive measurements.
Principles of Measurement
Intensive care clinicians rely on a wide variety of measurement systems to assess patient clinical status and response to therapy. However, not all clinicians have a good understanding of how physiologic variables are measured, and some may not be able to troubleshoot monitoring systems or recognize when information obtained is inaccurate. A detailed discussion of monitoring is beyond the scope of this chapter, but a basic understanding of the principles of measurement is helpful in deciding which measurements to trust and how to assess a monitoring system for accuracy. Detailed descriptions of monitoring systems are provided elsewhere.2–4
Signal Analysis
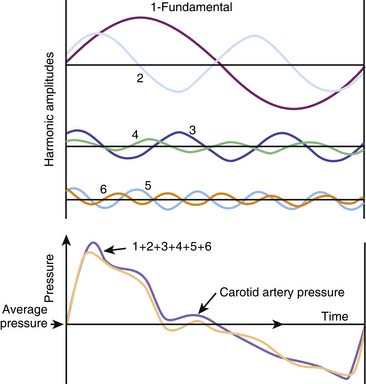
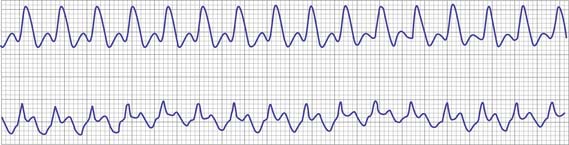
Complex periodic signals, such as an arterial pressure waveform, can be described mathematically as the sum of a series of simpler waveforms called a Fourier series. Alternatively, the arterial tracing can be thought of as a sum of simpler waveforms, sine waves, and cosine waves. Figure 21-2 depicts an arterial pressure waveform as the sum of the first six terms in the Fourier series. The sum of the first six terms in the series forms a waveform similar to the original tracing. Adding additional terms from the Fourier series, or higher harmonics, results in an increasingly better representation of the actual waveform. In general, to reproduce a pressure tracing without loss of significant characteristics for clinical use, the measurement system must have an accurate frequency response to approximately 10 times the fundamental frequency (first 10 harmonics).
The sampling rate of a measurement system determines how often a physiologic value is measured. For body temperature, sampling every few minutes might be sufficient, but for arterial pressure measurement, a higher rate is needed. This principle may seem obvious, but as an example of the importance of sampling rate, consider the number of points needed to define a circle. If we place three equidistant points on a circle, we describe a triangle, not a circle. Similarly, four points describe a square. If we increase the number of points (sampling rate), we can describe the circle more completely. For a sine wave, the minimum frequency of sampling needed to preserve the waveform is twice the frequency. This mathematical minimum is known as the Nyquist frequency.2 For complex waveforms such as arterial pressure tracings, the sampling rate must be at least twice the highest frequency component in the waveform.
Frequency Response
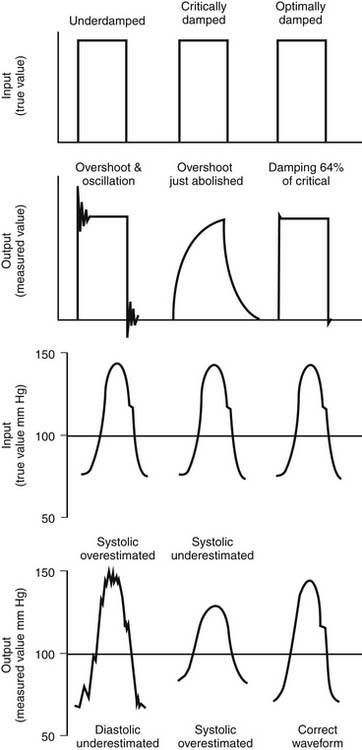
The ability of a measurement system to accurately measure an oscillating signal, such as arterial blood pressure, is dependent upon the system’s frequency response. The system can either overestimate or underestimate the true amplitude of a signal. If the system is overdamped, the value reported underestimates the amplitude, and waveform characteristics may be lost. Resonance in the system may result in overestimation of the amplitude. Measurement of arterial systolic pressure—the amplitude of the arterial waveform—may be inaccurate because of overdamping, and important waveform characteristics may be lost if the frequency response of the measurement system is poor. Figure 21-3 illustrates the effects of dampening on measurement of blood pressure.
Impedance
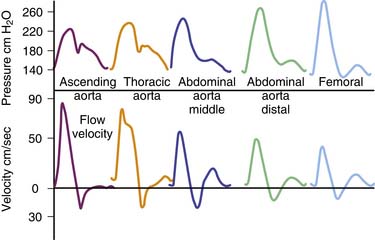
When blood is propelled through a vessel at a branch point, a reflected pressure wave back toward the heart increases the impedance of the system. The major sites of wave reflection from vessel branching are from vessels approximately 1 mm in diameter.3 Thus these small vessels contribute significantly to overall impedance. Figure 21-4 shows the relationships between pressure and flow velocity with distance along the length of the aorta. Because blood pressure increases with distance from the heart and flow velocity decreases with distance, the impedance increases toward the peripheral vasculature. Hemodynamic measuring systems are essentially physical extensions of the vascular system; thus the configuration and characteristics of the tubing and transducer system can alter the overall effect of impedance.
