165 Potassium
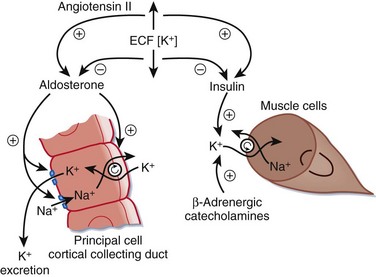
• Insulin enhances the activity of the sodium-potassium adenosine triphosphate pump, with a resultant decrease in extracellular potassium. Patients with diabetes mellitus are predisposed to hyperkalemia because of impaired insulin feedback and subsequently poor intracellular transfer of potassium.
• Asthmatic patients treated with bronchodilator therapy or epinephrine are predisposed to hypokalemia.
• Renal failure is responsible for the majority of cases of critical hyperkalemia seen in the emergency department.
• Calcium normalizes electrocardiographic manifestations of hyperkalemia within minutes of administration; however, the clinical effects are generally short-lived. Doses may need to be repeated within 30 minutes.
• Regular (short-acting) insulin administered as a 10-unit intravenous bolus will begin to lower serum potassium concentrations within 10 to 20 minutes, and the clinical effect lasts several hours. An ampule of 50% dextrose in water should be given concurrently to prevent hypoglycemia.
• Nebulized albuterol in 10- to 20-mg continuous treatments will transiently decrease serum potassium by 1 mEq/L over a 1- to 2-hour period.
• Definitive treatment of hyperkalemia is elimination of potassium. Hemodialysis is indicated for severe cases of hyperkalemia; when potassium-free dialysate is used, hemodialysis can reduce serum potassium by 1.5 mEq/hr.
Perspective
Potassium is the major intracellular cation and is closely regulated by the sodium-potassium adenosine triphosphatase (Na+,K+-ATPase) pump. Hypokalemia and hyperkalemia are electrolyte abnormalities common to both hospitalized and emergency department (ED) patients.1
Hypokalemia is observed more frequently than hyperkalemia and affects a broader range of patients; diuretic therapy accounts for as much as 80% of clinically significant cases seen in the ED.2 Hypokalemia is defined as a serum potassium level lower than 3.5 mEq/L. It is further classified as mild (3 to 3.5 mEq/L), moderate (2.5 to 2.9 mEq/L), and severe (<2.5 mEq/L).
Hyperkalemia, a disorder that affects patients with underlying renal insufficiency almost exclusively,1 is defined as a potassium level higher than 5.0 mEq/L. Hyperkalemia is further classified as mild (5 to 6 mEq/L), moderate (6.1 to 7 mEq/L), and severe (>7 mEq/L).
Both disorders can result in cardiac dysfunction, arrhythmia, and death.
Pathophysiology
Total body potassium (K+) is approximately 50 mEq/kg, or 3500 to 4000 mEq, in a normal-sized adult. For conversion purposes, 1 mEq of potassium is equivalent to 39.09 mg. Potassium is the major intracellular cation, and more than 98% of total body potassium is stored in the intracellular space. Intracellular fluid concentrations of potassium range from 150 to 160 mEq/L, with the highest amounts sequestered either in muscle (75%) or in bones and cartilage (8% to 10%).2
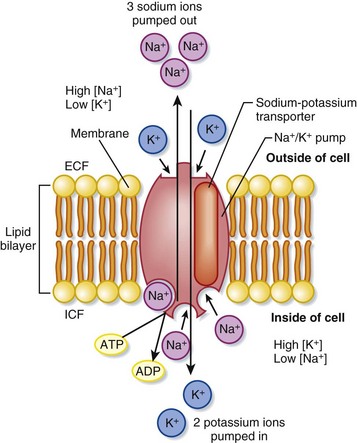
Extracellular potassium makes up less than 2% of total body stores, only two thirds of which is measurable in serum sampling. The normal range of plasma concentrations reported by most laboratory testing is 3.5 to 5 mEq/L; this small fraction is not reflective of total body potassium. Strict regulation of the ratio of intracellular to extracellular potassium (150 to 4 mEq/L) maintains a critical voltage gradient across cell membranes and plays a crucial role in establishing membrane potentials in cardiac and neuromuscular cells.1 The Na+,K+-ATPase transmembrane pump continuously maintains this gradient by actively transporting potassium into and sodium (Na+) out of cells1 (Fig. 165.1). Large changes in the intracellular potassium concentration have little effect on the ratio of intracellular to extracellular potassium. Conversely, even small changes in the extracellular concentration significantly affect this ratio, the transmembrane potential gradient, and the function of cardiac and neuromuscular tissue.1
All potassium disorders result from one of three disturbances3: impaired potassium intake, impaired distribution of potassium between the intracellular and extracellular spaces, and impaired renal excretion of potassium (Fig. 165.2).
Clinical Presentation
Hypokalemia
Approximately 20% of hospitalized patients are found to have subtherapeutic serum potassium levels.1 Despite this disease prevalence, most patients are asymptomatic, and only 5% of these patients have clinically significant hypokalemia.
In the outpatient setting, roughly 18% of patients have mild hypokalemia, which is generally asymptomatic. The vast majority of these cases (80%) are caused by potassium-wasting diuretic medications.2 Men and women are affected equally.
Box 165.1 summarizes the clinical findings of hypokalemia.
Box 165.1
Clinical Findings in Hypokalemia
Modified from Zull DN. Disorders of potassium metabolism. Emerg Med Clin North Am 1989;7:771–94.
Moderate Hypokalemia (2.5 to 2.9 mEq/L)
Muscular symptoms become more pronounced as the degree of hypokalemia worsens; the weakness is generalized, but proximal and lower extremity muscle groups are typically affected to a greater degree.2 Cardiac manifestations may include palpitations, non–life-threatening dysrhythmias (premature atrial contractions, premature ventricular contractions), and atrial fibrillation. Electrocardiographic (ECG) changes occur but do not correlate with the degree of hypokalemia (Box 165.2; Fig. 165.3).
Box 165.2
Electrocardiographic Abnormalities in Mild to Moderate Hypokalemia
Low, flattened, or inverted T waves
Potassium concentration usually less than 3.5 mEq/L
Decreased or depressed ST segment
Adapted from Cohn JN, Kowey PR, Whelton PK, et al. New guidelines for potassium replacement in clinical practice. Arch Intern Med 2000;160:2429–46; and Zull DN. Disorders of potassium metabolism. Emerg Med Clin North Am 1989;7:771–94.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree