Chapter 9 Preoperative assessment and management of neurological disease
John Andrzejowski
Stefan Jankowski
SUMMARY
This chapter will describe:
• basic anatomy and physiology of the neurological systems
• the role of testing in the preoperative phase
• clinical approach to preoperative optimisation of neurological conditions
• therapeutic treatment of neurological conditions and implications for perioperative care.
INTRODUCTION
This chapter will address the essential background physiology and pathology that will help you undertake an evaluation of a patient presenting for neurosurgery. It will also detail how to assess patients with pre-existing neurological conditions who are due to undergo other types of surgery.
Basic science: anatomy and physiology
The brain can be considered as freely communicating fluid volumes within a fixed box (the bony skull). Intracranial pressure results from the contributions of three intracranial fluid compartments: brain tissue (parenchyma), cerebral blood vessels and cerebrospinous fluid (CSF). An increase in one of these volumes (e.g. brain tumour with surrounding oedema) increases intracranial pressure unless there is a compensatory decrease in one of the others (e.g. ventricles compress or CSF moves out).
The brain is a very greedy organ. Despite only making up 2–3% of the body’s weight, (average 1.4kg), it receives 15% of the cardiac output and uses 20% of the body’s resting oxygen consumption. Needless to say it needs careful looking after, so let us start by considering the five things a brain needs to keep it ‘happy’ (see Figure 9.1).

Fig 9.1 The brain’s requirements
Maintain blood pressure and minimise ICP
The brain keeps its blood flow steady at 50mls/100gm by a process known as autoregulation. This is what stops you fainting every time you stand up. It involves the cerebral blood vessels dilating if blood pressure (BP) is low or constricting if BP is too high. However, changes in blood vessel diameter can lead to large changes in intracranial pressure (ICP). In an at-risk brain, it is therefore a good idea to maintain a decent cerebral perfusion pressure (CPP) by keeping the mean blood pressure (MAP) about 60mmHg above intracranial pressure. Normal ICP is around 10–15mmHg, so try to keep the patient’s MAP about 80mmHg. This is essentially a normal BP. It may involve giving IV fluids, or raising the foot of the bed.
In certain conditions, a high BP can put the patient at risk of intracranial haemorrhage so it may need treating. Raising the head of the bed will help in such circumstances.
If raised ICP is the biggest risk, it can be minimised by raising the head of the bed, avoiding tight clothing or ties around the neck. Osmotic diuretics (mannitol) can be given if the patient is deteriorating rapidly due to raised ICP.
Oxygen
Administer oxygen to any patient suspected of having raised ICP or depressed neurological status. All cells need oxygen to survive. Oxygen saturation can be measured and should be kept >96% if possible.
Control CO2
Figure 9.2 illustrates what can happen to cerebral blood flow with changes in carbon dioxide. A small 1kPa rise in CO2 results in a 20% increase in blood flow to the brain due to cerebral vasodilatation. The dilated blood vessels in the brain may supply the brain with more blood, but this is at the expense of increasing ICP.
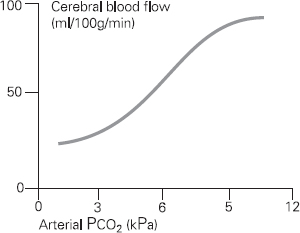
Figure 9.2 Effect of arterial carbon dioxide on cerebral blood flow
Avoid any drugs that may cause sedation or suppress respiration, since they are likely to increase CO2 levels and/or cause oxygen desaturation. Opiates are particularly hazardous in neurology patients who have raised ICP.
Control temperature
A hot brain uses more energy and consumes more oxygen; it tolerates insults badly. Try to prevent fever in neurology patients. There is evidence that patients who are hot when they have a stroke have a worse outcome. Many hospitals now cool patients following cardiac arrest to try to prevent secondary brain damage. Use paracetamol, wet towels and ice packs. Intravenous fluids can be cooled.
Provide nutrients
Patients need to have good nutrition prior to undergoing surgery. Try to maintain oral intake. Consider nasogastric feeding particularly in patients with no gag reflex who may be at risk of aspiration. TPN may be required in certain cases. The advice of a dietician may be useful at preassessment clinic in order to optimise nutrition.
The choice of intravenous fluids in neurology patients is of paramount importance. Avoid fluids that may result in hyponatraemia, since it causes cerebral oedema. Too much normal saline however can result in a hyperchloraemic acidosis due to the high chloride content. A suitable alternative is Hartmann’s (lactated Ringer’s) solution. Dextrose solutions have traditionally been avoided in neurology patients since they amount to giving free water that is rapidly redistributed throughout the body potentially exacerbating cerebral oedema. In addition, neurological damage in the presence of hyperglycaemia has a worse outcome. You should start a sliding scale insulin regime early if there is concern about blood sugar levels.
Certain neurological conditions (e.g. subarachnoid haemorrhage) may result in heavy electrolyte losses, so careful management of sodium, potassium, magnesium and phosphate levels is required.
History taking in patients presenting for neurosurgery
In addition to the usual thorough preoperative assessment, you might consider the following aims:
1. Identify significant co-morbidity that may impact upon the balance of the ‘happy brain’ discussed above.
2. Focus on the presenting condition, consider how this might complicate the perioperative course, and predict what changes might follow surgery.
Co-morbidity may include the following aspects:
Airway
Cervical spine pathology includes rheumatoid arthritis, degenerative spondylosis, intervertebral disc prolapse or tumour. Neck movements can be limited and there may be instability of the spinal column. Severe disease may affect the function of the spinal cord (myelopathy). Anticipate airway difficulty in acromegalic patients presenting for pituitary surgery. Investigations might include lateral C/Spine X-ray in flexion and extension. The patient may require neck immobilisation, and consent for awake fibreoptic intubation by the anaesthetist. Consider an antisialagogue in these cases.
Respiratory
Chronic obstructive pulmonary disease (COPD), asthma and chest infections are common in the elderly. Patients presenting with intracranial tumours may have a primary in the lungs. Recurrent aspiration (often silent) may complicate neuro-muscular disorders, as swallowing and the cough reflex may be impaired. These conditions can cause problems with oxygenation and ventilation (removal of carbon dioxide), so consider whether optimisation is possible. Investigations might include pulmonary function tests (PFTs), chest X-ray, arterial blood gases (ABGs). Preoperative optimisation includes the use of bronchodilators, antibiotics, and physiotherapy. Surgery may need to be postponed.
Cardiovascular
Hypertension should be controlled to prevent falls in cerebral blood flow (CBF). Autoregulation maintains CBF between 60 and 100mmHg in most people. These limits may be somewhat higher, however, in chronically hypertensive patients, with the result that an intraoperative fall in blood pressure (which is not uncommon) may detrimentally decrease CBF. Resetting of these limits occurs only after hypertension has been treated for some time. Untreated hypertensives may need surgery postponing for six weeks whilst their blood pressure is controlled. Ischaemic heart disease is common in the elderly, and ideally should be stable with no evidence of heart failure. Subarachnoid haemorrhage may be complicated by ECG changes and neurogenic pulmonary oedema.
Endocrine
It is thought that hyperglycaemia may aggravate ischaemic brain injury by increasing cerebral lactic acidosis (possibly by the supply of a substrate for metabolism, glucose, when no oxygen is being delivered to the cell). Diabetes should therefore be well controlled. Steroids, used acutely for cerebral oedema, and the stress response to acute illness, may cause hyperglycaemia. Inpatients may be managed with sliding scale insulin. Blood sugars of 6–9 are acceptable.
Patients with pituitary disease may have complex endocrine disorders with excess or depletion of hormones. A specialist endocrine opinion should be sought.
Disorders of sodium balance are common in neurological patients and necessitate the checking of urine and plasma osmolalities. Diabetes insipidus manifests with a high urine output and results in hypernatraemia. Treatment often involves the administration of desmopressin. The syndrome of inappropriate antidiuretic hormone secretion (SIADH) is more common and results in hyponatraemia. It may require fluid restriction.
Examination of neurological status
It is important to be able to assess a patient’s neurological condition (level of consciousness) rapidly and reproducibly. Changes in a patient’s condition have to be communicated to other members of the team and to this end there are two scoring systems that are commonly used.
The Glasgow Coma Scale (GCS)
Assessment should be carried out above the level of any suspected spinal cord damage. Response to pain should be by a central stimulus. Sternal rub, nailbed pressure and trapezius pinch are all often employed, but are not central stimuli. Firm pressure on the supraorbital ridge (supraorbital nerve) is used on neurosurgical units (see Table 9.1).
Table 9.1 Glasgow Coma Scale
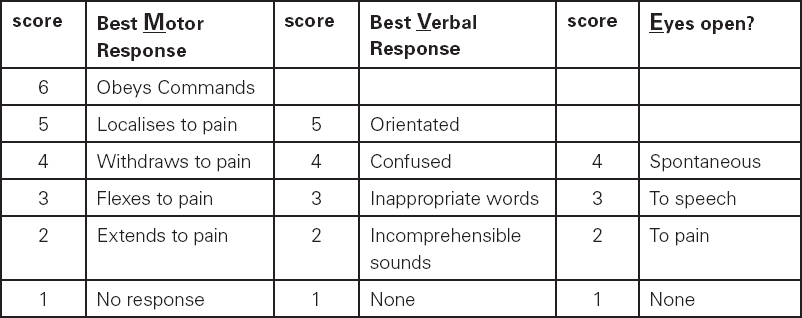
An alert patient has a score of 15 (M6, V5, E4). Patients with a GCS of less than 9 are rarely able to protect their airway (absent gag/cough) and so are at risk of hypoxia, raised CO2 and further deterioration by aspiration of gastric contents. A drop of two or more points on this scale, or an absolute score of less than 9, should prompt immediate medical review. The minimum score is 3 (M1, V1, E1) for a patient who has no response at all.
AVPU score
This is an easier scale that is often used for rapid assessment (see Table 9.2).
Table 9.2 AVPU score
| AVPU score | Assessment | Corresponding GCS |
| A | Alert | 14–15 |
| V | Responds to Voice | 11–14 |
| P | Responds to Pain | 7–11 |
| U | Unconscious | 3–7 |
The approximate GCS scores are given for comparison; it is evident that a ‘P’ (responds to pain) may give cause for immediate concern, since the GCS could be less than 9 as discussed above.
In addition to assessment of the level of consciousness it is important to document:
1. Pupillary size and response to light, as part of ongoing neurological observations.
2. Motor function of upper and lower limbs bilaterally, where GCS allows.
3. Findings of a full neurological examination. This is normally performed by the admitting clinician and is an important baseline.
Investigations
NICE guidelines for routine preoperative investigation are available, and are intended to avoid over-investigation of healthy patients. Neurosurgical units have their own protocols, but investigations should be prompted by findings in the history and examination.
Full blood count (FBC). Intercurrent infection associated with a raised white cell count or inflammatory markers (e.g. CRP/ESR) may delay surgery where implants are planned (metalwork, shunts).
Group and save (Screen)/Cross match (G&S/X-match). Craniotomy and major spinal surgery requires blood cross matching, although blood transfusion is rarely required. An agreed ‘tariff’ is usually available.
Urea and electrolytes (U&Es). Intravenous contrast agents are avoided in patients with renal impairment. Disorders of salt balance are common in sick and elderly patients, and those with endocrine disorders. The serum sodium may be high or low; a cause should be sought and treated.
Random blood glucose. Poor glycaemic control may worsen outcome in the brain injured; perioperative steroids may cause hyperglycaemia. Consideration should be given to the avoidance of dextrose-containing solutions in the management of diabetic patients. (Intravenous dextrose infusion is included in most intravenous insulin protocols, to protect from inadvertent hypoglycaemia. The free water given in such protocols may, however, worsen cerebral oedema.)
Coagulation screen. Intraoperative bleeding would make most neurosurgical procedures difficult, and be catastrophic in some. Coagulopathy should be investigated and corrected. Patients on long-term anticoagulants (e.g. warfarin), including anti-platelet agents (e.g. aspirin, clopidogrel) need careful management to minimise the risks of discontinuing treatment. Specialist haematology advice should be sought and local guidelines should be agreed.
Pulmonary function tests (PFTs). Problems with oxygenation and carbon dioxide retention may compromise the needs of the injured brain, or cause intraoperative brain swelling. Results of PFTs help guide preoptimisation where a reversible element is present (e.g. asthmatic component of COPD). A record of peak expiratory flow rate, where kept, should be examined to confirm stability in asthmatics.
Chest X-ray (CXR). Baseline in severe disease, exclusion of lung primary in patients with cerebral metastasis.
Arterial blood gases (ABGs). Rarely indicated as most neurosurgical interventions do not compromise lung function; history (exercise tolerance) and examination (respiratory rate, lung fields, pulse oximetry in air) are usually sufficient. Patients with severe respiratory or neuromuscular disease or those with bulbar palsies should have a baseline check.
Electrocardiogram (ECG). Neurosurgery is usually only considered in fit patients, but many are elderly, or have an exercise tolerance masked by the pain or weakness of their presenting condition. An ECG is mandatory following subarachnoid haemorrhage (SAH), since some myocardial damage can occur.
Pregnancy test. Intraoperative X-ray screening, particularly for lumbar surgery, presents some risk in pregnancy, and a pregnancy test should be performed on admission for surgery. Radiology departments may have local policies in this respect.
Premedication/Usual medication
Anxiolytics can be used where anxiety may, understandably, be a problem. Marked anxiety can contribute to hypertension and benzodiazepine premedication can be useful, but must not be administered until informed consent has been obtained.
Antisialagogue (drying) agents may be useful if an awake fibreoptic intubation is planned.
Anti-emetics should be prescribed with reference to local policy. Neurosurgery is usually considered medium risk for postoperative nausea, but the consequences of vomiting in those with swollen brains/obtunded airway reflexes would be significant.
Analgesia to treat ongoing pain must continue up to surgery. Simple analgesics, non-steroidals and opioid-based drugs may all be used. Consideration should be given to postoperative analgesia.
Patients on chronic opioids, and opioid abusers, need careful management; protocols exist and liaison with the acute pain team is vital.
Timely discontinuation of warfarin, anti-platelet agents (aspirin, clopidogrel), antihypertensive agents and oral hypoglycaemics, will prevent unnecessary cancellation of surgery. Discontinuing drugs is done on a balance of risks only after careful consideration.
Patients taking anti-epileptics (e.g. phenytoin) may need levels checking.
Steroid medication may need to be converted to intravenous dosing and should be continued perioperatively. Dexamethasone is often given during craniotomy.
Neurosurgical conditions
Intracranial
In general, mass lesions in the brain present with focal (localising) neurology, symptoms and signs of raised intracranial pressure (headache, vomiting, papilloedema, drowsiness), seizures, or occasionally are found incidentally during imaging for other reasons.
Scheduling of surgery tends to be more urgent than other surgical specialties; fewer elective cases mean the planning of preoperative assessment needs to be flexible. Patients admitted on-call may require surgery in a planned manner before discharge, but importantly there are some patients who require surgery as true emergencies, often admitted directly to theatre.
Examples of emergency intracranial surgery
• Intracranial haemorrhage. Bleeding can occur into different compartments in the brain, e.g. epidural/subdural/subarachnoid (see Figure 9.3).
• Cerebral abscess.
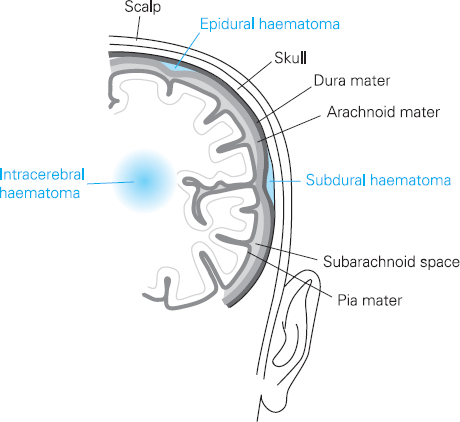
Figure 9.3
Location of epidural, subdural and intracerebral haematomas
Such neurosurgical emergencies leave little time for preoperative optimisation. If possible, a general history should be taken, with focus on neurological status and commencement of neurological observations, allowing a rapid response to any change in the patient’s condition. The need for urgent surgery should not compromise acute trauma care, with attention to ABC, spinal immobilisation, secondary survey and ongoing resuscitation.
We now consider other intracranial pathologies, by specialisation.
Oncology (tumour surgery)
Supratentorial and posterior fossa mass lesions. The intracranial content is divided into compartments by dural folds. In practice two compartments are considered:
1. That above the tentorium cerebelli (supratentorial) containing the cerebral hemispheres. This compartment contains lateral and third ventricles, which contain cerebrospinous fluid (CSF) that can move from the compartment (either by circulation or absorption) and consequently compensate for expanding mass lesions.
2. That below (termed the posterior fossa) housing the cerebellum, brainstem and fourth ventricle. This is a small compartment, bound by bony structures with little room for expansion. Brainstem function can be rapidly effected by expanding lesions. Lesions here are also more likely to compress and obstruct the ventricular drainage system, causing hydrocephalus.
The most common tumours are:
• Meningiomas (benign, arising from the dura and as such often vascular with risk of intraoperative bleeding). Surgery is usually intended to remove the entire tumour.
• Gliomas (malignant, arising from the cellular components of the brain, following a variable and unpredictable course).
• Metastasis. Often associated with oedema that responds to treatment with steroids. Surgery is usually intended to debulk tumour to alleviate symptoms/prolong life.
An oncology multi-disciplinary team usually plans the management of these cases. If surgery is planned, preoperative management should include continuation of steroids and anticonvulsants, and avoidance of neurological or respiratory depressants.
Stereotactic biopsy
Some intracranial lesions may require biopsy to establish/confirm a diagnosis. This is sometimes achieved by stereotactic biopsy. A frame is applied (usually under local anaesthetic) to the patient’s head; the brain is imaged (e.g. CT scan) with the frame in place; the patient is transferred to theatre, where the lesion can be biopsied using co-ordinates generated by the scan, and using the frame as a fixed point of reference. Patients are understandably often very anxious.
Aneurysmal disease
Blood is supplied to the brain by the internal carotid and vertebral arteries, which join together around the base of the brain as the Circle of Willis. This arrangement is intended to protect the brain should a single vessel become blocked, as flow can be recruited from other vessels in the ‘Circle’. An aneurysm occurs when there is ‘outpouching’ of the vessel wall. These can be associated with smoking, hypertension and a family history. The aneurysm is at increasing risk of rupture as it increases in size.
Some patients present post rupture, an emergency called subarachnoid haemorrhage (SAH). Life-threatening complications of this dangerous condition include re-bleeding, cardiovascular and respiratory problems and spasm of the intracranial blood vessels (vasospasm). Patients considered at risk need their aneurysm securing, either surgically, by placing a clip across the neck of the aneurysm, or radiologically, by packing the aneurysm sac with detachable titanium coils (coiling).
Patients will need careful preoperative assessment to exclude neurological, cardiac and respiratory complications. Nimodipine (a calcium antagonist shown to decrease severity of vasospasm post subarachnoid haemorrhage) should be continued up to surgery/coiling. An ECG is essential, chest X-ray (CXR) is useful; results and scans, including cranial CTs and angiograms, should be made available.
Arterio-venous malformations (AVMs)
Vascular malformations, which include AVMs, are a cause of intracranial bleed, or may present with seizures or neurological deficit. Preoperative management is as for aneurysmal disease, but a third option for treatment in some cases includes stereotactic gamma irradiation – see stereotactic radiosurgery below.
Endocrine
Tumours of the pituitary gland are quite common (8–15% of all symptomatic intracranial tumours); its complex endocrine function, and positioning within the cranial cavity, can lead to a number of different presentations. Preoperative investigation should be in conjunction with an endocrinologist. The usual surgical approach is transnasal transphenoidal resection.
Pituitary adenomas secreting growth hormone may cause acromegaly, which can make the airway difficult intraoperatively (macroglossia, malocclusion and upper airway lymphoid tissue excess). Diabetes is common, as are hypertension and cardiomegaly. Postoperatively the difficult airway can contribute to airway obstruction if the nose has been packed. Hormone replacement may be required.
Shunt
The ventricular drainage systems are subject to obstruction by tumours, trauma and intracerebral/SAH. Obstruction causes hydrocephalus (other causes include congenital abnormality) and the increase in intracranial pressure may require treatment. This can be done in a number of ways, but shunting CSF from the ventricle to the peritoneal cavity is often employed (a V-P Shunt).
Patients are often children, or have had numerous previous shunts in childhood. Signs and symptoms of raised ICP may be present.
Functional
These are highly specialised procedures for patients with movement disorders such as Parkinsonism, dystonia and tremor. One example is deep brain stimulators. Electrodes are placed, guided by neuroimaging, within the brain. The patient may be awake during the procedure (to optimise electrode placement) and intraoperative transfers for neuroimaging may be required. The electrodes are stimulated, and where benefit is seen, connected to an implanted stimulator, usually at a second operation. The surgeon might request that medical treatment is omitted preoperatively to exacerbate dystonia. However for some patients dystonia is so severe that a general anaesthetic is required for surgery.
Epilepsy
Patients with medically resistant epilepsy may be considered for neurosurgery. Operations include craniotomy to excise/disconnect the focus of seizures such as amygdalohippocampectomy and corpus callosotomy. These are complex patients, often with other neurological problems; communication can often be difficult. A carer who knows the patient well can be very helpful.
An alternative procedure to craniotomy that is helpful for some patients is implantation of a vagal nerve stimulator. During general anaesthesia an electrode is wound around the left vagus nerve (through a small incision in the neck), and connected to a stimulator, which is implanted.
Preoperative assessment should focus on epilepsy history and medication, which should be continued, and consideration given to the social needs of these patients.
Extracranial
Vascular
Carotid endarterectomy is a surgical technique to widen the carotid artery at the neck. Patients usually present with recurrent ‘mini-strokes’ (TIAs) due to a stenosis (stricture) of these vessels. The procedure may be performed under local or general anaesthesia. These patients often have cardiovascular co-morbidity, and a careful cardiovascular history and examination are important.
Spinal decompression
Conditions affecting the spinal cord may present:
1. electively; e.g. unremitting sciatica
2. urgently; e.g. cervical myelopathy
3. emergently; e.g. epidural abscess, cauda equina syndrome.
Surgery, which usually entails some form of decompression, may be required at one or more levels:
• craniocervical (usually a posterior approach)
• cervical spine (usually an anterior approach)
• thoraco-lumbar spine (usually a posterior approach).
Where the spine is unstable, fixation is required with grafts or metalwork.
Patients usually have restricted mobility secondary to pain or weakness, and the cardiorespiratory system may be difficult to assess. Degenerative disease is more common in the elderly and co-morbidity should be sought. Remember that rheumatoid arthritis is a multisystem disease. Chronic pain is common, and analgesia can be a challenge.
Complex spinal surgery
More complex surgery may be required for spinal tumours or instability. As with other major surgery perioperative problems are more likely and a high dependency bed should be available.
Chronic pain/palliative
Procedures such as spinal cord stimulators and intrathecal pumps are sometimes used in the chronic pain or palliative setting. These patients may have a number of co-morbidities and a complicated drug history.
Stereotactic radiosurgery
Gamma irradiation can be focused on some intracranial pathologies using a specialised radiotherapy machine – the gamma knife. Slow-growing tumours which cannot be accessed surgically because of their proximity to vital brain structures, and vascular malformations are two examples.
The patient has a frame fixed to their head (which can be done under local anaesthetic). They are imaged with the frame in situ, and co-ordinates (fiducials) are calculated for the gamma knife to target the lesion. If a general anaesthetic is required (patients are often paediatric, or may be claustrophobic or unable to lie still/flat), the procedure may involve a number of transfers from one location to another, under prolonged anaesthesia.
Diagnostic and interventional radiology
Although minimally invasive, patients having investigations or procedures in the radiology suite are still at some risk and require the same preoperative assessment as those undergoing surgery in theatres. In particular, any allergy to radiocontrast media, evidence of renal impairment, and a negative pregnancy test (where appropriate) should be documented. Patients may require anaesthetising if procedures are very prolonged, or they are required to keep very still.
Neuromedical conditions
Concurrent disease may affect all systems of the body. Remember to fully assess the cardiovascular and respiratory systems in all patients and take a good medication history.
Autonomic dysfunction
The autonomic nervous system regulates key functions of the body including the activity of the heart muscle, the smooth muscles (e.g., the muscles of the intestinal tract), and the glands. Possible causes of a disruption in this regulation include: diabetes mellitus, Guillain Barré syndrome, Parkinson’s disease and Shy-Drager syndrome.
Look for postural hypotension (decreased BP or dizziness when altering posture, e.g. changing from lying to sitting), sweating disorder, and gastrointestinal problems such as constipation. An ECG can be done while the patient performs a Valsalva manoeuvre (involves trying to breathe out through a closed glottis) with particular attention paid to the RR variability. Sympathetic skin response and sweat tests may be requested. Optimisation may include increased salt intake, fludrocortisone and graded compression stockings or even IV fluids to increase plasma volume.
Chronic spinal cord lesions
After an initial period of flaccidity these patients suffer from spasticity and increased reflexes. Depression and phantom pain may complicate their perioperative care.
Autonomic dysreflexia can be a serious problem. Any stimulus (e.g. cutaneous, blocked bladder catheter or bowel distension) can trigger an acute sympathetic discharge. This may cause hypertension, flushing, headache and arrhythmias. If untreated it can cause myocardial ischaemia and strokes. Patients will often be aware that they have such symptoms and need to have any triggers minimised. Prevention of blocked catheters is vital. Renal problems are increased so function should be assessed with UandEs. Check PFTs. Patients with respiratory muscle weakness and difficulty coughing will require extra physiotherapy and maybe high dependancy unit (HDU) care including non-invasive ventilation. Preoperative blood gases may be required.
Spinals are frequently used in these cases to ablate visceral and peripheral stimuli. Avoid clexane within 6 hours of surgery. Incidence of latex allergy is increased.
Dementia
This may take the form of senile or presenile dementia (Alzheimer’s). Impaired memory is followed by impaired thought and speech and finally complete helplessness.
Written reminders about perioperative starvation and medications are useful in the early stages. To avoid overtaxing the patient, the number of people looking after them should be kept to a minimum. A close family member or carer may provide a more accurate medical and surgical history, including past response to drugs, and a current list of medications prescribed. They should be encouraged to remain with the patient prior to surgery to ensure compliance with preoperative instructions and with medication, perioperative starvation and fluid prescription. Postoperatively they will also help reorient and reassure the person with dementia emerging from anaesthesia. They may help to protect against falls and the accidental removal of catheters and intravenous lines.
The patient should be kept warm and well hydrated perioperatively because hypothermia and dehydration can contribute to postoperative confusion.
Anaesthesia can contribute to postoperative cognitive dysfunction (POCD). Unfortunately there is no evidence that regional anaesthesia protects from this state. This group of patients may have a delayed recovery from general anaesthesia and they are at greater risk of an acute confusional state.
Acute confusional state is seen frequently in hospitalised patients of any age, but particularly in geriatric patients with dementia. Clinically there is clouding of consciousness, memory impairment, impaired cognitive function, impaired perception, disturbance of emotion, and depression of psychomotor activity, but repetitive, stereotyped activity such as plucking at bedclothes or tossing from side to side may be seen.
Epilepsy
Find out about frequency of seizures, their type and pattern and any triggering factors (e.g. flashing lights, etc). A complete drug history is vital; some drugs such as phenytoin may necessitate plasma levels and further loading. The drugs can all be given (via nasogastric tube if necessary) even when a patient is fasting preoperatively. In patients with ongoing absorbtion problems, IV phenytoin or phenobarbitone can be used. Complications such as anaemia, thrombocytopenia and hyponatraemia and deranged liver function should be excluded with the appropriate blood tests. Most patients will benefit from a benzodiazepine premed.
Guillain Barré
Patients have a progressive weakness of more than one limb. This usually ascends symmetrically and is due to peripheral nerve demyelination. They must be assessed for bulbar problems and chronic aspiration. PFTs are essential since respiratory muscles are frequently affected. Dehydration and electrolyte abnormalities should be excluded with blood tests. Excessive sweating and postural hypotension may allude to autonomic dysfunction; an ECG is indicated. Invasive cardiovascular monitoring will usually be required. HDU facilities should be available postoperatively.
Motor neurone disease (MND)
This progressive disorder is due to degeneration of motor neurones in the brain and spinal cord. Symptoms include spastic limb weakness, atrophy of muscles with fasciculation and bulbar palsies (problems swallowing with risk of aspiration). Later on respiratory muscle weakness may lead to problems breathing and coughing. Specific tests of diaphragmatic function include mouth occlusion pressures and looking for a >30% decrease in vital capacity when lying flat. Ask about dyspnoea when lying flat. Most cases that are unsuitable for regional anaesthesia (preferred technique), should be prepared as for awake intubation including acid aspiration prophylaxis.
Multiple sclerosis (MS)
Inflammation of white matter in the central nervous system leads to what can be a progressive disorder characterised by optic neuritis, limb weakness, bladder and bowel dysfunction. Symptoms may relapse and remit and could include dysarthria, dysphagia, depression or cognitive decline. Patients may be on steroid medication. Symptoms of bulbar dysfunction with aspiration as well as evidence of relapse should be noted. Poor respiratory function may require PFTs and ABGs. There is no evidence that anaesthesia can precipitate a relapse of MS; however high concentrations of local anaesthetics, for example in epidurals, may cause a relapse. Severe demyelination of the spinal cord can lead to autonomic dysreflexia. This can result in a dangerous autonomic response (hypertension, bradycardia, flushing) to stimuli below the level of demyelination. The presence of contractures or pressure sores makes careful positioning essential. Treat pyrexia aggressively since it may cause a relapse.
Duchennes muscular dystrophy
This is a genetic condition in which patients have atrophy and weakness of muscles. Repeated aspirations and spinal deformities can restrict respiratory reserve even though PFTs may be normal. Look for tachypnoea with small Tidal Volume (Vt) and a paradoxical breathing pattern. There is an association with malignant hyperthermia so a review of previous anaesthetics is essential. They should all have PFTs, chest X-rays, blood gases, ECG and echo if there are any signs of cardiomyopathy. Risk of aspiration is attenuated by giving a proton pump inhibitor and full starvation for six hours. Make sure an HDU/ITU bed is available before undertaking surgery.
Dystrophia myotonica
This is an autosomal dominant condition which presents usually in the third decade. Involuntary continuation of muscle contractions occurs after stimulation. The condition is provoked by cold. Muscle weakness with atrophy is the main feature. Potassium supplements may make symptoms worse. Avoid hypothermia and shivering. Patients with this condition are prone to arrhythmias and aspiration.
Myaesthenia gravis (MG)
Antibodies to the acetyl choline receptor result in muscle weakness with fatigability. Take a careful drug history. Assess the gag reflex since bulbar involvement may result in chronic aspiration so preoperative physiotherapy may be helpful. PFTs and ABGs will give some idea as to the need for postoperative ITU or ventilation (e.g. VC < 2.9L). It is also increased if MG has been present for more than six years; this possibility needs to be discussed with the patient. Continue the anticholinesterase therapy (e.g. pyridostigmine) as long as possible. Some advocate a course of steroids preoperatively. MG is associated with thyroid disease as well as systemic lupus erythematosus (SLE) and pernicious anaemia. Patients may be immunosuppressed and prone to infection.
Muscle relaxants and neurological disease
With any systemic neurological disease, monitoring of the effect of muscle relaxation is mandatory. This is carried out using a Train of Four (ToF) monitor or more accurately using acceleromyography.
Table 9.3 lists a few conditions and the consequence of depolarising (e.g. suxamethonium) and non-depolarising (e.g. vecuronium) muscle relaxants.
Table 9.3 Muscle relaxants and neurological conditions
| Non-depolarising MR | Suxamethonium | |
| Myaesthenia gravis | May have increased sensitivity. Wide variation in dose requirements. | Resistance has been reported. 1.5mg/kg usually enough. Cholinesterase levels correlated with recovery time |
| Myotonia | May not guarantee relaxation or prevent myotonia. | Can lead to prolonged paralysis/contraction. Avoid. |
| Muscular dystrophy | May be prolonged. Electro-myography may not reflect respiratory muscle function. | Contraindicated. |
| Motor neurone disease | Small initial dose and monitor. | Avoid (K+ release). |
Suxamethonium may also cause potassium ion (K+) release (due to up-regulation of acetylcholine receptors) in patients after burns, those on prolonged bed rest, as well as those with spinal cord injury, major muscle denervation (e.g. Guillain Barré) or hemiparetic stroke. Some advocate caution in patients with MS and Charcot–Marie–Tooth syndrome.
Parkinson’s
Parkinson’s disease comprises a classical triad of resting tremor, muscle rigidity, and bradykinesia, with additional loss of postural reflexes. Parkinson’s occurs as the result of a loss of dopamine-producing nerve cells in the substantia nigra. This disrupts the normal passage of messages to the basal ganglia. With the depletion of dopamine, these parts of the brain which coordinate movement are unable to function normally.
It is the commonest movement disorder and affects 3% of people over 65 years. Patients may present for other surgery but may also now be admitted for neurosurgical treatment, which involves stereotactic deep brain stimulation.
Patients may have concurrent dementia or depression. Autonomic dysfunction (see above) necessitates an ECG since they have increased incidence of arrhythmias. A baseline chest X-ray is useful to exclude atelectasis. They may have excess salivation and may have more risk of aspiration with upper airway dysfunction. Consider placing a catheter. Great care must be taken with management of antiparkinsonian drugs. Try not to allow disruption. The ‘on-off’ timing of the symptoms may dictate timing of surgery. Try to keep the patient warm since they have impaired thermoregulation. These patients may be at increased risk of dementia and postoperative cognitive dysfunction (POCD). Avoid anti-dopaminergic drugs such as metoclopramide and droperidol.
Psychiatric disorders
Anxiety disorders: these patients need sympathetic care. All drugs can be continued perioperatively. Premedication with benzodiazepines or beta-blockers is useful.
Depression: ECG is indicated with tricyclic antidepressants. These patients may be at increased risk of urinary retention. Patients on monoamine oxidase inhibitors (MAOIs) should avoid foods containing tyramine (e.g. cheese).
Manic disorders: Patients taking lithium should have plasma lithium levels checked since there is a narrow therapeutic window. The ECG may also be affected, and UandEs are indicated to exclude electrolyte imbalance.
Schizophrenia: Drugs can cause extrapyramidal symptoms (e.g. dyskinesis similar to Parkinsonism). Check for postural hypotension.
Recreational drugs
Various chemical substances and drugs are increasingly used recreationally in social settings. Healthcare professionals must be aware of the increasing abuse of these drugs and be able to recognise and manage serious reactions.
MDMA (‘ecstasy’) increases the release of neurotransmitters. The desired effects are euphoria, a feeling of intimacy, altered visual perception, enhanced libido, and increased energy. The most common adverse effects are agitation, anxiety, tachycardia, and hypertension. More serious adverse effects include arrhythmias, hyperthermia, and rhabdomyolysis.
Flunitrazepam is a potent benzodiazepine. At higher doses, the drug can cause lack of muscle control and loss of consciousness. Other adverse effects are hypotension, dizziness, confusion, and occasional aggression.
Ketamine is a dissociative anaesthetic used primarily in veterinary practice. It may be injected, swallowed, snorted, or smoked. Ketamine interacts with the N-methyl-D-aspartate channel. Analgesic effects occur at lower doses and amnesic effects at higher doses. Cardiovascular and respiratory toxicity may occur, as well as confusion and delirium.
GHB is a naturally occurring fatty acid derivative of [gamma]-aminobutyric acid that was originally used as a dietary supplement. Increasing doses progressively produce amnesia, drowsiness, dizziness, euphoria, seizures, coma, and death.
CONCLUSION
This chapter has given an overview of assessment and care for the patient undergoing neurological surgery. For more detailed understanding, the further reading list below will give the reader a wider perspective. It is important to understand in perioperative care that neurological conditions are relatively common and can present challenges in their assessment and subsequent management. Neurosurgical perioperative care is a more specialised field where expert advice and experience is required in relatively minor cases.
FURTHER READING
Arun K. Gupta and Andrew C. Summors (2001). Notes in Neuroanaesthesia and Critical Care. London: Greenwich Medical Media.
Joanne V. Hickey (2003). Clinical Practice of Neurological and Neurosurgical Nursing 5th edn. Philadelphia: Lippincott Williams.
Mary Jane Evans (1995). Neurologic-Neurosurgical Nursing 2nd edn. Philadelphia: Springhouse.
B. Matta, D. Menon and J. Turner (2000). Textbook of Neuroanaesthesia and Critical Care. London: Greenwich Medical Media.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