Invasive Techniques
Central Venous Pressure Catheters
Indications
Indications for CVP catheter placement in pediatric patients include assessment of right heart filling pressure (CVP), monitoring of large fluid shifts between the intravascular and the extravascular space, infusion of vasoactive substances, monitoring mixed venous oxygen saturation for goal directed therapy of sepsis, and infusion of hyperosmolar fluids and/or irritants.5–7
Interpretation of Waveforms
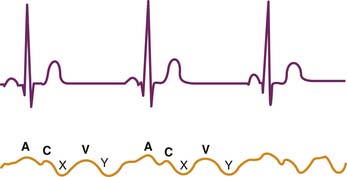
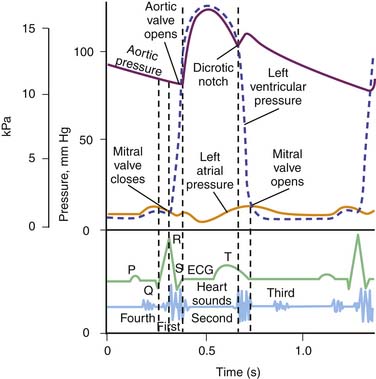
The CVP waveform is divided into three components: a, c, and v waves (Figure 21-5). Each component can be correlated with a specific portion of the electrocardiogram (ECG) tracing. The a wave occurs with atrial contraction and is seen after the P wave of the electrocardiogram during the PR interval. Thus the mean value of the a wave approximates right ventricular end-diastolic pressure. Canon a waves (Figure 21-6), which are enlarged a waves seen when the right atrium is ejecting against a closed tricuspid valve, may be seen when atrioventricular discordance occurs (i.e., during junctional ectopic tachycardia, ventricular tachycardia, or heart block). The c wave occurs in early systole with closure of the tricuspid valve and is seen at the end of the QRS complex in the RST junction. The v wave occurs during filling of the right atrium in late systole prior to opening of the tricuspid valve and is seen between the T and P waves of the ECG. The v wave is increased in the setting of tricuspid regurgitation. The x descent is the decrease in pressure after the a wave, reflecting atrial relaxation. The y descent is the decrease in pressure that occurs after the v wave as the tricuspid valve opens and passive filling of the right ventricle occurs.
Continuous Mixed Venous Oxygen Saturation
Mixed venous oxygen saturation (SvO2) can be measured continuously by using a specially designed central venous catheter. These catheters have two to three lumens and have the same capabilities of the catheters previously described. The SvO2 catheters use reflection spectrophotometry and are able to read hemoglobin oxygen saturation continuously. The reflected light is dependent on the oxygenated and deoxygenated hemoglobin concentration in the circulating blood.8
SvO2 is another parameter used to monitor the relationship between oxygen delivery and demand and is often used as a surrogate for cardiac index. Rivers et al.9 showed that when continuous SvO2 monitoring was used to guide resuscitation and hemodynamic support in patients with severe sepsis and septic shock, survival rates improved. Recent guidelines set forth by the American College of Critical Care Medicine/Pediatric Advanced Life Support have recommended goal-directed therapy with a target SvO2 of ≥70% in children and adolescents who are in septic shock.7 A randomized controlled trial conducted by Oliveira and colleagues10 supported the use of these guidelines in children and adolescents with severe sepsis or fluid-refractory septic shock.
Ideally, the catheter should be placed in the right internal jugular, with the tip taking measurements in the SVC. SvO2 measurements obtained from the inferior vena cava exhibit greater variability because of fluctuations in splanchnic oxygen utilization and thus are less reliable. SvO2 measurements from the right atrium contain coronary sinus blood and are more desaturated because of the high oxygen extraction rate of the myocardium. Studies in critically ill children have evaluated SvO2 measurements obtained in the pulmonary artery and the SVC. Concordance analysis showed appropriate agreement in the measurements between these two sampling sites.11 This finding has clinical importance because the use of pulmonary artery catheters (PACs) has declined, while central venous line use has increased.12 Continuous SvO2 monitoring can alert the intensivist to early changes in hemodynamic status and allows for less frequent opening of the central line for blood sampling and thus less risk of infection. Percutaneously placed SvO2 central lines have even been used to monitor patients undergoing complex cardiac surgery, thus avoiding the risks associated with transthoracic lines following surgery.13
Arterial Pressure Catheters
Indications
The transition to direct monitoring of arterial blood pressure dates back to the mid 1950s when two separate studies compared invasive arterial measurements and noninvasive or cuff measurements in healthy adults.14,15 Van Bergen and colleagues15 noted a frequent difference between direct and indirect measurements, with indirect measurements increasingly lower than direct measurements as the systemic blood pressure increased. The greatest disparity was found in young hypertensive patients. Similarly, Cohn and Luria16 observed that invasive arterial pressures were significantly greater than cuff pressures and emphasized the importance of direct measurements of systemic arterial pressure when caring for patients with hypotension and shock. Continuous direct monitoring of arterial blood pressure should be considered when treating patients who require more than minimal vasopressor therapy.
Indications for arterial catheterization include continuous monitoring of systemic arterial blood pressure, frequent blood sampling, and withdrawal of blood during exchange transfusions.17 In addition to the value of the measurements themselves, these measurements provide components of derived measures of CO and oxygen delivery.
Interpretation of Waveforms
Systolic blood pressure (SBP) in children varies greatly with age and gender. As with the CVP waveform, the arterial waveform can be correlated with specific parts of the cardiac cycle. The arterial waveform has three main components (Figure 21-7): (1) a rapid upstroke and downslope that correlates with systolic ejection, (2) a dicrotic notch that correlates with closure of the aortic valve, and (3) a smooth runoff that correlates with diastole. The dicrotic notch or incisura is decreased in situations of hyperdynamic CO in which left ventricular output and stroke volume (SV) are increased, pulse pressure is widened, and diastolic blood pressure (DBP) is increased (e.g., surgical systemic-to-pulmonary shunts, patent ductus arteriosus, aortic regurgitation, anemia, fever, sepsis, hypovolemia, and exercise).18 Conversely, cardiac tamponade and severe aortic stenosis can narrow the pulse pressure and are associated with a deflection (anacrotic notch) on the ascending limb of the waveform.18
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree